Low Back Disorders
Evidence-Based Prevention and Rehabilitation
424 Pages
Low Back Disorders, Third Edition With Web Resource, guides readers through the assessment and treatment of low back pain, providing evidence-based research on the best methods of rehabilitation and prevention of future injury. In this book, internationally recognized low back specialist Stuart McGill presents the research and applications of back anatomy and biomechanics to build effective prevention and rehabilitation programs for patients or clients.
This third edition of Low Back Disorders contains all of the essential tools for those with low back maladies. Strong foundational information on anatomy and injury mechanisms guide readers through the essential functions of the structures of the low back and related tissues, and common misconceptions about pain and discomfort are addressed and corrected. The text provides detailed insights into injury assessment by an extensively expanded set of tests with accompanying instructions. These provide guidance and recommendations for individualized rehabilitation strategies and exercises. Also new to this edition is a web resource featuring 20 fillable Handouts for Patients or Clients that can be edited and printed to suit practitioner and patients’ needs. The web resource also contains an online video suite that showcases various exercises and assessments. In addition to offering strategies for relieving and potentially eliminating pain, the text provides insight into the conditions and environments that may initially cause back pain and makes recommendations on reducing these influences so that clients can be pain free.
This book contains more than 500 photos, graphs, and charts on anatomy, biomechanics, and assessments; 50 tests and exercises with step-by-step instructions are available to aid readers in developing successful programs for patients and clients. In addition to the evidence-based foundation of this edition, the following enhancements have been made:
• Completely updated information and streamlined chapter organization ensure that practitioners use best clinical practices.
• Practical checklists throughout the text provide easy access to testing and assessment clinical techniques and information.
• Practical Applications provide clinical information to aid readers in understanding concepts and theory.
• To aid instructors, the text includes a newly added image bank to visually support class lectures.
Low Back Disorders, Third Edition With Web Resource, contains essential research and corresponding clinical applications in a clear and organized format. Part I introduces the functional anatomy and biomechanics of the lumbar spine. It also presents epidemiological studies on low back disorders and dispels common myths of lumbar spine stability. Part II reviews risk factors for low back disorders and common prevention methods, with specific attention paid to reducing workplace risk factors. Part III explains evaluating and diagnosing clients and developing exercise and rehabilitation programs. Specific exercises that are proven to enhance performance and reduce pain are also explained.
Evidence-based research and cutting-edge application strategies from a leading spine specialist in North America make Low Back Disorders, Third Edition With Web Resource, the authoritative text for the examination and rehabilitation of the low back. Its approach to back care will lead readers in developing intervention, rehabilitation, and prevention programs to address the unique needs of each patient or client.
Earn continuing education credits/units! A continuing education course and exam that uses this book is also available. It may be purchased separately or as part of a package that includes all the course materials and exam.
Part I Scientific Foundation
Chapter 1. Introduction to the Issues and Scientific Approach Unique to This Book
Legislative Landscape: The Unfortunate Adverse Impact on Painful Backs
Deficiencies in Current Diagnostic Practices
Inadequacies in Current Care and Prevention
Mechanical Loading and the Process of Injury: A Low Back Tissue Injury Primer
Excellent Clinicians and Excellent Practice
Unique Scientific Foundation of This Book
In Vitro Lab
In Vivo Lab
A Final Note
Chapter 2. Epidemiological Studies and What They Really Mean
Influence of Randomized Controlled Trials and Other Epidemiological Approaches
Misunderstandings of Epidemiology
Multidimensional Links Among Biomechanical, Psychosocial, and Personal Variables
Are Biomechanical Variables and Psychosocial Variables Distinct?
How Do Biomechanical Factors Affect LBD?
Links Between Personal Factors and LBD
Studies of Exercise Intervention
Practical Application: What the Evidence Supports
What Works Clinically
A Final Note
Chapter 3. Functional Anatomy of the Lumbar Spine
Anatomy Trains
Basic Neural Structure
Vascular Anatomy
Vertebrae
Sacroiliac Joints
Intervertebral Disc
Muscles
Ligaments
Lumbodorsal Fascia (LDF)
Quick Review of the Pelvis, Hips, and Related Musculature
Clinically Relevant Aspects of Pain and Anatomic Structure
A Final Note
Chapter 4. Normal and Injury Mechanics of the Lumbar Spine
Kinematic Properties of the Thoracolumbar Spine
Kinetics and Normal Lumbar Spine Mechanics
Dubious Lifting Mechanisms
Other Important Mechanisms of Normal Spine Mechanics
Injury Mechanisms
Biomechanical and Physiological Changes Following Injury
A Final Note
Chapter 5. Myths and Realities of Lumbar Spine Stability
Why Spine Stability Is Important for Everyone
Stability: A Qualitative Analogy
Quantitative Foundation of Stability
Stability Myths, Facts, and Clinical Implications
A Final Note
Part II Injury Prevention
Chapter 6. LBD Risk Assessment
Brief Review of the Risk Factors for LBD
NIOSH Approach to Risk Assessment
Snook Psychophysical Approach
Lumbar Motion Monitor (LMM)
Ergowatch
Biological Signal–Driven Model Approaches
A Final Note
Chapter 7. Reducing the Risk of Low Back Injury
Lessons From the Literature
LBD Prevention for Workers
The Question of Back Belts
LBD Prevention for Employers
Injury Prevention Primer
A Note for Consultants
Reducing the Risk in Athletes
A Final Note
Part III Low Back Rehabilitation
Chapter 8. Building Better Rehabilitation Programs for Low Back Injuries
Pain-Reducing Mechanisms of Exercise
Five-Stage Back Training Program
Finding the Best Approach
Stages of Patient Progression
Guidelines for Developing the Best Exercise Regimen
A Final Note
Chapter 9. Evaluating the Patient
Most Crucial Element in Evaluation
First Clinician–Patient Meeting
Assessing Posture and Movement Quality
Some Provocation Tests
Some Functional Screens
Testing Muscle Endurance
A Final Note
Chapter 10. Developing the Exercise Program
Philosophy of Low Back Exercise Design
Clinical Wisdom
Thoughts on Mobility
Identifying Safe and Effective Exercises
Beginner’s Program for Pain Control and Stabilization
Exercises That May Be Used in a Stabilization Program
Special Conditions
A Final Note
Chapter 11. Advanced Exercises
Safely Increasing Challenges
Occupational and Athletic Work Hardening
A Final Note
Stuart McGill, PhD, is a professor at the University of Waterloo, Ontario, Canada, and a world-renowned lecturer and expert in spine function, injury prevention, and rehabilitation. He has written more than 300 scientific publications on lumbar function, mechanisms of low back injury, investigation of rehabilitation programs matched to specific categories of back pain patients, and the formulation of work-related injury avoidance strategies. He has received several awards for his work, including the Volvo Bioengineering Award for Low Back Pain Research from Sweden.
McGill has been an invited lecturer at many universities and delivered more than 300 addresses to societies around the world. As a consultant, he has provided expertise on assessment and reduction of the risk of low back injury to government agencies, corporations, professional athletes and teams, and legal firms. He is one of the few scientists who, in addition to performing research, is regularly requested by the medical profession to consult with challenging patients from around the world.
Postural tests for formal assessment
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit.
Formal Assessment of Posture
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit. Some tests are posturally based, whereas others assess control of motion.The following postural tests are very helpful. Recall that screening need not involve manipulation or special positions. Some of the most useful "tests" are simply intelligent observation.
Sitting Posture
Remarkably, patients with troubled backs often sit in a way that causes more back troubles. For example, patients who show flexion intolerance during provocative tests often have a typical sitting posture that involves a lot of spine flexion. In a similar way, those who show extension intolerance often sit with the spine locked into extension. The sitting posture is the first clue in hypothesis formation because this is often the posture that is first observed in the waiting area. Sitting in the waiting room in a flexed posture often suggests flexion intolerance.
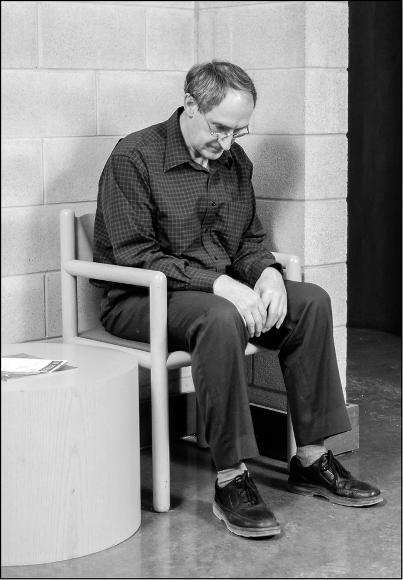
Photos from Stuart McGill
After noting the sitting posture, observe how the patient shifts from a slouched sitting posture to an upright one. Did she lift the rib cage, stressing the thoracolumbar junction ( a and b). Or did she flex the hips, rolling the pelvis forward to align the spine (c). Our recent work has shown that the best choice for most patients is to use a combination of the two (Castanhero et al., 2014) to minimize stress and avoid pain.
 |  |  |
Does the patient sit with a neutral spine (a) or a flexed spine (b)? When shifting from a slouch to a more upright posture, is the movement concentrated about the thoracolumbar junction or hips (c)?
Standing Pattern
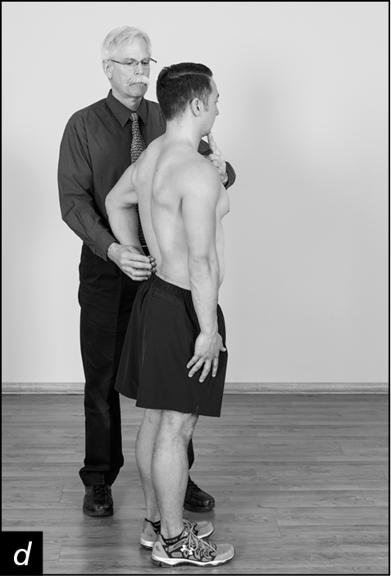
All sorts of clues are revealed in the standing posture. Simple palpation of the standing patient's lumbar extensor muscles will reveal whether the patient is chronically crushing the back with extensor contraction. Simple postural corrections such as extending the hip, retracting the shoulders posteriorly, and pulling in the chin can shut these muscles off.
 |  |  |
|
Teach patients to palpate the erectors at the L3 level, and learn where the switch point is between muscle activation and muscle relaxation. They do this by standing upright, head erect and shoulders back, and then leaning forward slightly (a). Then they perfect this strategy to relax the muscle. Teach them that chin poking (b) and shoulder slouching (c) activate the muscles that cause fatigue cramps. Have them try the hitchhiking thumb position as a correction strategy, externally rotating the arms about the shoulders and then letting the shoulders relax into this new position (d).Having patients palpate the lumbar erectors helps them learn self-correcting strategies - are the erectors silent or active (a)? If they are active, show the patient how to shut them off by unloading the spine, which often provides immediate relief of muscular pain. Cues include shifting the head and neck from a chin poke to chin retraction position, adopting a hitchhiking posture with external rotation of the arms and shoulders, and pulling the hips forward (b, c).
 |  |  |
No amount of muscle relaxants will shut off the painful back muscles if the patient stands in a slouched posture. Standing to spare the spine requires a finely tuned blend of postural adjustments and muscle activation patterns. One correction is to steer the thumbs in external rotation, retracting the shoulders (see b and c) to a spine-sparing, corrected posture.
Some patients stand with no measurable extensor or abdominal muscle activation - they simply balance on their passive elastic spine tissues. These people tend to have thick torsos with flaccid abdominal walls. For these patients, pain reduction can be achieved with mild abdominal contraction; 2 or 3% of maximal voluntary contraction is considered normal abdominal wall muscle tone during standing (Juker et al., 1998).
Lying Pattern
Stress during lying is a function of body shape, the lying surface, and the pain mechanism. For back sleepers with protruding buttocks, lying on a hard surface causes a bridge under the lumbar spine. This causes spine flexion as the back flattens to the mattress and pain in the flexion-intolerant back. This may be addressed with support such as a folded towel (a, b). In a similar fashion, wide hips cause full, and painful, spine lateral bend in side-lying. In this case, a pillow-top surface can provide relief.
 |
|
(a-b) Painful backs with lying and sleeping postures are usually relieved with support to foster a neutral posture. This support may be in the form of mattress selection (adjusting firmness and the thickness of the pillow-top) or buttressing devices such as a folded towel in a person whose spine is bridged with protruding buttocks (a). A pillow to support the neck and knees may assist with side lying (b).
Learn more about Low Back Disorders, Third Edition With Web Resource.
Treatment isn't a recipe from a cookbook: Strategies for individualizing rehabilitation
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
Finding the Best Approach
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
- Encourage patients to train for health versus performance. The notion that athletes are healthy is generally a myth, at least from a musculoskeletal point of view. Training for superior athletic performance demands substantial overload of the muscles and tissues of the joints. An elevated risk of injury is associated with athletic training and performance. Unfortunately, many patients observe the routines used by athletes to enhance performance and wrongly conclude that copying them will help their own backs. Training for health requires quite a different philosophy; it emphasizes muscle endurance, motor control perfection, and the maintenance of sufficient spine stability in all expected tasks. Although strength is not a goal, strength gains do result. If a patient with back pain states that his objective is to play tennis or golf, then he has the wrong short-term objective. First and foremost, the objective is to eliminate pain. Then the objective may shift toward a performance objective such as participation in a sporting activity.
- Integrate prevention and rehabilitation approaches.The best therapy rigorously followed will not produce results if the cause of the back troubles is not addressed. Part II provided guidelines for reducing the risk of back troubles: the importance of removing the cause of tissue overload cannot be overstressed. Linton and van Tulder (2001) demonstrated the efficacy of exercise for prevention; exercise satisfies the objective for both better prevention and better rehabilitation outcomes. First, teach patients what is causing their troubles; then work with them to eliminate the cause.
- Work toward a slow, continuous improvement in function and pain reduction. The return of function and the reduction of pain, particularly for those with chronic bad backs, is a slow process. The typical pattern of recovery is akin to that of the stock market. Daily, and even weekly, price fluctuations eventually result in higher prices. Patients have good days and bad days. Many times lawyers have hired private investigators to make clandestine videos of people with back troubles performing tasks that appear inconsistent with those troubles. I am hired to provide comment. Some of these people are true malingerers and get caught. Others are simply having a good day when they are video-recorded. In such cases, I see all sorts of movement pathology consistent with their chronic history, and they are exonerated.
- Have the patient keep a journal of daily activities. Sometimes it is difficult to hone in on the pain mechanism and the correct dosage and exercise form. Examining daily pain and activity patterns can help identify the link with mechanical scenarios that exacerbate the pain. Two critical components should be recorded in a daily journal: how the back feels and what tasks and activities were performed. When patients encounter repeated setbacks, they should try to identify a common task or activity that preceded the pain episode. Likewise, even when progress is slow, patients should be encouraged to see some progress nonetheless. Without referring to the diary, patients sometimes do not realize that they are improving. Linking pain with a dose of activity is different from recording pain on a 10-point scale, which is typical of behavior modification programs. I have seen too many patients from these programs obsessing over their pain levels; for these people, we suggest stopping pain recording.
- Ensure a positive slope in progress. Chapters 10 and 11introduce the big three exercises in different forms. We designed these exercises to spare the spine from large loads and to groove stabilizing motor patterns. Use the three to establish a positive slope in patient improvement. Once the slope is established, you may choose to add new exercises one at a time. The patient may tolerate some exercises well and others not so well. If the improvement slope is lost after adding a new activity, remove it, go back to the big three, and reestablish the positive slope. If the patient requires advanced exercises for athletic performance, perhaps to increase spine mobility, you may add exercises to achieve such objectives after establishing the positive slope. How long should each stage be? There is no single answer for everyone. Some progress quickly, whereas others require great patience. Your job is to determine the initial challenge, to gauge progress and enhance the challenge accordingly, and to keep the patient motivated, even during periods of no apparent progress. The great clinicians blend keen clinical skills and experience with scientifically founded guidelines and knowledge.
- Determine whether the patient is willing to make a change. Obviously, the patient must change the current patterns that caused her to become a back patient. This requires motivation, which is not always easy to establish. Some have listed the importance of, and steps for developing, a change in motivation and attitude (e.g., Ranney, 1997). Briefly, such a program begins with the setting of goals - for example, returning to a specific job or partaking in a leisure activity. The employer's role in enhancing motivation is to ensure that modified work is available together with the opportunity for a graduated return to duty. Employers can also enhance motivation by fostering a culture in which worker success equates to company success, which in turn helps the worker. The second step in a motivation program is to formulate a realistic plan for reaching the goal established in the first step. It is beyond the mandate of this book to develop the components of maintaining and enhancing motivational opportunities at each stage of recovery.
- Determine whether the patient needs initial mobilization. Although everyone should incorporate spine stabilization exercises into daily activity, a small group of people will benefit from some directed soft tissue work (e.g., manipulation, trigger point therapy, Active Release Techniques, the use of foam rollers). These techniques are not the focus of this book. A word of caution is required here. Too many make the mistake of trying to mobilize a painful spine region that already has mobility. Nonetheless, there is good evidence that those with documented hypomobility may benefit from some initial manipulation or mobilization with a transition into stabilization training (Fritz, Whitman, and Childs, 2005).
- Consider other soft tissue treatments. A good manual medicine clinician may perceive local muscle spasms and odd-feeling local muscle texture. Further, these spasms and local neurocompartment disorders are associated with larger dysfunctions of the agonist and synergist muscles involved in a movement. In many cases these dysfunctions delay recovery or prevent complete recovery. Clinicians use a variety of soft tissue treatments to reduce spasm and release tissues that can impede attaining more normal muscular and joint function. Documenting them is beyond the scope of this book. We simply alert you to their potential significance and role in rehabilitation.
- Avoid spine power. Spine power is the product of velocity and force (power = force × velocity). This means that the spine is bending quickly and there is velocity in the muscles' lengthening and shortening. Techniques that involve high velocity in the spine have been shown to lead to back troubles, because they usually indicate high power (Marras et al., 1993; Stevenson et al., 2001). To minimize power and maximize safety, the forces transmitted through the trunk must be low if the spine is moving. If the forces transmitted through the trunk are high, then the velocity must be low. The power must be generated at the hips and shoulders and transmitted through an isometrically stabilized torso. Fortunately, this fundamental tenet for safety also helps to maximize performance.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Five stages to reduce back pain through exercise
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood.
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood. However, many more exercise-induced analgesic pathways are coming to light. One example is that exercise increases neurotrophin-3 production, which appears to have an analgesic role in cutaneous and deep tissue pan (Sharma et al., 2010).
Psychological components are important for some patients and influence the approach used to introduce and program exercise. For example, some patients obsess over their pain and what is going on in their bodies. Patients with high fear avoidance do better with physical therapy, which de-emphasizes anatomical findings (George et al., 2003). For these types of patients, I suggest not using daily pain charts, but directing their focus to achieving good exercise form. Some patients have back pain because they overload themselves with daily regimens at the gym. For the type A personality, we ensure that exercise is not overexecuted (for people who believe that 25 repetitions of an exercise will do them more good than the 10 that were prescribed). For the type B personality who may bargain with the clinician about doing less exercise, performing the exercise dose as prescribed should be encouraged. These two personality types require different approaches to prescribing exercise.
Some people have pain as a result of tissues that are inappropriately weak for the applied demands. In such cases the goal of exercise is to strengthen tissue, which requires a certain kind of programming. Athletes I have worked with who have recovered well from compression fractures have incorporated sufficient rest intervals to allow the injury to adapt between loading sessions. This appears to not work with collagenous disc injuries given the time required (years) for migrated nucleus material to gristle and form a plug (Adams and Dolan, 2005). Thus, the type of tissue that is the target for strengthening should determine the exercise approach.
Imbalances in joint and muscle function create odd stress patterns and more pain. For example, hip and back pain can cause gluteal muscle inhibition (Freeman, Mascia, and McGill, 2013), which makes the hamstring muscles dominant in creating hip extension moment. Because of the lines of action of these muscles, this causes more load on the anterior acetabulum and labrum of the hip (Lewis, Sahrmann, and Moran, 2009), resulting in associated hip pain.
There is also substantial support for the notion of the existence of a psychological profile associated with fitness - that is, that fitter people ignore small discomforts. As discussed in the section Why and How You Should Read This Book, fitness reduces the tendency to catastrophize pain.
How is the most appropriate exercise determined to reduce each of these pain mechanisms? Although the assessment will reveal the pain mechanism, many challenging patients must be considered experiments in progress. Tweaking the exercise form and the dosage helps you to hone in on the optimal.
Five-Stage Back Training Program
We have developed a five-stage approach to back training that begins with identifying faulty movement patterns and ends with pain-free performance readiness. Consider this the big picture, because only athletes and people who perform demanding tasks will complete all five stages. However, it is important to understand the components and objectives of each stage, as well as their order. For example, patients may be unknowingly following a strengthening regimen (stage 4) without having addressed perturbed motion patterns (stage 1). Doing so will delay their recovery, or make them worse. So when approaching the program, you must first ask, Is the objective pain reduction and rehabilitation or athletic performance? Health objectives demand a focus on motion and motor patterns, stability, and endurance to achieve low tissue loads and a low-risk environment. Performance requires more overload, which naturally results in an elevated risk. The trick in the case of performance is to stay within the lowest risk possible.
Although all five major stages are listed here, only the first three are appropriate for rehabilitation and addressed in this book. Rigorous strength, speed, and power training are only for those interested in enhancing these attributes. The average person does not need them to have good back health. I address more advanced athletic training in detail in my book Ultimate Back Fitness and Performance (McGill, 2014). Begin with an assessment to understand the pain mechanisms. Then use the appropriate approach to address the mechanisms and build the person's tolerance and work capacity. Here is a summary of all five training stages:
- Stage 1: Establish quality movement engrams (motion patterns, motor patterns, and corrective exercise).
- Identify perturbed patterns and develop appropriate corrective exercise.
- Address basic movement patterns through to complex activity patterns.
- Address basic balance challenges through to complex and specific balance challenges.
- Stage 2: Build whole-body and joint stability (focus on spine stability here).
- Build stability while sparing the joints.
- Ensure sufficient stability commensurate with the demands of the task.
- Apply these patterns to the performance of daily activities.
- Stage 3: Increase endurance.
- Address basic endurance training to ensure the capacity needed for stabilization.
- Address activity-specific endurance (duration, intensity).
- Increase the ability to repeat pristine movement patterns without fatigue-induced compromise.
- Build the base for eventual performance training (only in those with this goal).
- Stage 4: Build strength.
- Spare the joints while maximizing the neuromuscular compartment challenge.
- Progress to skill movements.
- Stage 5: Develop speed, power, and agility.
- Develop ultimate performance based on the foundation laid in stages 1 through 4.
- Focus on optimizing elastic energy storage and recovery.
- Employ the techniques of superstiffness.
If you master the first three stages, which are discussed in this chapter, you will understand how to get bad backs to respond and how to develop better rehabilitation programs.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Models for measuring biological signals to assess risk
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Biological Signal - Driven Model Approaches
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Marras Model and McGill Model
The Marras model (Marras and Sommerich, 1991a, 1991b) measures electromyograms (EMGs) from several muscles and, using known physiological relationships, assigns forces to the muscles during virtually any industrial task. As noted earlier, this approach revealed powerful evidence linking the physical demands of specific occupational tasks with the incidence of LBD.
The McGill model (see chapter 1) uses the same philosophical approach to assign forces to the muscles, but attempts to include the highest level of anatomical accuracy possible. For example, it also measures three-dimensional spine curvature to assess forces to the passive tissues, including the intervertebral discs and the ligaments. By assigning forces to muscles and passive tissues throughout the full range of spine motion, it captures the ways people perform their jobs and even how they change with repetitions of the same jobs. The obvious liability of the approach is its enormous computational requirements, postprocessing of data, and difficulty collecting such comprehensive data from a wide number of workers in the field.
The question of the validity of this type of model must be addressed along with other models based on the biological approach. Some have argued that because these models contain known biomechanical and physiological relationships, they contain a certain amount of content validity. Moreover, both the Marras model and the McGill model have been quite successful in estimating the passive tissue and muscle forces that sum together to produce flexion and extension, lateral bend, and axial twisting moments. (These moments have been well predicted, with the exception of the twisting moment.) In summary, if twisting is not a dominant moment of force in a particular job, these models appear to predict accurate distributions of forces among the support tissues.
EMG-Assisted Optimization Approach
Perhaps the current pinnacle of model evolution is a hybrid modeling approach known as EMG-assisted optimization (developed by Cholewicki and McGill, 1994) with stability analysis and tissue load prediction (Cholewicki and McGill, 1996, was an early example, and Ikeda and McGill, 2012, is a more recent example). This approach exploits the asset of the biological EMG approach to distribute loads among the tissues based on the biological behavior of the subject. It then uses optimization to fine-tune the balancing of joint torques about several low back joints. The optimization takes the biologically predicted forces and adjusts muscle forces the minimal amount possible to satisfy the three-dimensional moment axes at every joint over the length of the lumbar spine. Once the three-dimensional moments have been assigned and tissue forces determined, an analysis of spine stability is performed via comparison of the joules of work imposed on the spine through perturbation with the joules of potential energy existing in the stiffened column.
This most highly evolved of spine models provides the biomechanist or ergonomist with insight into injury mechanisms caused by instability (as witnessed by Cholewicki and McGill, 1992) such as occurs while picking up a very light load from the floor. Even though patients have reported back injury from incidents such as bending over to tie a shoe, previous modeling approaches were sensitive only to tissue damage and injury scenarios produced from large loads and moments. Now a biomechanical explanation is available to explain the subsequent tissue damage, and a method is available to detect the risk of its happening. Although the routine use of this type of sophisticated model by ergonomists is not feasible, it is useful (for trained scientists) for analyzing individual workers and identifying those who are at elevated risk of injury because of faulty personal motor patterns.
Simple or Complex Models?
In summary, the complex models provide a tool to investigate the mechanisms of injury and the effects of technique during material handling on the risk of injury. The most complex and most highly evolved models provide insight into how injury occurs with all types of heavy and light loads. On the other hand, the simpler models, although sacrificing accuracy, can be powerful tools for the routine surveillance of physical demands in the workplace, but they must be wisely interpreted in each case given their limitations and constraints. Biomechanics and ergonomics require the full continuum of models. The choice of which one to use depends on the issue in question.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Postural tests for formal assessment
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit.
Formal Assessment of Posture
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit. Some tests are posturally based, whereas others assess control of motion.The following postural tests are very helpful. Recall that screening need not involve manipulation or special positions. Some of the most useful "tests" are simply intelligent observation.
Sitting Posture
Remarkably, patients with troubled backs often sit in a way that causes more back troubles. For example, patients who show flexion intolerance during provocative tests often have a typical sitting posture that involves a lot of spine flexion. In a similar way, those who show extension intolerance often sit with the spine locked into extension. The sitting posture is the first clue in hypothesis formation because this is often the posture that is first observed in the waiting area. Sitting in the waiting room in a flexed posture often suggests flexion intolerance.
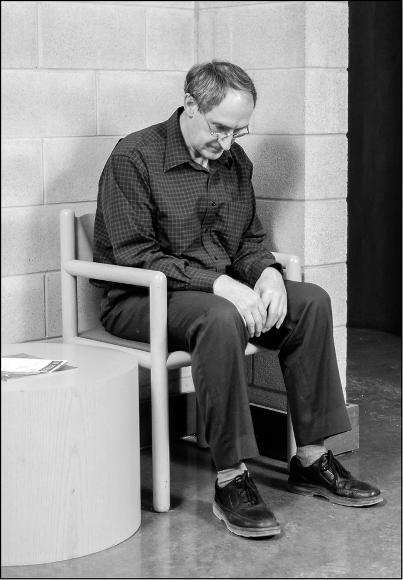
Photos from Stuart McGill
After noting the sitting posture, observe how the patient shifts from a slouched sitting posture to an upright one. Did she lift the rib cage, stressing the thoracolumbar junction ( a and b). Or did she flex the hips, rolling the pelvis forward to align the spine (c). Our recent work has shown that the best choice for most patients is to use a combination of the two (Castanhero et al., 2014) to minimize stress and avoid pain.
 |  |  |
Does the patient sit with a neutral spine (a) or a flexed spine (b)? When shifting from a slouch to a more upright posture, is the movement concentrated about the thoracolumbar junction or hips (c)?
Standing Pattern
All sorts of clues are revealed in the standing posture. Simple palpation of the standing patient's lumbar extensor muscles will reveal whether the patient is chronically crushing the back with extensor contraction. Simple postural corrections such as extending the hip, retracting the shoulders posteriorly, and pulling in the chin can shut these muscles off.
 |  |  |
|
Teach patients to palpate the erectors at the L3 level, and learn where the switch point is between muscle activation and muscle relaxation. They do this by standing upright, head erect and shoulders back, and then leaning forward slightly (a). Then they perfect this strategy to relax the muscle. Teach them that chin poking (b) and shoulder slouching (c) activate the muscles that cause fatigue cramps. Have them try the hitchhiking thumb position as a correction strategy, externally rotating the arms about the shoulders and then letting the shoulders relax into this new position (d).Having patients palpate the lumbar erectors helps them learn self-correcting strategies - are the erectors silent or active (a)? If they are active, show the patient how to shut them off by unloading the spine, which often provides immediate relief of muscular pain. Cues include shifting the head and neck from a chin poke to chin retraction position, adopting a hitchhiking posture with external rotation of the arms and shoulders, and pulling the hips forward (b, c).
 |  |  |
No amount of muscle relaxants will shut off the painful back muscles if the patient stands in a slouched posture. Standing to spare the spine requires a finely tuned blend of postural adjustments and muscle activation patterns. One correction is to steer the thumbs in external rotation, retracting the shoulders (see b and c) to a spine-sparing, corrected posture.
Some patients stand with no measurable extensor or abdominal muscle activation - they simply balance on their passive elastic spine tissues. These people tend to have thick torsos with flaccid abdominal walls. For these patients, pain reduction can be achieved with mild abdominal contraction; 2 or 3% of maximal voluntary contraction is considered normal abdominal wall muscle tone during standing (Juker et al., 1998).
Lying Pattern
Stress during lying is a function of body shape, the lying surface, and the pain mechanism. For back sleepers with protruding buttocks, lying on a hard surface causes a bridge under the lumbar spine. This causes spine flexion as the back flattens to the mattress and pain in the flexion-intolerant back. This may be addressed with support such as a folded towel (a, b). In a similar fashion, wide hips cause full, and painful, spine lateral bend in side-lying. In this case, a pillow-top surface can provide relief.
 |
|
(a-b) Painful backs with lying and sleeping postures are usually relieved with support to foster a neutral posture. This support may be in the form of mattress selection (adjusting firmness and the thickness of the pillow-top) or buttressing devices such as a folded towel in a person whose spine is bridged with protruding buttocks (a). A pillow to support the neck and knees may assist with side lying (b).
Learn more about Low Back Disorders, Third Edition With Web Resource.
Treatment isn't a recipe from a cookbook: Strategies for individualizing rehabilitation
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
Finding the Best Approach
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
- Encourage patients to train for health versus performance. The notion that athletes are healthy is generally a myth, at least from a musculoskeletal point of view. Training for superior athletic performance demands substantial overload of the muscles and tissues of the joints. An elevated risk of injury is associated with athletic training and performance. Unfortunately, many patients observe the routines used by athletes to enhance performance and wrongly conclude that copying them will help their own backs. Training for health requires quite a different philosophy; it emphasizes muscle endurance, motor control perfection, and the maintenance of sufficient spine stability in all expected tasks. Although strength is not a goal, strength gains do result. If a patient with back pain states that his objective is to play tennis or golf, then he has the wrong short-term objective. First and foremost, the objective is to eliminate pain. Then the objective may shift toward a performance objective such as participation in a sporting activity.
- Integrate prevention and rehabilitation approaches.The best therapy rigorously followed will not produce results if the cause of the back troubles is not addressed. Part II provided guidelines for reducing the risk of back troubles: the importance of removing the cause of tissue overload cannot be overstressed. Linton and van Tulder (2001) demonstrated the efficacy of exercise for prevention; exercise satisfies the objective for both better prevention and better rehabilitation outcomes. First, teach patients what is causing their troubles; then work with them to eliminate the cause.
- Work toward a slow, continuous improvement in function and pain reduction. The return of function and the reduction of pain, particularly for those with chronic bad backs, is a slow process. The typical pattern of recovery is akin to that of the stock market. Daily, and even weekly, price fluctuations eventually result in higher prices. Patients have good days and bad days. Many times lawyers have hired private investigators to make clandestine videos of people with back troubles performing tasks that appear inconsistent with those troubles. I am hired to provide comment. Some of these people are true malingerers and get caught. Others are simply having a good day when they are video-recorded. In such cases, I see all sorts of movement pathology consistent with their chronic history, and they are exonerated.
- Have the patient keep a journal of daily activities. Sometimes it is difficult to hone in on the pain mechanism and the correct dosage and exercise form. Examining daily pain and activity patterns can help identify the link with mechanical scenarios that exacerbate the pain. Two critical components should be recorded in a daily journal: how the back feels and what tasks and activities were performed. When patients encounter repeated setbacks, they should try to identify a common task or activity that preceded the pain episode. Likewise, even when progress is slow, patients should be encouraged to see some progress nonetheless. Without referring to the diary, patients sometimes do not realize that they are improving. Linking pain with a dose of activity is different from recording pain on a 10-point scale, which is typical of behavior modification programs. I have seen too many patients from these programs obsessing over their pain levels; for these people, we suggest stopping pain recording.
- Ensure a positive slope in progress. Chapters 10 and 11introduce the big three exercises in different forms. We designed these exercises to spare the spine from large loads and to groove stabilizing motor patterns. Use the three to establish a positive slope in patient improvement. Once the slope is established, you may choose to add new exercises one at a time. The patient may tolerate some exercises well and others not so well. If the improvement slope is lost after adding a new activity, remove it, go back to the big three, and reestablish the positive slope. If the patient requires advanced exercises for athletic performance, perhaps to increase spine mobility, you may add exercises to achieve such objectives after establishing the positive slope. How long should each stage be? There is no single answer for everyone. Some progress quickly, whereas others require great patience. Your job is to determine the initial challenge, to gauge progress and enhance the challenge accordingly, and to keep the patient motivated, even during periods of no apparent progress. The great clinicians blend keen clinical skills and experience with scientifically founded guidelines and knowledge.
- Determine whether the patient is willing to make a change. Obviously, the patient must change the current patterns that caused her to become a back patient. This requires motivation, which is not always easy to establish. Some have listed the importance of, and steps for developing, a change in motivation and attitude (e.g., Ranney, 1997). Briefly, such a program begins with the setting of goals - for example, returning to a specific job or partaking in a leisure activity. The employer's role in enhancing motivation is to ensure that modified work is available together with the opportunity for a graduated return to duty. Employers can also enhance motivation by fostering a culture in which worker success equates to company success, which in turn helps the worker. The second step in a motivation program is to formulate a realistic plan for reaching the goal established in the first step. It is beyond the mandate of this book to develop the components of maintaining and enhancing motivational opportunities at each stage of recovery.
- Determine whether the patient needs initial mobilization. Although everyone should incorporate spine stabilization exercises into daily activity, a small group of people will benefit from some directed soft tissue work (e.g., manipulation, trigger point therapy, Active Release Techniques, the use of foam rollers). These techniques are not the focus of this book. A word of caution is required here. Too many make the mistake of trying to mobilize a painful spine region that already has mobility. Nonetheless, there is good evidence that those with documented hypomobility may benefit from some initial manipulation or mobilization with a transition into stabilization training (Fritz, Whitman, and Childs, 2005).
- Consider other soft tissue treatments. A good manual medicine clinician may perceive local muscle spasms and odd-feeling local muscle texture. Further, these spasms and local neurocompartment disorders are associated with larger dysfunctions of the agonist and synergist muscles involved in a movement. In many cases these dysfunctions delay recovery or prevent complete recovery. Clinicians use a variety of soft tissue treatments to reduce spasm and release tissues that can impede attaining more normal muscular and joint function. Documenting them is beyond the scope of this book. We simply alert you to their potential significance and role in rehabilitation.
- Avoid spine power. Spine power is the product of velocity and force (power = force × velocity). This means that the spine is bending quickly and there is velocity in the muscles' lengthening and shortening. Techniques that involve high velocity in the spine have been shown to lead to back troubles, because they usually indicate high power (Marras et al., 1993; Stevenson et al., 2001). To minimize power and maximize safety, the forces transmitted through the trunk must be low if the spine is moving. If the forces transmitted through the trunk are high, then the velocity must be low. The power must be generated at the hips and shoulders and transmitted through an isometrically stabilized torso. Fortunately, this fundamental tenet for safety also helps to maximize performance.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Five stages to reduce back pain through exercise
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood.
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood. However, many more exercise-induced analgesic pathways are coming to light. One example is that exercise increases neurotrophin-3 production, which appears to have an analgesic role in cutaneous and deep tissue pan (Sharma et al., 2010).
Psychological components are important for some patients and influence the approach used to introduce and program exercise. For example, some patients obsess over their pain and what is going on in their bodies. Patients with high fear avoidance do better with physical therapy, which de-emphasizes anatomical findings (George et al., 2003). For these types of patients, I suggest not using daily pain charts, but directing their focus to achieving good exercise form. Some patients have back pain because they overload themselves with daily regimens at the gym. For the type A personality, we ensure that exercise is not overexecuted (for people who believe that 25 repetitions of an exercise will do them more good than the 10 that were prescribed). For the type B personality who may bargain with the clinician about doing less exercise, performing the exercise dose as prescribed should be encouraged. These two personality types require different approaches to prescribing exercise.
Some people have pain as a result of tissues that are inappropriately weak for the applied demands. In such cases the goal of exercise is to strengthen tissue, which requires a certain kind of programming. Athletes I have worked with who have recovered well from compression fractures have incorporated sufficient rest intervals to allow the injury to adapt between loading sessions. This appears to not work with collagenous disc injuries given the time required (years) for migrated nucleus material to gristle and form a plug (Adams and Dolan, 2005). Thus, the type of tissue that is the target for strengthening should determine the exercise approach.
Imbalances in joint and muscle function create odd stress patterns and more pain. For example, hip and back pain can cause gluteal muscle inhibition (Freeman, Mascia, and McGill, 2013), which makes the hamstring muscles dominant in creating hip extension moment. Because of the lines of action of these muscles, this causes more load on the anterior acetabulum and labrum of the hip (Lewis, Sahrmann, and Moran, 2009), resulting in associated hip pain.
There is also substantial support for the notion of the existence of a psychological profile associated with fitness - that is, that fitter people ignore small discomforts. As discussed in the section Why and How You Should Read This Book, fitness reduces the tendency to catastrophize pain.
How is the most appropriate exercise determined to reduce each of these pain mechanisms? Although the assessment will reveal the pain mechanism, many challenging patients must be considered experiments in progress. Tweaking the exercise form and the dosage helps you to hone in on the optimal.
Five-Stage Back Training Program
We have developed a five-stage approach to back training that begins with identifying faulty movement patterns and ends with pain-free performance readiness. Consider this the big picture, because only athletes and people who perform demanding tasks will complete all five stages. However, it is important to understand the components and objectives of each stage, as well as their order. For example, patients may be unknowingly following a strengthening regimen (stage 4) without having addressed perturbed motion patterns (stage 1). Doing so will delay their recovery, or make them worse. So when approaching the program, you must first ask, Is the objective pain reduction and rehabilitation or athletic performance? Health objectives demand a focus on motion and motor patterns, stability, and endurance to achieve low tissue loads and a low-risk environment. Performance requires more overload, which naturally results in an elevated risk. The trick in the case of performance is to stay within the lowest risk possible.
Although all five major stages are listed here, only the first three are appropriate for rehabilitation and addressed in this book. Rigorous strength, speed, and power training are only for those interested in enhancing these attributes. The average person does not need them to have good back health. I address more advanced athletic training in detail in my book Ultimate Back Fitness and Performance (McGill, 2014). Begin with an assessment to understand the pain mechanisms. Then use the appropriate approach to address the mechanisms and build the person's tolerance and work capacity. Here is a summary of all five training stages:
- Stage 1: Establish quality movement engrams (motion patterns, motor patterns, and corrective exercise).
- Identify perturbed patterns and develop appropriate corrective exercise.
- Address basic movement patterns through to complex activity patterns.
- Address basic balance challenges through to complex and specific balance challenges.
- Stage 2: Build whole-body and joint stability (focus on spine stability here).
- Build stability while sparing the joints.
- Ensure sufficient stability commensurate with the demands of the task.
- Apply these patterns to the performance of daily activities.
- Stage 3: Increase endurance.
- Address basic endurance training to ensure the capacity needed for stabilization.
- Address activity-specific endurance (duration, intensity).
- Increase the ability to repeat pristine movement patterns without fatigue-induced compromise.
- Build the base for eventual performance training (only in those with this goal).
- Stage 4: Build strength.
- Spare the joints while maximizing the neuromuscular compartment challenge.
- Progress to skill movements.
- Stage 5: Develop speed, power, and agility.
- Develop ultimate performance based on the foundation laid in stages 1 through 4.
- Focus on optimizing elastic energy storage and recovery.
- Employ the techniques of superstiffness.
If you master the first three stages, which are discussed in this chapter, you will understand how to get bad backs to respond and how to develop better rehabilitation programs.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Models for measuring biological signals to assess risk
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Biological Signal - Driven Model Approaches
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Marras Model and McGill Model
The Marras model (Marras and Sommerich, 1991a, 1991b) measures electromyograms (EMGs) from several muscles and, using known physiological relationships, assigns forces to the muscles during virtually any industrial task. As noted earlier, this approach revealed powerful evidence linking the physical demands of specific occupational tasks with the incidence of LBD.
The McGill model (see chapter 1) uses the same philosophical approach to assign forces to the muscles, but attempts to include the highest level of anatomical accuracy possible. For example, it also measures three-dimensional spine curvature to assess forces to the passive tissues, including the intervertebral discs and the ligaments. By assigning forces to muscles and passive tissues throughout the full range of spine motion, it captures the ways people perform their jobs and even how they change with repetitions of the same jobs. The obvious liability of the approach is its enormous computational requirements, postprocessing of data, and difficulty collecting such comprehensive data from a wide number of workers in the field.
The question of the validity of this type of model must be addressed along with other models based on the biological approach. Some have argued that because these models contain known biomechanical and physiological relationships, they contain a certain amount of content validity. Moreover, both the Marras model and the McGill model have been quite successful in estimating the passive tissue and muscle forces that sum together to produce flexion and extension, lateral bend, and axial twisting moments. (These moments have been well predicted, with the exception of the twisting moment.) In summary, if twisting is not a dominant moment of force in a particular job, these models appear to predict accurate distributions of forces among the support tissues.
EMG-Assisted Optimization Approach
Perhaps the current pinnacle of model evolution is a hybrid modeling approach known as EMG-assisted optimization (developed by Cholewicki and McGill, 1994) with stability analysis and tissue load prediction (Cholewicki and McGill, 1996, was an early example, and Ikeda and McGill, 2012, is a more recent example). This approach exploits the asset of the biological EMG approach to distribute loads among the tissues based on the biological behavior of the subject. It then uses optimization to fine-tune the balancing of joint torques about several low back joints. The optimization takes the biologically predicted forces and adjusts muscle forces the minimal amount possible to satisfy the three-dimensional moment axes at every joint over the length of the lumbar spine. Once the three-dimensional moments have been assigned and tissue forces determined, an analysis of spine stability is performed via comparison of the joules of work imposed on the spine through perturbation with the joules of potential energy existing in the stiffened column.
This most highly evolved of spine models provides the biomechanist or ergonomist with insight into injury mechanisms caused by instability (as witnessed by Cholewicki and McGill, 1992) such as occurs while picking up a very light load from the floor. Even though patients have reported back injury from incidents such as bending over to tie a shoe, previous modeling approaches were sensitive only to tissue damage and injury scenarios produced from large loads and moments. Now a biomechanical explanation is available to explain the subsequent tissue damage, and a method is available to detect the risk of its happening. Although the routine use of this type of sophisticated model by ergonomists is not feasible, it is useful (for trained scientists) for analyzing individual workers and identifying those who are at elevated risk of injury because of faulty personal motor patterns.
Simple or Complex Models?
In summary, the complex models provide a tool to investigate the mechanisms of injury and the effects of technique during material handling on the risk of injury. The most complex and most highly evolved models provide insight into how injury occurs with all types of heavy and light loads. On the other hand, the simpler models, although sacrificing accuracy, can be powerful tools for the routine surveillance of physical demands in the workplace, but they must be wisely interpreted in each case given their limitations and constraints. Biomechanics and ergonomics require the full continuum of models. The choice of which one to use depends on the issue in question.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Postural tests for formal assessment
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit.
Formal Assessment of Posture
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit. Some tests are posturally based, whereas others assess control of motion.The following postural tests are very helpful. Recall that screening need not involve manipulation or special positions. Some of the most useful "tests" are simply intelligent observation.
Sitting Posture
Remarkably, patients with troubled backs often sit in a way that causes more back troubles. For example, patients who show flexion intolerance during provocative tests often have a typical sitting posture that involves a lot of spine flexion. In a similar way, those who show extension intolerance often sit with the spine locked into extension. The sitting posture is the first clue in hypothesis formation because this is often the posture that is first observed in the waiting area. Sitting in the waiting room in a flexed posture often suggests flexion intolerance.
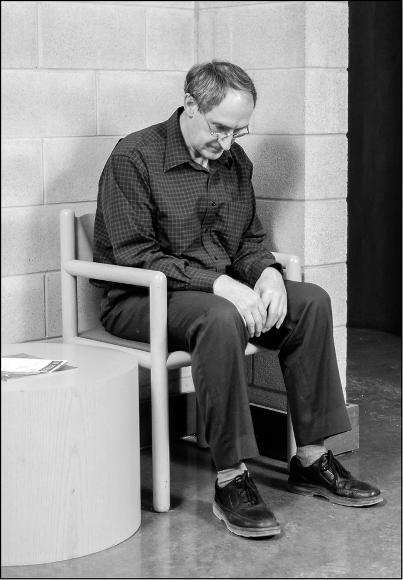
Photos from Stuart McGill
After noting the sitting posture, observe how the patient shifts from a slouched sitting posture to an upright one. Did she lift the rib cage, stressing the thoracolumbar junction ( a and b). Or did she flex the hips, rolling the pelvis forward to align the spine (c). Our recent work has shown that the best choice for most patients is to use a combination of the two (Castanhero et al., 2014) to minimize stress and avoid pain.
 |  |  |
Does the patient sit with a neutral spine (a) or a flexed spine (b)? When shifting from a slouch to a more upright posture, is the movement concentrated about the thoracolumbar junction or hips (c)?
Standing Pattern
All sorts of clues are revealed in the standing posture. Simple palpation of the standing patient's lumbar extensor muscles will reveal whether the patient is chronically crushing the back with extensor contraction. Simple postural corrections such as extending the hip, retracting the shoulders posteriorly, and pulling in the chin can shut these muscles off.
 |  |  |
|
Teach patients to palpate the erectors at the L3 level, and learn where the switch point is between muscle activation and muscle relaxation. They do this by standing upright, head erect and shoulders back, and then leaning forward slightly (a). Then they perfect this strategy to relax the muscle. Teach them that chin poking (b) and shoulder slouching (c) activate the muscles that cause fatigue cramps. Have them try the hitchhiking thumb position as a correction strategy, externally rotating the arms about the shoulders and then letting the shoulders relax into this new position (d).Having patients palpate the lumbar erectors helps them learn self-correcting strategies - are the erectors silent or active (a)? If they are active, show the patient how to shut them off by unloading the spine, which often provides immediate relief of muscular pain. Cues include shifting the head and neck from a chin poke to chin retraction position, adopting a hitchhiking posture with external rotation of the arms and shoulders, and pulling the hips forward (b, c).
 |  |  |
No amount of muscle relaxants will shut off the painful back muscles if the patient stands in a slouched posture. Standing to spare the spine requires a finely tuned blend of postural adjustments and muscle activation patterns. One correction is to steer the thumbs in external rotation, retracting the shoulders (see b and c) to a spine-sparing, corrected posture.
Some patients stand with no measurable extensor or abdominal muscle activation - they simply balance on their passive elastic spine tissues. These people tend to have thick torsos with flaccid abdominal walls. For these patients, pain reduction can be achieved with mild abdominal contraction; 2 or 3% of maximal voluntary contraction is considered normal abdominal wall muscle tone during standing (Juker et al., 1998).
Lying Pattern
Stress during lying is a function of body shape, the lying surface, and the pain mechanism. For back sleepers with protruding buttocks, lying on a hard surface causes a bridge under the lumbar spine. This causes spine flexion as the back flattens to the mattress and pain in the flexion-intolerant back. This may be addressed with support such as a folded towel (a, b). In a similar fashion, wide hips cause full, and painful, spine lateral bend in side-lying. In this case, a pillow-top surface can provide relief.
 |
|
(a-b) Painful backs with lying and sleeping postures are usually relieved with support to foster a neutral posture. This support may be in the form of mattress selection (adjusting firmness and the thickness of the pillow-top) or buttressing devices such as a folded towel in a person whose spine is bridged with protruding buttocks (a). A pillow to support the neck and knees may assist with side lying (b).
Learn more about Low Back Disorders, Third Edition With Web Resource.
Treatment isn't a recipe from a cookbook: Strategies for individualizing rehabilitation
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
Finding the Best Approach
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
- Encourage patients to train for health versus performance. The notion that athletes are healthy is generally a myth, at least from a musculoskeletal point of view. Training for superior athletic performance demands substantial overload of the muscles and tissues of the joints. An elevated risk of injury is associated with athletic training and performance. Unfortunately, many patients observe the routines used by athletes to enhance performance and wrongly conclude that copying them will help their own backs. Training for health requires quite a different philosophy; it emphasizes muscle endurance, motor control perfection, and the maintenance of sufficient spine stability in all expected tasks. Although strength is not a goal, strength gains do result. If a patient with back pain states that his objective is to play tennis or golf, then he has the wrong short-term objective. First and foremost, the objective is to eliminate pain. Then the objective may shift toward a performance objective such as participation in a sporting activity.
- Integrate prevention and rehabilitation approaches.The best therapy rigorously followed will not produce results if the cause of the back troubles is not addressed. Part II provided guidelines for reducing the risk of back troubles: the importance of removing the cause of tissue overload cannot be overstressed. Linton and van Tulder (2001) demonstrated the efficacy of exercise for prevention; exercise satisfies the objective for both better prevention and better rehabilitation outcomes. First, teach patients what is causing their troubles; then work with them to eliminate the cause.
- Work toward a slow, continuous improvement in function and pain reduction. The return of function and the reduction of pain, particularly for those with chronic bad backs, is a slow process. The typical pattern of recovery is akin to that of the stock market. Daily, and even weekly, price fluctuations eventually result in higher prices. Patients have good days and bad days. Many times lawyers have hired private investigators to make clandestine videos of people with back troubles performing tasks that appear inconsistent with those troubles. I am hired to provide comment. Some of these people are true malingerers and get caught. Others are simply having a good day when they are video-recorded. In such cases, I see all sorts of movement pathology consistent with their chronic history, and they are exonerated.
- Have the patient keep a journal of daily activities. Sometimes it is difficult to hone in on the pain mechanism and the correct dosage and exercise form. Examining daily pain and activity patterns can help identify the link with mechanical scenarios that exacerbate the pain. Two critical components should be recorded in a daily journal: how the back feels and what tasks and activities were performed. When patients encounter repeated setbacks, they should try to identify a common task or activity that preceded the pain episode. Likewise, even when progress is slow, patients should be encouraged to see some progress nonetheless. Without referring to the diary, patients sometimes do not realize that they are improving. Linking pain with a dose of activity is different from recording pain on a 10-point scale, which is typical of behavior modification programs. I have seen too many patients from these programs obsessing over their pain levels; for these people, we suggest stopping pain recording.
- Ensure a positive slope in progress. Chapters 10 and 11introduce the big three exercises in different forms. We designed these exercises to spare the spine from large loads and to groove stabilizing motor patterns. Use the three to establish a positive slope in patient improvement. Once the slope is established, you may choose to add new exercises one at a time. The patient may tolerate some exercises well and others not so well. If the improvement slope is lost after adding a new activity, remove it, go back to the big three, and reestablish the positive slope. If the patient requires advanced exercises for athletic performance, perhaps to increase spine mobility, you may add exercises to achieve such objectives after establishing the positive slope. How long should each stage be? There is no single answer for everyone. Some progress quickly, whereas others require great patience. Your job is to determine the initial challenge, to gauge progress and enhance the challenge accordingly, and to keep the patient motivated, even during periods of no apparent progress. The great clinicians blend keen clinical skills and experience with scientifically founded guidelines and knowledge.
- Determine whether the patient is willing to make a change. Obviously, the patient must change the current patterns that caused her to become a back patient. This requires motivation, which is not always easy to establish. Some have listed the importance of, and steps for developing, a change in motivation and attitude (e.g., Ranney, 1997). Briefly, such a program begins with the setting of goals - for example, returning to a specific job or partaking in a leisure activity. The employer's role in enhancing motivation is to ensure that modified work is available together with the opportunity for a graduated return to duty. Employers can also enhance motivation by fostering a culture in which worker success equates to company success, which in turn helps the worker. The second step in a motivation program is to formulate a realistic plan for reaching the goal established in the first step. It is beyond the mandate of this book to develop the components of maintaining and enhancing motivational opportunities at each stage of recovery.
- Determine whether the patient needs initial mobilization. Although everyone should incorporate spine stabilization exercises into daily activity, a small group of people will benefit from some directed soft tissue work (e.g., manipulation, trigger point therapy, Active Release Techniques, the use of foam rollers). These techniques are not the focus of this book. A word of caution is required here. Too many make the mistake of trying to mobilize a painful spine region that already has mobility. Nonetheless, there is good evidence that those with documented hypomobility may benefit from some initial manipulation or mobilization with a transition into stabilization training (Fritz, Whitman, and Childs, 2005).
- Consider other soft tissue treatments. A good manual medicine clinician may perceive local muscle spasms and odd-feeling local muscle texture. Further, these spasms and local neurocompartment disorders are associated with larger dysfunctions of the agonist and synergist muscles involved in a movement. In many cases these dysfunctions delay recovery or prevent complete recovery. Clinicians use a variety of soft tissue treatments to reduce spasm and release tissues that can impede attaining more normal muscular and joint function. Documenting them is beyond the scope of this book. We simply alert you to their potential significance and role in rehabilitation.
- Avoid spine power. Spine power is the product of velocity and force (power = force × velocity). This means that the spine is bending quickly and there is velocity in the muscles' lengthening and shortening. Techniques that involve high velocity in the spine have been shown to lead to back troubles, because they usually indicate high power (Marras et al., 1993; Stevenson et al., 2001). To minimize power and maximize safety, the forces transmitted through the trunk must be low if the spine is moving. If the forces transmitted through the trunk are high, then the velocity must be low. The power must be generated at the hips and shoulders and transmitted through an isometrically stabilized torso. Fortunately, this fundamental tenet for safety also helps to maximize performance.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Five stages to reduce back pain through exercise
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood.
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood. However, many more exercise-induced analgesic pathways are coming to light. One example is that exercise increases neurotrophin-3 production, which appears to have an analgesic role in cutaneous and deep tissue pan (Sharma et al., 2010).
Psychological components are important for some patients and influence the approach used to introduce and program exercise. For example, some patients obsess over their pain and what is going on in their bodies. Patients with high fear avoidance do better with physical therapy, which de-emphasizes anatomical findings (George et al., 2003). For these types of patients, I suggest not using daily pain charts, but directing their focus to achieving good exercise form. Some patients have back pain because they overload themselves with daily regimens at the gym. For the type A personality, we ensure that exercise is not overexecuted (for people who believe that 25 repetitions of an exercise will do them more good than the 10 that were prescribed). For the type B personality who may bargain with the clinician about doing less exercise, performing the exercise dose as prescribed should be encouraged. These two personality types require different approaches to prescribing exercise.
Some people have pain as a result of tissues that are inappropriately weak for the applied demands. In such cases the goal of exercise is to strengthen tissue, which requires a certain kind of programming. Athletes I have worked with who have recovered well from compression fractures have incorporated sufficient rest intervals to allow the injury to adapt between loading sessions. This appears to not work with collagenous disc injuries given the time required (years) for migrated nucleus material to gristle and form a plug (Adams and Dolan, 2005). Thus, the type of tissue that is the target for strengthening should determine the exercise approach.
Imbalances in joint and muscle function create odd stress patterns and more pain. For example, hip and back pain can cause gluteal muscle inhibition (Freeman, Mascia, and McGill, 2013), which makes the hamstring muscles dominant in creating hip extension moment. Because of the lines of action of these muscles, this causes more load on the anterior acetabulum and labrum of the hip (Lewis, Sahrmann, and Moran, 2009), resulting in associated hip pain.
There is also substantial support for the notion of the existence of a psychological profile associated with fitness - that is, that fitter people ignore small discomforts. As discussed in the section Why and How You Should Read This Book, fitness reduces the tendency to catastrophize pain.
How is the most appropriate exercise determined to reduce each of these pain mechanisms? Although the assessment will reveal the pain mechanism, many challenging patients must be considered experiments in progress. Tweaking the exercise form and the dosage helps you to hone in on the optimal.
Five-Stage Back Training Program
We have developed a five-stage approach to back training that begins with identifying faulty movement patterns and ends with pain-free performance readiness. Consider this the big picture, because only athletes and people who perform demanding tasks will complete all five stages. However, it is important to understand the components and objectives of each stage, as well as their order. For example, patients may be unknowingly following a strengthening regimen (stage 4) without having addressed perturbed motion patterns (stage 1). Doing so will delay their recovery, or make them worse. So when approaching the program, you must first ask, Is the objective pain reduction and rehabilitation or athletic performance? Health objectives demand a focus on motion and motor patterns, stability, and endurance to achieve low tissue loads and a low-risk environment. Performance requires more overload, which naturally results in an elevated risk. The trick in the case of performance is to stay within the lowest risk possible.
Although all five major stages are listed here, only the first three are appropriate for rehabilitation and addressed in this book. Rigorous strength, speed, and power training are only for those interested in enhancing these attributes. The average person does not need them to have good back health. I address more advanced athletic training in detail in my book Ultimate Back Fitness and Performance (McGill, 2014). Begin with an assessment to understand the pain mechanisms. Then use the appropriate approach to address the mechanisms and build the person's tolerance and work capacity. Here is a summary of all five training stages:
- Stage 1: Establish quality movement engrams (motion patterns, motor patterns, and corrective exercise).
- Identify perturbed patterns and develop appropriate corrective exercise.
- Address basic movement patterns through to complex activity patterns.
- Address basic balance challenges through to complex and specific balance challenges.
- Stage 2: Build whole-body and joint stability (focus on spine stability here).
- Build stability while sparing the joints.
- Ensure sufficient stability commensurate with the demands of the task.
- Apply these patterns to the performance of daily activities.
- Stage 3: Increase endurance.
- Address basic endurance training to ensure the capacity needed for stabilization.
- Address activity-specific endurance (duration, intensity).
- Increase the ability to repeat pristine movement patterns without fatigue-induced compromise.
- Build the base for eventual performance training (only in those with this goal).
- Stage 4: Build strength.
- Spare the joints while maximizing the neuromuscular compartment challenge.
- Progress to skill movements.
- Stage 5: Develop speed, power, and agility.
- Develop ultimate performance based on the foundation laid in stages 1 through 4.
- Focus on optimizing elastic energy storage and recovery.
- Employ the techniques of superstiffness.
If you master the first three stages, which are discussed in this chapter, you will understand how to get bad backs to respond and how to develop better rehabilitation programs.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Models for measuring biological signals to assess risk
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Biological Signal - Driven Model Approaches
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Marras Model and McGill Model
The Marras model (Marras and Sommerich, 1991a, 1991b) measures electromyograms (EMGs) from several muscles and, using known physiological relationships, assigns forces to the muscles during virtually any industrial task. As noted earlier, this approach revealed powerful evidence linking the physical demands of specific occupational tasks with the incidence of LBD.
The McGill model (see chapter 1) uses the same philosophical approach to assign forces to the muscles, but attempts to include the highest level of anatomical accuracy possible. For example, it also measures three-dimensional spine curvature to assess forces to the passive tissues, including the intervertebral discs and the ligaments. By assigning forces to muscles and passive tissues throughout the full range of spine motion, it captures the ways people perform their jobs and even how they change with repetitions of the same jobs. The obvious liability of the approach is its enormous computational requirements, postprocessing of data, and difficulty collecting such comprehensive data from a wide number of workers in the field.
The question of the validity of this type of model must be addressed along with other models based on the biological approach. Some have argued that because these models contain known biomechanical and physiological relationships, they contain a certain amount of content validity. Moreover, both the Marras model and the McGill model have been quite successful in estimating the passive tissue and muscle forces that sum together to produce flexion and extension, lateral bend, and axial twisting moments. (These moments have been well predicted, with the exception of the twisting moment.) In summary, if twisting is not a dominant moment of force in a particular job, these models appear to predict accurate distributions of forces among the support tissues.
EMG-Assisted Optimization Approach
Perhaps the current pinnacle of model evolution is a hybrid modeling approach known as EMG-assisted optimization (developed by Cholewicki and McGill, 1994) with stability analysis and tissue load prediction (Cholewicki and McGill, 1996, was an early example, and Ikeda and McGill, 2012, is a more recent example). This approach exploits the asset of the biological EMG approach to distribute loads among the tissues based on the biological behavior of the subject. It then uses optimization to fine-tune the balancing of joint torques about several low back joints. The optimization takes the biologically predicted forces and adjusts muscle forces the minimal amount possible to satisfy the three-dimensional moment axes at every joint over the length of the lumbar spine. Once the three-dimensional moments have been assigned and tissue forces determined, an analysis of spine stability is performed via comparison of the joules of work imposed on the spine through perturbation with the joules of potential energy existing in the stiffened column.
This most highly evolved of spine models provides the biomechanist or ergonomist with insight into injury mechanisms caused by instability (as witnessed by Cholewicki and McGill, 1992) such as occurs while picking up a very light load from the floor. Even though patients have reported back injury from incidents such as bending over to tie a shoe, previous modeling approaches were sensitive only to tissue damage and injury scenarios produced from large loads and moments. Now a biomechanical explanation is available to explain the subsequent tissue damage, and a method is available to detect the risk of its happening. Although the routine use of this type of sophisticated model by ergonomists is not feasible, it is useful (for trained scientists) for analyzing individual workers and identifying those who are at elevated risk of injury because of faulty personal motor patterns.
Simple or Complex Models?
In summary, the complex models provide a tool to investigate the mechanisms of injury and the effects of technique during material handling on the risk of injury. The most complex and most highly evolved models provide insight into how injury occurs with all types of heavy and light loads. On the other hand, the simpler models, although sacrificing accuracy, can be powerful tools for the routine surveillance of physical demands in the workplace, but they must be wisely interpreted in each case given their limitations and constraints. Biomechanics and ergonomics require the full continuum of models. The choice of which one to use depends on the issue in question.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Postural tests for formal assessment
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit.
Formal Assessment of Posture
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit. Some tests are posturally based, whereas others assess control of motion.The following postural tests are very helpful. Recall that screening need not involve manipulation or special positions. Some of the most useful "tests" are simply intelligent observation.
Sitting Posture
Remarkably, patients with troubled backs often sit in a way that causes more back troubles. For example, patients who show flexion intolerance during provocative tests often have a typical sitting posture that involves a lot of spine flexion. In a similar way, those who show extension intolerance often sit with the spine locked into extension. The sitting posture is the first clue in hypothesis formation because this is often the posture that is first observed in the waiting area. Sitting in the waiting room in a flexed posture often suggests flexion intolerance.
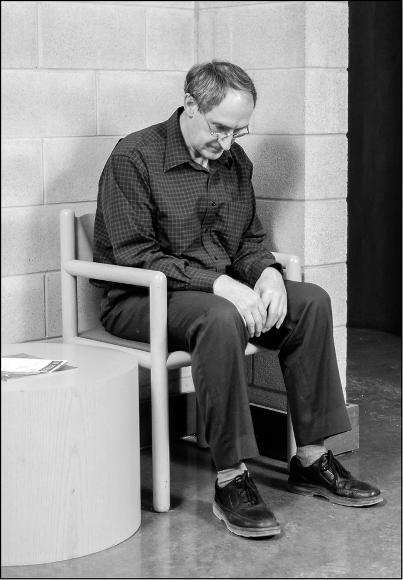
Photos from Stuart McGill
After noting the sitting posture, observe how the patient shifts from a slouched sitting posture to an upright one. Did she lift the rib cage, stressing the thoracolumbar junction ( a and b). Or did she flex the hips, rolling the pelvis forward to align the spine (c). Our recent work has shown that the best choice for most patients is to use a combination of the two (Castanhero et al., 2014) to minimize stress and avoid pain.
 |  |  |
Does the patient sit with a neutral spine (a) or a flexed spine (b)? When shifting from a slouch to a more upright posture, is the movement concentrated about the thoracolumbar junction or hips (c)?
Standing Pattern
All sorts of clues are revealed in the standing posture. Simple palpation of the standing patient's lumbar extensor muscles will reveal whether the patient is chronically crushing the back with extensor contraction. Simple postural corrections such as extending the hip, retracting the shoulders posteriorly, and pulling in the chin can shut these muscles off.
 |  |  |
|
Teach patients to palpate the erectors at the L3 level, and learn where the switch point is between muscle activation and muscle relaxation. They do this by standing upright, head erect and shoulders back, and then leaning forward slightly (a). Then they perfect this strategy to relax the muscle. Teach them that chin poking (b) and shoulder slouching (c) activate the muscles that cause fatigue cramps. Have them try the hitchhiking thumb position as a correction strategy, externally rotating the arms about the shoulders and then letting the shoulders relax into this new position (d).Having patients palpate the lumbar erectors helps them learn self-correcting strategies - are the erectors silent or active (a)? If they are active, show the patient how to shut them off by unloading the spine, which often provides immediate relief of muscular pain. Cues include shifting the head and neck from a chin poke to chin retraction position, adopting a hitchhiking posture with external rotation of the arms and shoulders, and pulling the hips forward (b, c).
 |  |  |
No amount of muscle relaxants will shut off the painful back muscles if the patient stands in a slouched posture. Standing to spare the spine requires a finely tuned blend of postural adjustments and muscle activation patterns. One correction is to steer the thumbs in external rotation, retracting the shoulders (see b and c) to a spine-sparing, corrected posture.
Some patients stand with no measurable extensor or abdominal muscle activation - they simply balance on their passive elastic spine tissues. These people tend to have thick torsos with flaccid abdominal walls. For these patients, pain reduction can be achieved with mild abdominal contraction; 2 or 3% of maximal voluntary contraction is considered normal abdominal wall muscle tone during standing (Juker et al., 1998).
Lying Pattern
Stress during lying is a function of body shape, the lying surface, and the pain mechanism. For back sleepers with protruding buttocks, lying on a hard surface causes a bridge under the lumbar spine. This causes spine flexion as the back flattens to the mattress and pain in the flexion-intolerant back. This may be addressed with support such as a folded towel (a, b). In a similar fashion, wide hips cause full, and painful, spine lateral bend in side-lying. In this case, a pillow-top surface can provide relief.
 |
|
(a-b) Painful backs with lying and sleeping postures are usually relieved with support to foster a neutral posture. This support may be in the form of mattress selection (adjusting firmness and the thickness of the pillow-top) or buttressing devices such as a folded towel in a person whose spine is bridged with protruding buttocks (a). A pillow to support the neck and knees may assist with side lying (b).
Learn more about Low Back Disorders, Third Edition With Web Resource.
Treatment isn't a recipe from a cookbook: Strategies for individualizing rehabilitation
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
Finding the Best Approach
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
- Encourage patients to train for health versus performance. The notion that athletes are healthy is generally a myth, at least from a musculoskeletal point of view. Training for superior athletic performance demands substantial overload of the muscles and tissues of the joints. An elevated risk of injury is associated with athletic training and performance. Unfortunately, many patients observe the routines used by athletes to enhance performance and wrongly conclude that copying them will help their own backs. Training for health requires quite a different philosophy; it emphasizes muscle endurance, motor control perfection, and the maintenance of sufficient spine stability in all expected tasks. Although strength is not a goal, strength gains do result. If a patient with back pain states that his objective is to play tennis or golf, then he has the wrong short-term objective. First and foremost, the objective is to eliminate pain. Then the objective may shift toward a performance objective such as participation in a sporting activity.
- Integrate prevention and rehabilitation approaches.The best therapy rigorously followed will not produce results if the cause of the back troubles is not addressed. Part II provided guidelines for reducing the risk of back troubles: the importance of removing the cause of tissue overload cannot be overstressed. Linton and van Tulder (2001) demonstrated the efficacy of exercise for prevention; exercise satisfies the objective for both better prevention and better rehabilitation outcomes. First, teach patients what is causing their troubles; then work with them to eliminate the cause.
- Work toward a slow, continuous improvement in function and pain reduction. The return of function and the reduction of pain, particularly for those with chronic bad backs, is a slow process. The typical pattern of recovery is akin to that of the stock market. Daily, and even weekly, price fluctuations eventually result in higher prices. Patients have good days and bad days. Many times lawyers have hired private investigators to make clandestine videos of people with back troubles performing tasks that appear inconsistent with those troubles. I am hired to provide comment. Some of these people are true malingerers and get caught. Others are simply having a good day when they are video-recorded. In such cases, I see all sorts of movement pathology consistent with their chronic history, and they are exonerated.
- Have the patient keep a journal of daily activities. Sometimes it is difficult to hone in on the pain mechanism and the correct dosage and exercise form. Examining daily pain and activity patterns can help identify the link with mechanical scenarios that exacerbate the pain. Two critical components should be recorded in a daily journal: how the back feels and what tasks and activities were performed. When patients encounter repeated setbacks, they should try to identify a common task or activity that preceded the pain episode. Likewise, even when progress is slow, patients should be encouraged to see some progress nonetheless. Without referring to the diary, patients sometimes do not realize that they are improving. Linking pain with a dose of activity is different from recording pain on a 10-point scale, which is typical of behavior modification programs. I have seen too many patients from these programs obsessing over their pain levels; for these people, we suggest stopping pain recording.
- Ensure a positive slope in progress. Chapters 10 and 11introduce the big three exercises in different forms. We designed these exercises to spare the spine from large loads and to groove stabilizing motor patterns. Use the three to establish a positive slope in patient improvement. Once the slope is established, you may choose to add new exercises one at a time. The patient may tolerate some exercises well and others not so well. If the improvement slope is lost after adding a new activity, remove it, go back to the big three, and reestablish the positive slope. If the patient requires advanced exercises for athletic performance, perhaps to increase spine mobility, you may add exercises to achieve such objectives after establishing the positive slope. How long should each stage be? There is no single answer for everyone. Some progress quickly, whereas others require great patience. Your job is to determine the initial challenge, to gauge progress and enhance the challenge accordingly, and to keep the patient motivated, even during periods of no apparent progress. The great clinicians blend keen clinical skills and experience with scientifically founded guidelines and knowledge.
- Determine whether the patient is willing to make a change. Obviously, the patient must change the current patterns that caused her to become a back patient. This requires motivation, which is not always easy to establish. Some have listed the importance of, and steps for developing, a change in motivation and attitude (e.g., Ranney, 1997). Briefly, such a program begins with the setting of goals - for example, returning to a specific job or partaking in a leisure activity. The employer's role in enhancing motivation is to ensure that modified work is available together with the opportunity for a graduated return to duty. Employers can also enhance motivation by fostering a culture in which worker success equates to company success, which in turn helps the worker. The second step in a motivation program is to formulate a realistic plan for reaching the goal established in the first step. It is beyond the mandate of this book to develop the components of maintaining and enhancing motivational opportunities at each stage of recovery.
- Determine whether the patient needs initial mobilization. Although everyone should incorporate spine stabilization exercises into daily activity, a small group of people will benefit from some directed soft tissue work (e.g., manipulation, trigger point therapy, Active Release Techniques, the use of foam rollers). These techniques are not the focus of this book. A word of caution is required here. Too many make the mistake of trying to mobilize a painful spine region that already has mobility. Nonetheless, there is good evidence that those with documented hypomobility may benefit from some initial manipulation or mobilization with a transition into stabilization training (Fritz, Whitman, and Childs, 2005).
- Consider other soft tissue treatments. A good manual medicine clinician may perceive local muscle spasms and odd-feeling local muscle texture. Further, these spasms and local neurocompartment disorders are associated with larger dysfunctions of the agonist and synergist muscles involved in a movement. In many cases these dysfunctions delay recovery or prevent complete recovery. Clinicians use a variety of soft tissue treatments to reduce spasm and release tissues that can impede attaining more normal muscular and joint function. Documenting them is beyond the scope of this book. We simply alert you to their potential significance and role in rehabilitation.
- Avoid spine power. Spine power is the product of velocity and force (power = force × velocity). This means that the spine is bending quickly and there is velocity in the muscles' lengthening and shortening. Techniques that involve high velocity in the spine have been shown to lead to back troubles, because they usually indicate high power (Marras et al., 1993; Stevenson et al., 2001). To minimize power and maximize safety, the forces transmitted through the trunk must be low if the spine is moving. If the forces transmitted through the trunk are high, then the velocity must be low. The power must be generated at the hips and shoulders and transmitted through an isometrically stabilized torso. Fortunately, this fundamental tenet for safety also helps to maximize performance.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Five stages to reduce back pain through exercise
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood.
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood. However, many more exercise-induced analgesic pathways are coming to light. One example is that exercise increases neurotrophin-3 production, which appears to have an analgesic role in cutaneous and deep tissue pan (Sharma et al., 2010).
Psychological components are important for some patients and influence the approach used to introduce and program exercise. For example, some patients obsess over their pain and what is going on in their bodies. Patients with high fear avoidance do better with physical therapy, which de-emphasizes anatomical findings (George et al., 2003). For these types of patients, I suggest not using daily pain charts, but directing their focus to achieving good exercise form. Some patients have back pain because they overload themselves with daily regimens at the gym. For the type A personality, we ensure that exercise is not overexecuted (for people who believe that 25 repetitions of an exercise will do them more good than the 10 that were prescribed). For the type B personality who may bargain with the clinician about doing less exercise, performing the exercise dose as prescribed should be encouraged. These two personality types require different approaches to prescribing exercise.
Some people have pain as a result of tissues that are inappropriately weak for the applied demands. In such cases the goal of exercise is to strengthen tissue, which requires a certain kind of programming. Athletes I have worked with who have recovered well from compression fractures have incorporated sufficient rest intervals to allow the injury to adapt between loading sessions. This appears to not work with collagenous disc injuries given the time required (years) for migrated nucleus material to gristle and form a plug (Adams and Dolan, 2005). Thus, the type of tissue that is the target for strengthening should determine the exercise approach.
Imbalances in joint and muscle function create odd stress patterns and more pain. For example, hip and back pain can cause gluteal muscle inhibition (Freeman, Mascia, and McGill, 2013), which makes the hamstring muscles dominant in creating hip extension moment. Because of the lines of action of these muscles, this causes more load on the anterior acetabulum and labrum of the hip (Lewis, Sahrmann, and Moran, 2009), resulting in associated hip pain.
There is also substantial support for the notion of the existence of a psychological profile associated with fitness - that is, that fitter people ignore small discomforts. As discussed in the section Why and How You Should Read This Book, fitness reduces the tendency to catastrophize pain.
How is the most appropriate exercise determined to reduce each of these pain mechanisms? Although the assessment will reveal the pain mechanism, many challenging patients must be considered experiments in progress. Tweaking the exercise form and the dosage helps you to hone in on the optimal.
Five-Stage Back Training Program
We have developed a five-stage approach to back training that begins with identifying faulty movement patterns and ends with pain-free performance readiness. Consider this the big picture, because only athletes and people who perform demanding tasks will complete all five stages. However, it is important to understand the components and objectives of each stage, as well as their order. For example, patients may be unknowingly following a strengthening regimen (stage 4) without having addressed perturbed motion patterns (stage 1). Doing so will delay their recovery, or make them worse. So when approaching the program, you must first ask, Is the objective pain reduction and rehabilitation or athletic performance? Health objectives demand a focus on motion and motor patterns, stability, and endurance to achieve low tissue loads and a low-risk environment. Performance requires more overload, which naturally results in an elevated risk. The trick in the case of performance is to stay within the lowest risk possible.
Although all five major stages are listed here, only the first three are appropriate for rehabilitation and addressed in this book. Rigorous strength, speed, and power training are only for those interested in enhancing these attributes. The average person does not need them to have good back health. I address more advanced athletic training in detail in my book Ultimate Back Fitness and Performance (McGill, 2014). Begin with an assessment to understand the pain mechanisms. Then use the appropriate approach to address the mechanisms and build the person's tolerance and work capacity. Here is a summary of all five training stages:
- Stage 1: Establish quality movement engrams (motion patterns, motor patterns, and corrective exercise).
- Identify perturbed patterns and develop appropriate corrective exercise.
- Address basic movement patterns through to complex activity patterns.
- Address basic balance challenges through to complex and specific balance challenges.
- Stage 2: Build whole-body and joint stability (focus on spine stability here).
- Build stability while sparing the joints.
- Ensure sufficient stability commensurate with the demands of the task.
- Apply these patterns to the performance of daily activities.
- Stage 3: Increase endurance.
- Address basic endurance training to ensure the capacity needed for stabilization.
- Address activity-specific endurance (duration, intensity).
- Increase the ability to repeat pristine movement patterns without fatigue-induced compromise.
- Build the base for eventual performance training (only in those with this goal).
- Stage 4: Build strength.
- Spare the joints while maximizing the neuromuscular compartment challenge.
- Progress to skill movements.
- Stage 5: Develop speed, power, and agility.
- Develop ultimate performance based on the foundation laid in stages 1 through 4.
- Focus on optimizing elastic energy storage and recovery.
- Employ the techniques of superstiffness.
If you master the first three stages, which are discussed in this chapter, you will understand how to get bad backs to respond and how to develop better rehabilitation programs.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Models for measuring biological signals to assess risk
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Biological Signal - Driven Model Approaches
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Marras Model and McGill Model
The Marras model (Marras and Sommerich, 1991a, 1991b) measures electromyograms (EMGs) from several muscles and, using known physiological relationships, assigns forces to the muscles during virtually any industrial task. As noted earlier, this approach revealed powerful evidence linking the physical demands of specific occupational tasks with the incidence of LBD.
The McGill model (see chapter 1) uses the same philosophical approach to assign forces to the muscles, but attempts to include the highest level of anatomical accuracy possible. For example, it also measures three-dimensional spine curvature to assess forces to the passive tissues, including the intervertebral discs and the ligaments. By assigning forces to muscles and passive tissues throughout the full range of spine motion, it captures the ways people perform their jobs and even how they change with repetitions of the same jobs. The obvious liability of the approach is its enormous computational requirements, postprocessing of data, and difficulty collecting such comprehensive data from a wide number of workers in the field.
The question of the validity of this type of model must be addressed along with other models based on the biological approach. Some have argued that because these models contain known biomechanical and physiological relationships, they contain a certain amount of content validity. Moreover, both the Marras model and the McGill model have been quite successful in estimating the passive tissue and muscle forces that sum together to produce flexion and extension, lateral bend, and axial twisting moments. (These moments have been well predicted, with the exception of the twisting moment.) In summary, if twisting is not a dominant moment of force in a particular job, these models appear to predict accurate distributions of forces among the support tissues.
EMG-Assisted Optimization Approach
Perhaps the current pinnacle of model evolution is a hybrid modeling approach known as EMG-assisted optimization (developed by Cholewicki and McGill, 1994) with stability analysis and tissue load prediction (Cholewicki and McGill, 1996, was an early example, and Ikeda and McGill, 2012, is a more recent example). This approach exploits the asset of the biological EMG approach to distribute loads among the tissues based on the biological behavior of the subject. It then uses optimization to fine-tune the balancing of joint torques about several low back joints. The optimization takes the biologically predicted forces and adjusts muscle forces the minimal amount possible to satisfy the three-dimensional moment axes at every joint over the length of the lumbar spine. Once the three-dimensional moments have been assigned and tissue forces determined, an analysis of spine stability is performed via comparison of the joules of work imposed on the spine through perturbation with the joules of potential energy existing in the stiffened column.
This most highly evolved of spine models provides the biomechanist or ergonomist with insight into injury mechanisms caused by instability (as witnessed by Cholewicki and McGill, 1992) such as occurs while picking up a very light load from the floor. Even though patients have reported back injury from incidents such as bending over to tie a shoe, previous modeling approaches were sensitive only to tissue damage and injury scenarios produced from large loads and moments. Now a biomechanical explanation is available to explain the subsequent tissue damage, and a method is available to detect the risk of its happening. Although the routine use of this type of sophisticated model by ergonomists is not feasible, it is useful (for trained scientists) for analyzing individual workers and identifying those who are at elevated risk of injury because of faulty personal motor patterns.
Simple or Complex Models?
In summary, the complex models provide a tool to investigate the mechanisms of injury and the effects of technique during material handling on the risk of injury. The most complex and most highly evolved models provide insight into how injury occurs with all types of heavy and light loads. On the other hand, the simpler models, although sacrificing accuracy, can be powerful tools for the routine surveillance of physical demands in the workplace, but they must be wisely interpreted in each case given their limitations and constraints. Biomechanics and ergonomics require the full continuum of models. The choice of which one to use depends on the issue in question.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Postural tests for formal assessment
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit.
Formal Assessment of Posture
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit. Some tests are posturally based, whereas others assess control of motion.The following postural tests are very helpful. Recall that screening need not involve manipulation or special positions. Some of the most useful "tests" are simply intelligent observation.
Sitting Posture
Remarkably, patients with troubled backs often sit in a way that causes more back troubles. For example, patients who show flexion intolerance during provocative tests often have a typical sitting posture that involves a lot of spine flexion. In a similar way, those who show extension intolerance often sit with the spine locked into extension. The sitting posture is the first clue in hypothesis formation because this is often the posture that is first observed in the waiting area. Sitting in the waiting room in a flexed posture often suggests flexion intolerance.
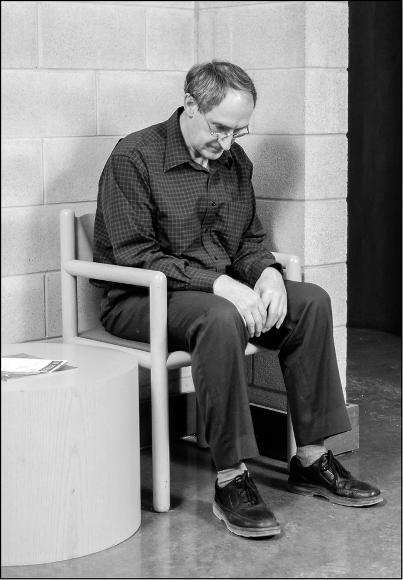
Photos from Stuart McGill
After noting the sitting posture, observe how the patient shifts from a slouched sitting posture to an upright one. Did she lift the rib cage, stressing the thoracolumbar junction ( a and b). Or did she flex the hips, rolling the pelvis forward to align the spine (c). Our recent work has shown that the best choice for most patients is to use a combination of the two (Castanhero et al., 2014) to minimize stress and avoid pain.
 |  |  |
Does the patient sit with a neutral spine (a) or a flexed spine (b)? When shifting from a slouch to a more upright posture, is the movement concentrated about the thoracolumbar junction or hips (c)?
Standing Pattern
All sorts of clues are revealed in the standing posture. Simple palpation of the standing patient's lumbar extensor muscles will reveal whether the patient is chronically crushing the back with extensor contraction. Simple postural corrections such as extending the hip, retracting the shoulders posteriorly, and pulling in the chin can shut these muscles off.
 |  |  |
|
Teach patients to palpate the erectors at the L3 level, and learn where the switch point is between muscle activation and muscle relaxation. They do this by standing upright, head erect and shoulders back, and then leaning forward slightly (a). Then they perfect this strategy to relax the muscle. Teach them that chin poking (b) and shoulder slouching (c) activate the muscles that cause fatigue cramps. Have them try the hitchhiking thumb position as a correction strategy, externally rotating the arms about the shoulders and then letting the shoulders relax into this new position (d).Having patients palpate the lumbar erectors helps them learn self-correcting strategies - are the erectors silent or active (a)? If they are active, show the patient how to shut them off by unloading the spine, which often provides immediate relief of muscular pain. Cues include shifting the head and neck from a chin poke to chin retraction position, adopting a hitchhiking posture with external rotation of the arms and shoulders, and pulling the hips forward (b, c).
 |  |  |
No amount of muscle relaxants will shut off the painful back muscles if the patient stands in a slouched posture. Standing to spare the spine requires a finely tuned blend of postural adjustments and muscle activation patterns. One correction is to steer the thumbs in external rotation, retracting the shoulders (see b and c) to a spine-sparing, corrected posture.
Some patients stand with no measurable extensor or abdominal muscle activation - they simply balance on their passive elastic spine tissues. These people tend to have thick torsos with flaccid abdominal walls. For these patients, pain reduction can be achieved with mild abdominal contraction; 2 or 3% of maximal voluntary contraction is considered normal abdominal wall muscle tone during standing (Juker et al., 1998).
Lying Pattern
Stress during lying is a function of body shape, the lying surface, and the pain mechanism. For back sleepers with protruding buttocks, lying on a hard surface causes a bridge under the lumbar spine. This causes spine flexion as the back flattens to the mattress and pain in the flexion-intolerant back. This may be addressed with support such as a folded towel (a, b). In a similar fashion, wide hips cause full, and painful, spine lateral bend in side-lying. In this case, a pillow-top surface can provide relief.
 |
|
(a-b) Painful backs with lying and sleeping postures are usually relieved with support to foster a neutral posture. This support may be in the form of mattress selection (adjusting firmness and the thickness of the pillow-top) or buttressing devices such as a folded towel in a person whose spine is bridged with protruding buttocks (a). A pillow to support the neck and knees may assist with side lying (b).
Learn more about Low Back Disorders, Third Edition With Web Resource.
Treatment isn't a recipe from a cookbook: Strategies for individualizing rehabilitation
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
Finding the Best Approach
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
- Encourage patients to train for health versus performance. The notion that athletes are healthy is generally a myth, at least from a musculoskeletal point of view. Training for superior athletic performance demands substantial overload of the muscles and tissues of the joints. An elevated risk of injury is associated with athletic training and performance. Unfortunately, many patients observe the routines used by athletes to enhance performance and wrongly conclude that copying them will help their own backs. Training for health requires quite a different philosophy; it emphasizes muscle endurance, motor control perfection, and the maintenance of sufficient spine stability in all expected tasks. Although strength is not a goal, strength gains do result. If a patient with back pain states that his objective is to play tennis or golf, then he has the wrong short-term objective. First and foremost, the objective is to eliminate pain. Then the objective may shift toward a performance objective such as participation in a sporting activity.
- Integrate prevention and rehabilitation approaches.The best therapy rigorously followed will not produce results if the cause of the back troubles is not addressed. Part II provided guidelines for reducing the risk of back troubles: the importance of removing the cause of tissue overload cannot be overstressed. Linton and van Tulder (2001) demonstrated the efficacy of exercise for prevention; exercise satisfies the objective for both better prevention and better rehabilitation outcomes. First, teach patients what is causing their troubles; then work with them to eliminate the cause.
- Work toward a slow, continuous improvement in function and pain reduction. The return of function and the reduction of pain, particularly for those with chronic bad backs, is a slow process. The typical pattern of recovery is akin to that of the stock market. Daily, and even weekly, price fluctuations eventually result in higher prices. Patients have good days and bad days. Many times lawyers have hired private investigators to make clandestine videos of people with back troubles performing tasks that appear inconsistent with those troubles. I am hired to provide comment. Some of these people are true malingerers and get caught. Others are simply having a good day when they are video-recorded. In such cases, I see all sorts of movement pathology consistent with their chronic history, and they are exonerated.
- Have the patient keep a journal of daily activities. Sometimes it is difficult to hone in on the pain mechanism and the correct dosage and exercise form. Examining daily pain and activity patterns can help identify the link with mechanical scenarios that exacerbate the pain. Two critical components should be recorded in a daily journal: how the back feels and what tasks and activities were performed. When patients encounter repeated setbacks, they should try to identify a common task or activity that preceded the pain episode. Likewise, even when progress is slow, patients should be encouraged to see some progress nonetheless. Without referring to the diary, patients sometimes do not realize that they are improving. Linking pain with a dose of activity is different from recording pain on a 10-point scale, which is typical of behavior modification programs. I have seen too many patients from these programs obsessing over their pain levels; for these people, we suggest stopping pain recording.
- Ensure a positive slope in progress. Chapters 10 and 11introduce the big three exercises in different forms. We designed these exercises to spare the spine from large loads and to groove stabilizing motor patterns. Use the three to establish a positive slope in patient improvement. Once the slope is established, you may choose to add new exercises one at a time. The patient may tolerate some exercises well and others not so well. If the improvement slope is lost after adding a new activity, remove it, go back to the big three, and reestablish the positive slope. If the patient requires advanced exercises for athletic performance, perhaps to increase spine mobility, you may add exercises to achieve such objectives after establishing the positive slope. How long should each stage be? There is no single answer for everyone. Some progress quickly, whereas others require great patience. Your job is to determine the initial challenge, to gauge progress and enhance the challenge accordingly, and to keep the patient motivated, even during periods of no apparent progress. The great clinicians blend keen clinical skills and experience with scientifically founded guidelines and knowledge.
- Determine whether the patient is willing to make a change. Obviously, the patient must change the current patterns that caused her to become a back patient. This requires motivation, which is not always easy to establish. Some have listed the importance of, and steps for developing, a change in motivation and attitude (e.g., Ranney, 1997). Briefly, such a program begins with the setting of goals - for example, returning to a specific job or partaking in a leisure activity. The employer's role in enhancing motivation is to ensure that modified work is available together with the opportunity for a graduated return to duty. Employers can also enhance motivation by fostering a culture in which worker success equates to company success, which in turn helps the worker. The second step in a motivation program is to formulate a realistic plan for reaching the goal established in the first step. It is beyond the mandate of this book to develop the components of maintaining and enhancing motivational opportunities at each stage of recovery.
- Determine whether the patient needs initial mobilization. Although everyone should incorporate spine stabilization exercises into daily activity, a small group of people will benefit from some directed soft tissue work (e.g., manipulation, trigger point therapy, Active Release Techniques, the use of foam rollers). These techniques are not the focus of this book. A word of caution is required here. Too many make the mistake of trying to mobilize a painful spine region that already has mobility. Nonetheless, there is good evidence that those with documented hypomobility may benefit from some initial manipulation or mobilization with a transition into stabilization training (Fritz, Whitman, and Childs, 2005).
- Consider other soft tissue treatments. A good manual medicine clinician may perceive local muscle spasms and odd-feeling local muscle texture. Further, these spasms and local neurocompartment disorders are associated with larger dysfunctions of the agonist and synergist muscles involved in a movement. In many cases these dysfunctions delay recovery or prevent complete recovery. Clinicians use a variety of soft tissue treatments to reduce spasm and release tissues that can impede attaining more normal muscular and joint function. Documenting them is beyond the scope of this book. We simply alert you to their potential significance and role in rehabilitation.
- Avoid spine power. Spine power is the product of velocity and force (power = force × velocity). This means that the spine is bending quickly and there is velocity in the muscles' lengthening and shortening. Techniques that involve high velocity in the spine have been shown to lead to back troubles, because they usually indicate high power (Marras et al., 1993; Stevenson et al., 2001). To minimize power and maximize safety, the forces transmitted through the trunk must be low if the spine is moving. If the forces transmitted through the trunk are high, then the velocity must be low. The power must be generated at the hips and shoulders and transmitted through an isometrically stabilized torso. Fortunately, this fundamental tenet for safety also helps to maximize performance.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Five stages to reduce back pain through exercise
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood.
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood. However, many more exercise-induced analgesic pathways are coming to light. One example is that exercise increases neurotrophin-3 production, which appears to have an analgesic role in cutaneous and deep tissue pan (Sharma et al., 2010).
Psychological components are important for some patients and influence the approach used to introduce and program exercise. For example, some patients obsess over their pain and what is going on in their bodies. Patients with high fear avoidance do better with physical therapy, which de-emphasizes anatomical findings (George et al., 2003). For these types of patients, I suggest not using daily pain charts, but directing their focus to achieving good exercise form. Some patients have back pain because they overload themselves with daily regimens at the gym. For the type A personality, we ensure that exercise is not overexecuted (for people who believe that 25 repetitions of an exercise will do them more good than the 10 that were prescribed). For the type B personality who may bargain with the clinician about doing less exercise, performing the exercise dose as prescribed should be encouraged. These two personality types require different approaches to prescribing exercise.
Some people have pain as a result of tissues that are inappropriately weak for the applied demands. In such cases the goal of exercise is to strengthen tissue, which requires a certain kind of programming. Athletes I have worked with who have recovered well from compression fractures have incorporated sufficient rest intervals to allow the injury to adapt between loading sessions. This appears to not work with collagenous disc injuries given the time required (years) for migrated nucleus material to gristle and form a plug (Adams and Dolan, 2005). Thus, the type of tissue that is the target for strengthening should determine the exercise approach.
Imbalances in joint and muscle function create odd stress patterns and more pain. For example, hip and back pain can cause gluteal muscle inhibition (Freeman, Mascia, and McGill, 2013), which makes the hamstring muscles dominant in creating hip extension moment. Because of the lines of action of these muscles, this causes more load on the anterior acetabulum and labrum of the hip (Lewis, Sahrmann, and Moran, 2009), resulting in associated hip pain.
There is also substantial support for the notion of the existence of a psychological profile associated with fitness - that is, that fitter people ignore small discomforts. As discussed in the section Why and How You Should Read This Book, fitness reduces the tendency to catastrophize pain.
How is the most appropriate exercise determined to reduce each of these pain mechanisms? Although the assessment will reveal the pain mechanism, many challenging patients must be considered experiments in progress. Tweaking the exercise form and the dosage helps you to hone in on the optimal.
Five-Stage Back Training Program
We have developed a five-stage approach to back training that begins with identifying faulty movement patterns and ends with pain-free performance readiness. Consider this the big picture, because only athletes and people who perform demanding tasks will complete all five stages. However, it is important to understand the components and objectives of each stage, as well as their order. For example, patients may be unknowingly following a strengthening regimen (stage 4) without having addressed perturbed motion patterns (stage 1). Doing so will delay their recovery, or make them worse. So when approaching the program, you must first ask, Is the objective pain reduction and rehabilitation or athletic performance? Health objectives demand a focus on motion and motor patterns, stability, and endurance to achieve low tissue loads and a low-risk environment. Performance requires more overload, which naturally results in an elevated risk. The trick in the case of performance is to stay within the lowest risk possible.
Although all five major stages are listed here, only the first three are appropriate for rehabilitation and addressed in this book. Rigorous strength, speed, and power training are only for those interested in enhancing these attributes. The average person does not need them to have good back health. I address more advanced athletic training in detail in my book Ultimate Back Fitness and Performance (McGill, 2014). Begin with an assessment to understand the pain mechanisms. Then use the appropriate approach to address the mechanisms and build the person's tolerance and work capacity. Here is a summary of all five training stages:
- Stage 1: Establish quality movement engrams (motion patterns, motor patterns, and corrective exercise).
- Identify perturbed patterns and develop appropriate corrective exercise.
- Address basic movement patterns through to complex activity patterns.
- Address basic balance challenges through to complex and specific balance challenges.
- Stage 2: Build whole-body and joint stability (focus on spine stability here).
- Build stability while sparing the joints.
- Ensure sufficient stability commensurate with the demands of the task.
- Apply these patterns to the performance of daily activities.
- Stage 3: Increase endurance.
- Address basic endurance training to ensure the capacity needed for stabilization.
- Address activity-specific endurance (duration, intensity).
- Increase the ability to repeat pristine movement patterns without fatigue-induced compromise.
- Build the base for eventual performance training (only in those with this goal).
- Stage 4: Build strength.
- Spare the joints while maximizing the neuromuscular compartment challenge.
- Progress to skill movements.
- Stage 5: Develop speed, power, and agility.
- Develop ultimate performance based on the foundation laid in stages 1 through 4.
- Focus on optimizing elastic energy storage and recovery.
- Employ the techniques of superstiffness.
If you master the first three stages, which are discussed in this chapter, you will understand how to get bad backs to respond and how to develop better rehabilitation programs.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Models for measuring biological signals to assess risk
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Biological Signal - Driven Model Approaches
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Marras Model and McGill Model
The Marras model (Marras and Sommerich, 1991a, 1991b) measures electromyograms (EMGs) from several muscles and, using known physiological relationships, assigns forces to the muscles during virtually any industrial task. As noted earlier, this approach revealed powerful evidence linking the physical demands of specific occupational tasks with the incidence of LBD.
The McGill model (see chapter 1) uses the same philosophical approach to assign forces to the muscles, but attempts to include the highest level of anatomical accuracy possible. For example, it also measures three-dimensional spine curvature to assess forces to the passive tissues, including the intervertebral discs and the ligaments. By assigning forces to muscles and passive tissues throughout the full range of spine motion, it captures the ways people perform their jobs and even how they change with repetitions of the same jobs. The obvious liability of the approach is its enormous computational requirements, postprocessing of data, and difficulty collecting such comprehensive data from a wide number of workers in the field.
The question of the validity of this type of model must be addressed along with other models based on the biological approach. Some have argued that because these models contain known biomechanical and physiological relationships, they contain a certain amount of content validity. Moreover, both the Marras model and the McGill model have been quite successful in estimating the passive tissue and muscle forces that sum together to produce flexion and extension, lateral bend, and axial twisting moments. (These moments have been well predicted, with the exception of the twisting moment.) In summary, if twisting is not a dominant moment of force in a particular job, these models appear to predict accurate distributions of forces among the support tissues.
EMG-Assisted Optimization Approach
Perhaps the current pinnacle of model evolution is a hybrid modeling approach known as EMG-assisted optimization (developed by Cholewicki and McGill, 1994) with stability analysis and tissue load prediction (Cholewicki and McGill, 1996, was an early example, and Ikeda and McGill, 2012, is a more recent example). This approach exploits the asset of the biological EMG approach to distribute loads among the tissues based on the biological behavior of the subject. It then uses optimization to fine-tune the balancing of joint torques about several low back joints. The optimization takes the biologically predicted forces and adjusts muscle forces the minimal amount possible to satisfy the three-dimensional moment axes at every joint over the length of the lumbar spine. Once the three-dimensional moments have been assigned and tissue forces determined, an analysis of spine stability is performed via comparison of the joules of work imposed on the spine through perturbation with the joules of potential energy existing in the stiffened column.
This most highly evolved of spine models provides the biomechanist or ergonomist with insight into injury mechanisms caused by instability (as witnessed by Cholewicki and McGill, 1992) such as occurs while picking up a very light load from the floor. Even though patients have reported back injury from incidents such as bending over to tie a shoe, previous modeling approaches were sensitive only to tissue damage and injury scenarios produced from large loads and moments. Now a biomechanical explanation is available to explain the subsequent tissue damage, and a method is available to detect the risk of its happening. Although the routine use of this type of sophisticated model by ergonomists is not feasible, it is useful (for trained scientists) for analyzing individual workers and identifying those who are at elevated risk of injury because of faulty personal motor patterns.
Simple or Complex Models?
In summary, the complex models provide a tool to investigate the mechanisms of injury and the effects of technique during material handling on the risk of injury. The most complex and most highly evolved models provide insight into how injury occurs with all types of heavy and light loads. On the other hand, the simpler models, although sacrificing accuracy, can be powerful tools for the routine surveillance of physical demands in the workplace, but they must be wisely interpreted in each case given their limitations and constraints. Biomechanics and ergonomics require the full continuum of models. The choice of which one to use depends on the issue in question.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Postural tests for formal assessment
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit.
Formal Assessment of Posture
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit. Some tests are posturally based, whereas others assess control of motion.The following postural tests are very helpful. Recall that screening need not involve manipulation or special positions. Some of the most useful "tests" are simply intelligent observation.
Sitting Posture
Remarkably, patients with troubled backs often sit in a way that causes more back troubles. For example, patients who show flexion intolerance during provocative tests often have a typical sitting posture that involves a lot of spine flexion. In a similar way, those who show extension intolerance often sit with the spine locked into extension. The sitting posture is the first clue in hypothesis formation because this is often the posture that is first observed in the waiting area. Sitting in the waiting room in a flexed posture often suggests flexion intolerance.
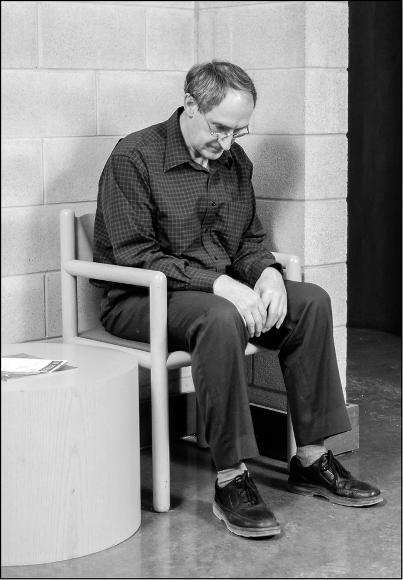
Photos from Stuart McGill
After noting the sitting posture, observe how the patient shifts from a slouched sitting posture to an upright one. Did she lift the rib cage, stressing the thoracolumbar junction ( a and b). Or did she flex the hips, rolling the pelvis forward to align the spine (c). Our recent work has shown that the best choice for most patients is to use a combination of the two (Castanhero et al., 2014) to minimize stress and avoid pain.
 |  |  |
Does the patient sit with a neutral spine (a) or a flexed spine (b)? When shifting from a slouch to a more upright posture, is the movement concentrated about the thoracolumbar junction or hips (c)?
Standing Pattern
All sorts of clues are revealed in the standing posture. Simple palpation of the standing patient's lumbar extensor muscles will reveal whether the patient is chronically crushing the back with extensor contraction. Simple postural corrections such as extending the hip, retracting the shoulders posteriorly, and pulling in the chin can shut these muscles off.
 |  |  |
|
Teach patients to palpate the erectors at the L3 level, and learn where the switch point is between muscle activation and muscle relaxation. They do this by standing upright, head erect and shoulders back, and then leaning forward slightly (a). Then they perfect this strategy to relax the muscle. Teach them that chin poking (b) and shoulder slouching (c) activate the muscles that cause fatigue cramps. Have them try the hitchhiking thumb position as a correction strategy, externally rotating the arms about the shoulders and then letting the shoulders relax into this new position (d).Having patients palpate the lumbar erectors helps them learn self-correcting strategies - are the erectors silent or active (a)? If they are active, show the patient how to shut them off by unloading the spine, which often provides immediate relief of muscular pain. Cues include shifting the head and neck from a chin poke to chin retraction position, adopting a hitchhiking posture with external rotation of the arms and shoulders, and pulling the hips forward (b, c).
 |  |  |
No amount of muscle relaxants will shut off the painful back muscles if the patient stands in a slouched posture. Standing to spare the spine requires a finely tuned blend of postural adjustments and muscle activation patterns. One correction is to steer the thumbs in external rotation, retracting the shoulders (see b and c) to a spine-sparing, corrected posture.
Some patients stand with no measurable extensor or abdominal muscle activation - they simply balance on their passive elastic spine tissues. These people tend to have thick torsos with flaccid abdominal walls. For these patients, pain reduction can be achieved with mild abdominal contraction; 2 or 3% of maximal voluntary contraction is considered normal abdominal wall muscle tone during standing (Juker et al., 1998).
Lying Pattern
Stress during lying is a function of body shape, the lying surface, and the pain mechanism. For back sleepers with protruding buttocks, lying on a hard surface causes a bridge under the lumbar spine. This causes spine flexion as the back flattens to the mattress and pain in the flexion-intolerant back. This may be addressed with support such as a folded towel (a, b). In a similar fashion, wide hips cause full, and painful, spine lateral bend in side-lying. In this case, a pillow-top surface can provide relief.
 |
|
(a-b) Painful backs with lying and sleeping postures are usually relieved with support to foster a neutral posture. This support may be in the form of mattress selection (adjusting firmness and the thickness of the pillow-top) or buttressing devices such as a folded towel in a person whose spine is bridged with protruding buttocks (a). A pillow to support the neck and knees may assist with side lying (b).
Learn more about Low Back Disorders, Third Edition With Web Resource.
Treatment isn't a recipe from a cookbook: Strategies for individualizing rehabilitation
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
Finding the Best Approach
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
- Encourage patients to train for health versus performance. The notion that athletes are healthy is generally a myth, at least from a musculoskeletal point of view. Training for superior athletic performance demands substantial overload of the muscles and tissues of the joints. An elevated risk of injury is associated with athletic training and performance. Unfortunately, many patients observe the routines used by athletes to enhance performance and wrongly conclude that copying them will help their own backs. Training for health requires quite a different philosophy; it emphasizes muscle endurance, motor control perfection, and the maintenance of sufficient spine stability in all expected tasks. Although strength is not a goal, strength gains do result. If a patient with back pain states that his objective is to play tennis or golf, then he has the wrong short-term objective. First and foremost, the objective is to eliminate pain. Then the objective may shift toward a performance objective such as participation in a sporting activity.
- Integrate prevention and rehabilitation approaches.The best therapy rigorously followed will not produce results if the cause of the back troubles is not addressed. Part II provided guidelines for reducing the risk of back troubles: the importance of removing the cause of tissue overload cannot be overstressed. Linton and van Tulder (2001) demonstrated the efficacy of exercise for prevention; exercise satisfies the objective for both better prevention and better rehabilitation outcomes. First, teach patients what is causing their troubles; then work with them to eliminate the cause.
- Work toward a slow, continuous improvement in function and pain reduction. The return of function and the reduction of pain, particularly for those with chronic bad backs, is a slow process. The typical pattern of recovery is akin to that of the stock market. Daily, and even weekly, price fluctuations eventually result in higher prices. Patients have good days and bad days. Many times lawyers have hired private investigators to make clandestine videos of people with back troubles performing tasks that appear inconsistent with those troubles. I am hired to provide comment. Some of these people are true malingerers and get caught. Others are simply having a good day when they are video-recorded. In such cases, I see all sorts of movement pathology consistent with their chronic history, and they are exonerated.
- Have the patient keep a journal of daily activities. Sometimes it is difficult to hone in on the pain mechanism and the correct dosage and exercise form. Examining daily pain and activity patterns can help identify the link with mechanical scenarios that exacerbate the pain. Two critical components should be recorded in a daily journal: how the back feels and what tasks and activities were performed. When patients encounter repeated setbacks, they should try to identify a common task or activity that preceded the pain episode. Likewise, even when progress is slow, patients should be encouraged to see some progress nonetheless. Without referring to the diary, patients sometimes do not realize that they are improving. Linking pain with a dose of activity is different from recording pain on a 10-point scale, which is typical of behavior modification programs. I have seen too many patients from these programs obsessing over their pain levels; for these people, we suggest stopping pain recording.
- Ensure a positive slope in progress. Chapters 10 and 11introduce the big three exercises in different forms. We designed these exercises to spare the spine from large loads and to groove stabilizing motor patterns. Use the three to establish a positive slope in patient improvement. Once the slope is established, you may choose to add new exercises one at a time. The patient may tolerate some exercises well and others not so well. If the improvement slope is lost after adding a new activity, remove it, go back to the big three, and reestablish the positive slope. If the patient requires advanced exercises for athletic performance, perhaps to increase spine mobility, you may add exercises to achieve such objectives after establishing the positive slope. How long should each stage be? There is no single answer for everyone. Some progress quickly, whereas others require great patience. Your job is to determine the initial challenge, to gauge progress and enhance the challenge accordingly, and to keep the patient motivated, even during periods of no apparent progress. The great clinicians blend keen clinical skills and experience with scientifically founded guidelines and knowledge.
- Determine whether the patient is willing to make a change. Obviously, the patient must change the current patterns that caused her to become a back patient. This requires motivation, which is not always easy to establish. Some have listed the importance of, and steps for developing, a change in motivation and attitude (e.g., Ranney, 1997). Briefly, such a program begins with the setting of goals - for example, returning to a specific job or partaking in a leisure activity. The employer's role in enhancing motivation is to ensure that modified work is available together with the opportunity for a graduated return to duty. Employers can also enhance motivation by fostering a culture in which worker success equates to company success, which in turn helps the worker. The second step in a motivation program is to formulate a realistic plan for reaching the goal established in the first step. It is beyond the mandate of this book to develop the components of maintaining and enhancing motivational opportunities at each stage of recovery.
- Determine whether the patient needs initial mobilization. Although everyone should incorporate spine stabilization exercises into daily activity, a small group of people will benefit from some directed soft tissue work (e.g., manipulation, trigger point therapy, Active Release Techniques, the use of foam rollers). These techniques are not the focus of this book. A word of caution is required here. Too many make the mistake of trying to mobilize a painful spine region that already has mobility. Nonetheless, there is good evidence that those with documented hypomobility may benefit from some initial manipulation or mobilization with a transition into stabilization training (Fritz, Whitman, and Childs, 2005).
- Consider other soft tissue treatments. A good manual medicine clinician may perceive local muscle spasms and odd-feeling local muscle texture. Further, these spasms and local neurocompartment disorders are associated with larger dysfunctions of the agonist and synergist muscles involved in a movement. In many cases these dysfunctions delay recovery or prevent complete recovery. Clinicians use a variety of soft tissue treatments to reduce spasm and release tissues that can impede attaining more normal muscular and joint function. Documenting them is beyond the scope of this book. We simply alert you to their potential significance and role in rehabilitation.
- Avoid spine power. Spine power is the product of velocity and force (power = force × velocity). This means that the spine is bending quickly and there is velocity in the muscles' lengthening and shortening. Techniques that involve high velocity in the spine have been shown to lead to back troubles, because they usually indicate high power (Marras et al., 1993; Stevenson et al., 2001). To minimize power and maximize safety, the forces transmitted through the trunk must be low if the spine is moving. If the forces transmitted through the trunk are high, then the velocity must be low. The power must be generated at the hips and shoulders and transmitted through an isometrically stabilized torso. Fortunately, this fundamental tenet for safety also helps to maximize performance.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Five stages to reduce back pain through exercise
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood.
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood. However, many more exercise-induced analgesic pathways are coming to light. One example is that exercise increases neurotrophin-3 production, which appears to have an analgesic role in cutaneous and deep tissue pan (Sharma et al., 2010).
Psychological components are important for some patients and influence the approach used to introduce and program exercise. For example, some patients obsess over their pain and what is going on in their bodies. Patients with high fear avoidance do better with physical therapy, which de-emphasizes anatomical findings (George et al., 2003). For these types of patients, I suggest not using daily pain charts, but directing their focus to achieving good exercise form. Some patients have back pain because they overload themselves with daily regimens at the gym. For the type A personality, we ensure that exercise is not overexecuted (for people who believe that 25 repetitions of an exercise will do them more good than the 10 that were prescribed). For the type B personality who may bargain with the clinician about doing less exercise, performing the exercise dose as prescribed should be encouraged. These two personality types require different approaches to prescribing exercise.
Some people have pain as a result of tissues that are inappropriately weak for the applied demands. In such cases the goal of exercise is to strengthen tissue, which requires a certain kind of programming. Athletes I have worked with who have recovered well from compression fractures have incorporated sufficient rest intervals to allow the injury to adapt between loading sessions. This appears to not work with collagenous disc injuries given the time required (years) for migrated nucleus material to gristle and form a plug (Adams and Dolan, 2005). Thus, the type of tissue that is the target for strengthening should determine the exercise approach.
Imbalances in joint and muscle function create odd stress patterns and more pain. For example, hip and back pain can cause gluteal muscle inhibition (Freeman, Mascia, and McGill, 2013), which makes the hamstring muscles dominant in creating hip extension moment. Because of the lines of action of these muscles, this causes more load on the anterior acetabulum and labrum of the hip (Lewis, Sahrmann, and Moran, 2009), resulting in associated hip pain.
There is also substantial support for the notion of the existence of a psychological profile associated with fitness - that is, that fitter people ignore small discomforts. As discussed in the section Why and How You Should Read This Book, fitness reduces the tendency to catastrophize pain.
How is the most appropriate exercise determined to reduce each of these pain mechanisms? Although the assessment will reveal the pain mechanism, many challenging patients must be considered experiments in progress. Tweaking the exercise form and the dosage helps you to hone in on the optimal.
Five-Stage Back Training Program
We have developed a five-stage approach to back training that begins with identifying faulty movement patterns and ends with pain-free performance readiness. Consider this the big picture, because only athletes and people who perform demanding tasks will complete all five stages. However, it is important to understand the components and objectives of each stage, as well as their order. For example, patients may be unknowingly following a strengthening regimen (stage 4) without having addressed perturbed motion patterns (stage 1). Doing so will delay their recovery, or make them worse. So when approaching the program, you must first ask, Is the objective pain reduction and rehabilitation or athletic performance? Health objectives demand a focus on motion and motor patterns, stability, and endurance to achieve low tissue loads and a low-risk environment. Performance requires more overload, which naturally results in an elevated risk. The trick in the case of performance is to stay within the lowest risk possible.
Although all five major stages are listed here, only the first three are appropriate for rehabilitation and addressed in this book. Rigorous strength, speed, and power training are only for those interested in enhancing these attributes. The average person does not need them to have good back health. I address more advanced athletic training in detail in my book Ultimate Back Fitness and Performance (McGill, 2014). Begin with an assessment to understand the pain mechanisms. Then use the appropriate approach to address the mechanisms and build the person's tolerance and work capacity. Here is a summary of all five training stages:
- Stage 1: Establish quality movement engrams (motion patterns, motor patterns, and corrective exercise).
- Identify perturbed patterns and develop appropriate corrective exercise.
- Address basic movement patterns through to complex activity patterns.
- Address basic balance challenges through to complex and specific balance challenges.
- Stage 2: Build whole-body and joint stability (focus on spine stability here).
- Build stability while sparing the joints.
- Ensure sufficient stability commensurate with the demands of the task.
- Apply these patterns to the performance of daily activities.
- Stage 3: Increase endurance.
- Address basic endurance training to ensure the capacity needed for stabilization.
- Address activity-specific endurance (duration, intensity).
- Increase the ability to repeat pristine movement patterns without fatigue-induced compromise.
- Build the base for eventual performance training (only in those with this goal).
- Stage 4: Build strength.
- Spare the joints while maximizing the neuromuscular compartment challenge.
- Progress to skill movements.
- Stage 5: Develop speed, power, and agility.
- Develop ultimate performance based on the foundation laid in stages 1 through 4.
- Focus on optimizing elastic energy storage and recovery.
- Employ the techniques of superstiffness.
If you master the first three stages, which are discussed in this chapter, you will understand how to get bad backs to respond and how to develop better rehabilitation programs.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Models for measuring biological signals to assess risk
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Biological Signal - Driven Model Approaches
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Marras Model and McGill Model
The Marras model (Marras and Sommerich, 1991a, 1991b) measures electromyograms (EMGs) from several muscles and, using known physiological relationships, assigns forces to the muscles during virtually any industrial task. As noted earlier, this approach revealed powerful evidence linking the physical demands of specific occupational tasks with the incidence of LBD.
The McGill model (see chapter 1) uses the same philosophical approach to assign forces to the muscles, but attempts to include the highest level of anatomical accuracy possible. For example, it also measures three-dimensional spine curvature to assess forces to the passive tissues, including the intervertebral discs and the ligaments. By assigning forces to muscles and passive tissues throughout the full range of spine motion, it captures the ways people perform their jobs and even how they change with repetitions of the same jobs. The obvious liability of the approach is its enormous computational requirements, postprocessing of data, and difficulty collecting such comprehensive data from a wide number of workers in the field.
The question of the validity of this type of model must be addressed along with other models based on the biological approach. Some have argued that because these models contain known biomechanical and physiological relationships, they contain a certain amount of content validity. Moreover, both the Marras model and the McGill model have been quite successful in estimating the passive tissue and muscle forces that sum together to produce flexion and extension, lateral bend, and axial twisting moments. (These moments have been well predicted, with the exception of the twisting moment.) In summary, if twisting is not a dominant moment of force in a particular job, these models appear to predict accurate distributions of forces among the support tissues.
EMG-Assisted Optimization Approach
Perhaps the current pinnacle of model evolution is a hybrid modeling approach known as EMG-assisted optimization (developed by Cholewicki and McGill, 1994) with stability analysis and tissue load prediction (Cholewicki and McGill, 1996, was an early example, and Ikeda and McGill, 2012, is a more recent example). This approach exploits the asset of the biological EMG approach to distribute loads among the tissues based on the biological behavior of the subject. It then uses optimization to fine-tune the balancing of joint torques about several low back joints. The optimization takes the biologically predicted forces and adjusts muscle forces the minimal amount possible to satisfy the three-dimensional moment axes at every joint over the length of the lumbar spine. Once the three-dimensional moments have been assigned and tissue forces determined, an analysis of spine stability is performed via comparison of the joules of work imposed on the spine through perturbation with the joules of potential energy existing in the stiffened column.
This most highly evolved of spine models provides the biomechanist or ergonomist with insight into injury mechanisms caused by instability (as witnessed by Cholewicki and McGill, 1992) such as occurs while picking up a very light load from the floor. Even though patients have reported back injury from incidents such as bending over to tie a shoe, previous modeling approaches were sensitive only to tissue damage and injury scenarios produced from large loads and moments. Now a biomechanical explanation is available to explain the subsequent tissue damage, and a method is available to detect the risk of its happening. Although the routine use of this type of sophisticated model by ergonomists is not feasible, it is useful (for trained scientists) for analyzing individual workers and identifying those who are at elevated risk of injury because of faulty personal motor patterns.
Simple or Complex Models?
In summary, the complex models provide a tool to investigate the mechanisms of injury and the effects of technique during material handling on the risk of injury. The most complex and most highly evolved models provide insight into how injury occurs with all types of heavy and light loads. On the other hand, the simpler models, although sacrificing accuracy, can be powerful tools for the routine surveillance of physical demands in the workplace, but they must be wisely interpreted in each case given their limitations and constraints. Biomechanics and ergonomics require the full continuum of models. The choice of which one to use depends on the issue in question.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Postural tests for formal assessment
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit.
Formal Assessment of Posture
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit. Some tests are posturally based, whereas others assess control of motion.The following postural tests are very helpful. Recall that screening need not involve manipulation or special positions. Some of the most useful "tests" are simply intelligent observation.
Sitting Posture
Remarkably, patients with troubled backs often sit in a way that causes more back troubles. For example, patients who show flexion intolerance during provocative tests often have a typical sitting posture that involves a lot of spine flexion. In a similar way, those who show extension intolerance often sit with the spine locked into extension. The sitting posture is the first clue in hypothesis formation because this is often the posture that is first observed in the waiting area. Sitting in the waiting room in a flexed posture often suggests flexion intolerance.
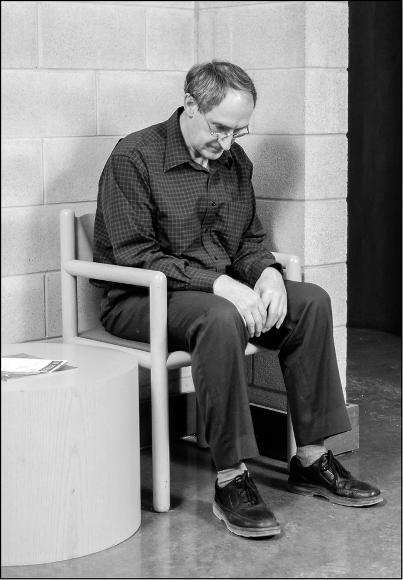
Photos from Stuart McGill
After noting the sitting posture, observe how the patient shifts from a slouched sitting posture to an upright one. Did she lift the rib cage, stressing the thoracolumbar junction ( a and b). Or did she flex the hips, rolling the pelvis forward to align the spine (c). Our recent work has shown that the best choice for most patients is to use a combination of the two (Castanhero et al., 2014) to minimize stress and avoid pain.
 |  |  |
Does the patient sit with a neutral spine (a) or a flexed spine (b)? When shifting from a slouch to a more upright posture, is the movement concentrated about the thoracolumbar junction or hips (c)?
Standing Pattern
All sorts of clues are revealed in the standing posture. Simple palpation of the standing patient's lumbar extensor muscles will reveal whether the patient is chronically crushing the back with extensor contraction. Simple postural corrections such as extending the hip, retracting the shoulders posteriorly, and pulling in the chin can shut these muscles off.
 |  |  |
|
Teach patients to palpate the erectors at the L3 level, and learn where the switch point is between muscle activation and muscle relaxation. They do this by standing upright, head erect and shoulders back, and then leaning forward slightly (a). Then they perfect this strategy to relax the muscle. Teach them that chin poking (b) and shoulder slouching (c) activate the muscles that cause fatigue cramps. Have them try the hitchhiking thumb position as a correction strategy, externally rotating the arms about the shoulders and then letting the shoulders relax into this new position (d).Having patients palpate the lumbar erectors helps them learn self-correcting strategies - are the erectors silent or active (a)? If they are active, show the patient how to shut them off by unloading the spine, which often provides immediate relief of muscular pain. Cues include shifting the head and neck from a chin poke to chin retraction position, adopting a hitchhiking posture with external rotation of the arms and shoulders, and pulling the hips forward (b, c).
 |  |  |
No amount of muscle relaxants will shut off the painful back muscles if the patient stands in a slouched posture. Standing to spare the spine requires a finely tuned blend of postural adjustments and muscle activation patterns. One correction is to steer the thumbs in external rotation, retracting the shoulders (see b and c) to a spine-sparing, corrected posture.
Some patients stand with no measurable extensor or abdominal muscle activation - they simply balance on their passive elastic spine tissues. These people tend to have thick torsos with flaccid abdominal walls. For these patients, pain reduction can be achieved with mild abdominal contraction; 2 or 3% of maximal voluntary contraction is considered normal abdominal wall muscle tone during standing (Juker et al., 1998).
Lying Pattern
Stress during lying is a function of body shape, the lying surface, and the pain mechanism. For back sleepers with protruding buttocks, lying on a hard surface causes a bridge under the lumbar spine. This causes spine flexion as the back flattens to the mattress and pain in the flexion-intolerant back. This may be addressed with support such as a folded towel (a, b). In a similar fashion, wide hips cause full, and painful, spine lateral bend in side-lying. In this case, a pillow-top surface can provide relief.
 |
|
(a-b) Painful backs with lying and sleeping postures are usually relieved with support to foster a neutral posture. This support may be in the form of mattress selection (adjusting firmness and the thickness of the pillow-top) or buttressing devices such as a folded towel in a person whose spine is bridged with protruding buttocks (a). A pillow to support the neck and knees may assist with side lying (b).
Learn more about Low Back Disorders, Third Edition With Web Resource.
Treatment isn't a recipe from a cookbook: Strategies for individualizing rehabilitation
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
Finding the Best Approach
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
- Encourage patients to train for health versus performance. The notion that athletes are healthy is generally a myth, at least from a musculoskeletal point of view. Training for superior athletic performance demands substantial overload of the muscles and tissues of the joints. An elevated risk of injury is associated with athletic training and performance. Unfortunately, many patients observe the routines used by athletes to enhance performance and wrongly conclude that copying them will help their own backs. Training for health requires quite a different philosophy; it emphasizes muscle endurance, motor control perfection, and the maintenance of sufficient spine stability in all expected tasks. Although strength is not a goal, strength gains do result. If a patient with back pain states that his objective is to play tennis or golf, then he has the wrong short-term objective. First and foremost, the objective is to eliminate pain. Then the objective may shift toward a performance objective such as participation in a sporting activity.
- Integrate prevention and rehabilitation approaches.The best therapy rigorously followed will not produce results if the cause of the back troubles is not addressed. Part II provided guidelines for reducing the risk of back troubles: the importance of removing the cause of tissue overload cannot be overstressed. Linton and van Tulder (2001) demonstrated the efficacy of exercise for prevention; exercise satisfies the objective for both better prevention and better rehabilitation outcomes. First, teach patients what is causing their troubles; then work with them to eliminate the cause.
- Work toward a slow, continuous improvement in function and pain reduction. The return of function and the reduction of pain, particularly for those with chronic bad backs, is a slow process. The typical pattern of recovery is akin to that of the stock market. Daily, and even weekly, price fluctuations eventually result in higher prices. Patients have good days and bad days. Many times lawyers have hired private investigators to make clandestine videos of people with back troubles performing tasks that appear inconsistent with those troubles. I am hired to provide comment. Some of these people are true malingerers and get caught. Others are simply having a good day when they are video-recorded. In such cases, I see all sorts of movement pathology consistent with their chronic history, and they are exonerated.
- Have the patient keep a journal of daily activities. Sometimes it is difficult to hone in on the pain mechanism and the correct dosage and exercise form. Examining daily pain and activity patterns can help identify the link with mechanical scenarios that exacerbate the pain. Two critical components should be recorded in a daily journal: how the back feels and what tasks and activities were performed. When patients encounter repeated setbacks, they should try to identify a common task or activity that preceded the pain episode. Likewise, even when progress is slow, patients should be encouraged to see some progress nonetheless. Without referring to the diary, patients sometimes do not realize that they are improving. Linking pain with a dose of activity is different from recording pain on a 10-point scale, which is typical of behavior modification programs. I have seen too many patients from these programs obsessing over their pain levels; for these people, we suggest stopping pain recording.
- Ensure a positive slope in progress. Chapters 10 and 11introduce the big three exercises in different forms. We designed these exercises to spare the spine from large loads and to groove stabilizing motor patterns. Use the three to establish a positive slope in patient improvement. Once the slope is established, you may choose to add new exercises one at a time. The patient may tolerate some exercises well and others not so well. If the improvement slope is lost after adding a new activity, remove it, go back to the big three, and reestablish the positive slope. If the patient requires advanced exercises for athletic performance, perhaps to increase spine mobility, you may add exercises to achieve such objectives after establishing the positive slope. How long should each stage be? There is no single answer for everyone. Some progress quickly, whereas others require great patience. Your job is to determine the initial challenge, to gauge progress and enhance the challenge accordingly, and to keep the patient motivated, even during periods of no apparent progress. The great clinicians blend keen clinical skills and experience with scientifically founded guidelines and knowledge.
- Determine whether the patient is willing to make a change. Obviously, the patient must change the current patterns that caused her to become a back patient. This requires motivation, which is not always easy to establish. Some have listed the importance of, and steps for developing, a change in motivation and attitude (e.g., Ranney, 1997). Briefly, such a program begins with the setting of goals - for example, returning to a specific job or partaking in a leisure activity. The employer's role in enhancing motivation is to ensure that modified work is available together with the opportunity for a graduated return to duty. Employers can also enhance motivation by fostering a culture in which worker success equates to company success, which in turn helps the worker. The second step in a motivation program is to formulate a realistic plan for reaching the goal established in the first step. It is beyond the mandate of this book to develop the components of maintaining and enhancing motivational opportunities at each stage of recovery.
- Determine whether the patient needs initial mobilization. Although everyone should incorporate spine stabilization exercises into daily activity, a small group of people will benefit from some directed soft tissue work (e.g., manipulation, trigger point therapy, Active Release Techniques, the use of foam rollers). These techniques are not the focus of this book. A word of caution is required here. Too many make the mistake of trying to mobilize a painful spine region that already has mobility. Nonetheless, there is good evidence that those with documented hypomobility may benefit from some initial manipulation or mobilization with a transition into stabilization training (Fritz, Whitman, and Childs, 2005).
- Consider other soft tissue treatments. A good manual medicine clinician may perceive local muscle spasms and odd-feeling local muscle texture. Further, these spasms and local neurocompartment disorders are associated with larger dysfunctions of the agonist and synergist muscles involved in a movement. In many cases these dysfunctions delay recovery or prevent complete recovery. Clinicians use a variety of soft tissue treatments to reduce spasm and release tissues that can impede attaining more normal muscular and joint function. Documenting them is beyond the scope of this book. We simply alert you to their potential significance and role in rehabilitation.
- Avoid spine power. Spine power is the product of velocity and force (power = force × velocity). This means that the spine is bending quickly and there is velocity in the muscles' lengthening and shortening. Techniques that involve high velocity in the spine have been shown to lead to back troubles, because they usually indicate high power (Marras et al., 1993; Stevenson et al., 2001). To minimize power and maximize safety, the forces transmitted through the trunk must be low if the spine is moving. If the forces transmitted through the trunk are high, then the velocity must be low. The power must be generated at the hips and shoulders and transmitted through an isometrically stabilized torso. Fortunately, this fundamental tenet for safety also helps to maximize performance.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Five stages to reduce back pain through exercise
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood.
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood. However, many more exercise-induced analgesic pathways are coming to light. One example is that exercise increases neurotrophin-3 production, which appears to have an analgesic role in cutaneous and deep tissue pan (Sharma et al., 2010).
Psychological components are important for some patients and influence the approach used to introduce and program exercise. For example, some patients obsess over their pain and what is going on in their bodies. Patients with high fear avoidance do better with physical therapy, which de-emphasizes anatomical findings (George et al., 2003). For these types of patients, I suggest not using daily pain charts, but directing their focus to achieving good exercise form. Some patients have back pain because they overload themselves with daily regimens at the gym. For the type A personality, we ensure that exercise is not overexecuted (for people who believe that 25 repetitions of an exercise will do them more good than the 10 that were prescribed). For the type B personality who may bargain with the clinician about doing less exercise, performing the exercise dose as prescribed should be encouraged. These two personality types require different approaches to prescribing exercise.
Some people have pain as a result of tissues that are inappropriately weak for the applied demands. In such cases the goal of exercise is to strengthen tissue, which requires a certain kind of programming. Athletes I have worked with who have recovered well from compression fractures have incorporated sufficient rest intervals to allow the injury to adapt between loading sessions. This appears to not work with collagenous disc injuries given the time required (years) for migrated nucleus material to gristle and form a plug (Adams and Dolan, 2005). Thus, the type of tissue that is the target for strengthening should determine the exercise approach.
Imbalances in joint and muscle function create odd stress patterns and more pain. For example, hip and back pain can cause gluteal muscle inhibition (Freeman, Mascia, and McGill, 2013), which makes the hamstring muscles dominant in creating hip extension moment. Because of the lines of action of these muscles, this causes more load on the anterior acetabulum and labrum of the hip (Lewis, Sahrmann, and Moran, 2009), resulting in associated hip pain.
There is also substantial support for the notion of the existence of a psychological profile associated with fitness - that is, that fitter people ignore small discomforts. As discussed in the section Why and How You Should Read This Book, fitness reduces the tendency to catastrophize pain.
How is the most appropriate exercise determined to reduce each of these pain mechanisms? Although the assessment will reveal the pain mechanism, many challenging patients must be considered experiments in progress. Tweaking the exercise form and the dosage helps you to hone in on the optimal.
Five-Stage Back Training Program
We have developed a five-stage approach to back training that begins with identifying faulty movement patterns and ends with pain-free performance readiness. Consider this the big picture, because only athletes and people who perform demanding tasks will complete all five stages. However, it is important to understand the components and objectives of each stage, as well as their order. For example, patients may be unknowingly following a strengthening regimen (stage 4) without having addressed perturbed motion patterns (stage 1). Doing so will delay their recovery, or make them worse. So when approaching the program, you must first ask, Is the objective pain reduction and rehabilitation or athletic performance? Health objectives demand a focus on motion and motor patterns, stability, and endurance to achieve low tissue loads and a low-risk environment. Performance requires more overload, which naturally results in an elevated risk. The trick in the case of performance is to stay within the lowest risk possible.
Although all five major stages are listed here, only the first three are appropriate for rehabilitation and addressed in this book. Rigorous strength, speed, and power training are only for those interested in enhancing these attributes. The average person does not need them to have good back health. I address more advanced athletic training in detail in my book Ultimate Back Fitness and Performance (McGill, 2014). Begin with an assessment to understand the pain mechanisms. Then use the appropriate approach to address the mechanisms and build the person's tolerance and work capacity. Here is a summary of all five training stages:
- Stage 1: Establish quality movement engrams (motion patterns, motor patterns, and corrective exercise).
- Identify perturbed patterns and develop appropriate corrective exercise.
- Address basic movement patterns through to complex activity patterns.
- Address basic balance challenges through to complex and specific balance challenges.
- Stage 2: Build whole-body and joint stability (focus on spine stability here).
- Build stability while sparing the joints.
- Ensure sufficient stability commensurate with the demands of the task.
- Apply these patterns to the performance of daily activities.
- Stage 3: Increase endurance.
- Address basic endurance training to ensure the capacity needed for stabilization.
- Address activity-specific endurance (duration, intensity).
- Increase the ability to repeat pristine movement patterns without fatigue-induced compromise.
- Build the base for eventual performance training (only in those with this goal).
- Stage 4: Build strength.
- Spare the joints while maximizing the neuromuscular compartment challenge.
- Progress to skill movements.
- Stage 5: Develop speed, power, and agility.
- Develop ultimate performance based on the foundation laid in stages 1 through 4.
- Focus on optimizing elastic energy storage and recovery.
- Employ the techniques of superstiffness.
If you master the first three stages, which are discussed in this chapter, you will understand how to get bad backs to respond and how to develop better rehabilitation programs.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Models for measuring biological signals to assess risk
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Biological Signal - Driven Model Approaches
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Marras Model and McGill Model
The Marras model (Marras and Sommerich, 1991a, 1991b) measures electromyograms (EMGs) from several muscles and, using known physiological relationships, assigns forces to the muscles during virtually any industrial task. As noted earlier, this approach revealed powerful evidence linking the physical demands of specific occupational tasks with the incidence of LBD.
The McGill model (see chapter 1) uses the same philosophical approach to assign forces to the muscles, but attempts to include the highest level of anatomical accuracy possible. For example, it also measures three-dimensional spine curvature to assess forces to the passive tissues, including the intervertebral discs and the ligaments. By assigning forces to muscles and passive tissues throughout the full range of spine motion, it captures the ways people perform their jobs and even how they change with repetitions of the same jobs. The obvious liability of the approach is its enormous computational requirements, postprocessing of data, and difficulty collecting such comprehensive data from a wide number of workers in the field.
The question of the validity of this type of model must be addressed along with other models based on the biological approach. Some have argued that because these models contain known biomechanical and physiological relationships, they contain a certain amount of content validity. Moreover, both the Marras model and the McGill model have been quite successful in estimating the passive tissue and muscle forces that sum together to produce flexion and extension, lateral bend, and axial twisting moments. (These moments have been well predicted, with the exception of the twisting moment.) In summary, if twisting is not a dominant moment of force in a particular job, these models appear to predict accurate distributions of forces among the support tissues.
EMG-Assisted Optimization Approach
Perhaps the current pinnacle of model evolution is a hybrid modeling approach known as EMG-assisted optimization (developed by Cholewicki and McGill, 1994) with stability analysis and tissue load prediction (Cholewicki and McGill, 1996, was an early example, and Ikeda and McGill, 2012, is a more recent example). This approach exploits the asset of the biological EMG approach to distribute loads among the tissues based on the biological behavior of the subject. It then uses optimization to fine-tune the balancing of joint torques about several low back joints. The optimization takes the biologically predicted forces and adjusts muscle forces the minimal amount possible to satisfy the three-dimensional moment axes at every joint over the length of the lumbar spine. Once the three-dimensional moments have been assigned and tissue forces determined, an analysis of spine stability is performed via comparison of the joules of work imposed on the spine through perturbation with the joules of potential energy existing in the stiffened column.
This most highly evolved of spine models provides the biomechanist or ergonomist with insight into injury mechanisms caused by instability (as witnessed by Cholewicki and McGill, 1992) such as occurs while picking up a very light load from the floor. Even though patients have reported back injury from incidents such as bending over to tie a shoe, previous modeling approaches were sensitive only to tissue damage and injury scenarios produced from large loads and moments. Now a biomechanical explanation is available to explain the subsequent tissue damage, and a method is available to detect the risk of its happening. Although the routine use of this type of sophisticated model by ergonomists is not feasible, it is useful (for trained scientists) for analyzing individual workers and identifying those who are at elevated risk of injury because of faulty personal motor patterns.
Simple or Complex Models?
In summary, the complex models provide a tool to investigate the mechanisms of injury and the effects of technique during material handling on the risk of injury. The most complex and most highly evolved models provide insight into how injury occurs with all types of heavy and light loads. On the other hand, the simpler models, although sacrificing accuracy, can be powerful tools for the routine surveillance of physical demands in the workplace, but they must be wisely interpreted in each case given their limitations and constraints. Biomechanics and ergonomics require the full continuum of models. The choice of which one to use depends on the issue in question.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Postural tests for formal assessment
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit.
Formal Assessment of Posture
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit. Some tests are posturally based, whereas others assess control of motion.The following postural tests are very helpful. Recall that screening need not involve manipulation or special positions. Some of the most useful "tests" are simply intelligent observation.
Sitting Posture
Remarkably, patients with troubled backs often sit in a way that causes more back troubles. For example, patients who show flexion intolerance during provocative tests often have a typical sitting posture that involves a lot of spine flexion. In a similar way, those who show extension intolerance often sit with the spine locked into extension. The sitting posture is the first clue in hypothesis formation because this is often the posture that is first observed in the waiting area. Sitting in the waiting room in a flexed posture often suggests flexion intolerance.
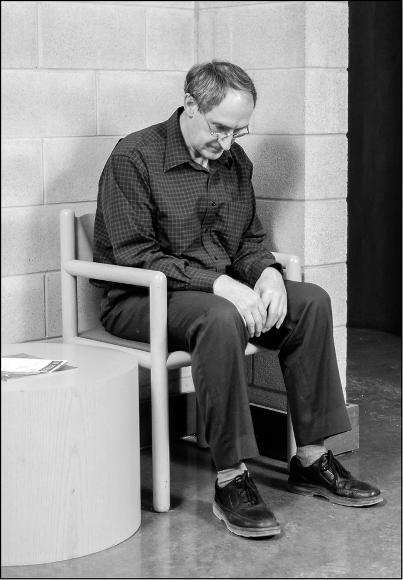
Photos from Stuart McGill
After noting the sitting posture, observe how the patient shifts from a slouched sitting posture to an upright one. Did she lift the rib cage, stressing the thoracolumbar junction ( a and b). Or did she flex the hips, rolling the pelvis forward to align the spine (c). Our recent work has shown that the best choice for most patients is to use a combination of the two (Castanhero et al., 2014) to minimize stress and avoid pain.
 |  |  |
Does the patient sit with a neutral spine (a) or a flexed spine (b)? When shifting from a slouch to a more upright posture, is the movement concentrated about the thoracolumbar junction or hips (c)?
Standing Pattern
All sorts of clues are revealed in the standing posture. Simple palpation of the standing patient's lumbar extensor muscles will reveal whether the patient is chronically crushing the back with extensor contraction. Simple postural corrections such as extending the hip, retracting the shoulders posteriorly, and pulling in the chin can shut these muscles off.
 |  |  |
|
Teach patients to palpate the erectors at the L3 level, and learn where the switch point is between muscle activation and muscle relaxation. They do this by standing upright, head erect and shoulders back, and then leaning forward slightly (a). Then they perfect this strategy to relax the muscle. Teach them that chin poking (b) and shoulder slouching (c) activate the muscles that cause fatigue cramps. Have them try the hitchhiking thumb position as a correction strategy, externally rotating the arms about the shoulders and then letting the shoulders relax into this new position (d).Having patients palpate the lumbar erectors helps them learn self-correcting strategies - are the erectors silent or active (a)? If they are active, show the patient how to shut them off by unloading the spine, which often provides immediate relief of muscular pain. Cues include shifting the head and neck from a chin poke to chin retraction position, adopting a hitchhiking posture with external rotation of the arms and shoulders, and pulling the hips forward (b, c).
 |  |  |
No amount of muscle relaxants will shut off the painful back muscles if the patient stands in a slouched posture. Standing to spare the spine requires a finely tuned blend of postural adjustments and muscle activation patterns. One correction is to steer the thumbs in external rotation, retracting the shoulders (see b and c) to a spine-sparing, corrected posture.
Some patients stand with no measurable extensor or abdominal muscle activation - they simply balance on their passive elastic spine tissues. These people tend to have thick torsos with flaccid abdominal walls. For these patients, pain reduction can be achieved with mild abdominal contraction; 2 or 3% of maximal voluntary contraction is considered normal abdominal wall muscle tone during standing (Juker et al., 1998).
Lying Pattern
Stress during lying is a function of body shape, the lying surface, and the pain mechanism. For back sleepers with protruding buttocks, lying on a hard surface causes a bridge under the lumbar spine. This causes spine flexion as the back flattens to the mattress and pain in the flexion-intolerant back. This may be addressed with support such as a folded towel (a, b). In a similar fashion, wide hips cause full, and painful, spine lateral bend in side-lying. In this case, a pillow-top surface can provide relief.
 |
|
(a-b) Painful backs with lying and sleeping postures are usually relieved with support to foster a neutral posture. This support may be in the form of mattress selection (adjusting firmness and the thickness of the pillow-top) or buttressing devices such as a folded towel in a person whose spine is bridged with protruding buttocks (a). A pillow to support the neck and knees may assist with side lying (b).
Learn more about Low Back Disorders, Third Edition With Web Resource.
Treatment isn't a recipe from a cookbook: Strategies for individualizing rehabilitation
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
Finding the Best Approach
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
- Encourage patients to train for health versus performance. The notion that athletes are healthy is generally a myth, at least from a musculoskeletal point of view. Training for superior athletic performance demands substantial overload of the muscles and tissues of the joints. An elevated risk of injury is associated with athletic training and performance. Unfortunately, many patients observe the routines used by athletes to enhance performance and wrongly conclude that copying them will help their own backs. Training for health requires quite a different philosophy; it emphasizes muscle endurance, motor control perfection, and the maintenance of sufficient spine stability in all expected tasks. Although strength is not a goal, strength gains do result. If a patient with back pain states that his objective is to play tennis or golf, then he has the wrong short-term objective. First and foremost, the objective is to eliminate pain. Then the objective may shift toward a performance objective such as participation in a sporting activity.
- Integrate prevention and rehabilitation approaches.The best therapy rigorously followed will not produce results if the cause of the back troubles is not addressed. Part II provided guidelines for reducing the risk of back troubles: the importance of removing the cause of tissue overload cannot be overstressed. Linton and van Tulder (2001) demonstrated the efficacy of exercise for prevention; exercise satisfies the objective for both better prevention and better rehabilitation outcomes. First, teach patients what is causing their troubles; then work with them to eliminate the cause.
- Work toward a slow, continuous improvement in function and pain reduction. The return of function and the reduction of pain, particularly for those with chronic bad backs, is a slow process. The typical pattern of recovery is akin to that of the stock market. Daily, and even weekly, price fluctuations eventually result in higher prices. Patients have good days and bad days. Many times lawyers have hired private investigators to make clandestine videos of people with back troubles performing tasks that appear inconsistent with those troubles. I am hired to provide comment. Some of these people are true malingerers and get caught. Others are simply having a good day when they are video-recorded. In such cases, I see all sorts of movement pathology consistent with their chronic history, and they are exonerated.
- Have the patient keep a journal of daily activities. Sometimes it is difficult to hone in on the pain mechanism and the correct dosage and exercise form. Examining daily pain and activity patterns can help identify the link with mechanical scenarios that exacerbate the pain. Two critical components should be recorded in a daily journal: how the back feels and what tasks and activities were performed. When patients encounter repeated setbacks, they should try to identify a common task or activity that preceded the pain episode. Likewise, even when progress is slow, patients should be encouraged to see some progress nonetheless. Without referring to the diary, patients sometimes do not realize that they are improving. Linking pain with a dose of activity is different from recording pain on a 10-point scale, which is typical of behavior modification programs. I have seen too many patients from these programs obsessing over their pain levels; for these people, we suggest stopping pain recording.
- Ensure a positive slope in progress. Chapters 10 and 11introduce the big three exercises in different forms. We designed these exercises to spare the spine from large loads and to groove stabilizing motor patterns. Use the three to establish a positive slope in patient improvement. Once the slope is established, you may choose to add new exercises one at a time. The patient may tolerate some exercises well and others not so well. If the improvement slope is lost after adding a new activity, remove it, go back to the big three, and reestablish the positive slope. If the patient requires advanced exercises for athletic performance, perhaps to increase spine mobility, you may add exercises to achieve such objectives after establishing the positive slope. How long should each stage be? There is no single answer for everyone. Some progress quickly, whereas others require great patience. Your job is to determine the initial challenge, to gauge progress and enhance the challenge accordingly, and to keep the patient motivated, even during periods of no apparent progress. The great clinicians blend keen clinical skills and experience with scientifically founded guidelines and knowledge.
- Determine whether the patient is willing to make a change. Obviously, the patient must change the current patterns that caused her to become a back patient. This requires motivation, which is not always easy to establish. Some have listed the importance of, and steps for developing, a change in motivation and attitude (e.g., Ranney, 1997). Briefly, such a program begins with the setting of goals - for example, returning to a specific job or partaking in a leisure activity. The employer's role in enhancing motivation is to ensure that modified work is available together with the opportunity for a graduated return to duty. Employers can also enhance motivation by fostering a culture in which worker success equates to company success, which in turn helps the worker. The second step in a motivation program is to formulate a realistic plan for reaching the goal established in the first step. It is beyond the mandate of this book to develop the components of maintaining and enhancing motivational opportunities at each stage of recovery.
- Determine whether the patient needs initial mobilization. Although everyone should incorporate spine stabilization exercises into daily activity, a small group of people will benefit from some directed soft tissue work (e.g., manipulation, trigger point therapy, Active Release Techniques, the use of foam rollers). These techniques are not the focus of this book. A word of caution is required here. Too many make the mistake of trying to mobilize a painful spine region that already has mobility. Nonetheless, there is good evidence that those with documented hypomobility may benefit from some initial manipulation or mobilization with a transition into stabilization training (Fritz, Whitman, and Childs, 2005).
- Consider other soft tissue treatments. A good manual medicine clinician may perceive local muscle spasms and odd-feeling local muscle texture. Further, these spasms and local neurocompartment disorders are associated with larger dysfunctions of the agonist and synergist muscles involved in a movement. In many cases these dysfunctions delay recovery or prevent complete recovery. Clinicians use a variety of soft tissue treatments to reduce spasm and release tissues that can impede attaining more normal muscular and joint function. Documenting them is beyond the scope of this book. We simply alert you to their potential significance and role in rehabilitation.
- Avoid spine power. Spine power is the product of velocity and force (power = force × velocity). This means that the spine is bending quickly and there is velocity in the muscles' lengthening and shortening. Techniques that involve high velocity in the spine have been shown to lead to back troubles, because they usually indicate high power (Marras et al., 1993; Stevenson et al., 2001). To minimize power and maximize safety, the forces transmitted through the trunk must be low if the spine is moving. If the forces transmitted through the trunk are high, then the velocity must be low. The power must be generated at the hips and shoulders and transmitted through an isometrically stabilized torso. Fortunately, this fundamental tenet for safety also helps to maximize performance.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Five stages to reduce back pain through exercise
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood.
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood. However, many more exercise-induced analgesic pathways are coming to light. One example is that exercise increases neurotrophin-3 production, which appears to have an analgesic role in cutaneous and deep tissue pan (Sharma et al., 2010).
Psychological components are important for some patients and influence the approach used to introduce and program exercise. For example, some patients obsess over their pain and what is going on in their bodies. Patients with high fear avoidance do better with physical therapy, which de-emphasizes anatomical findings (George et al., 2003). For these types of patients, I suggest not using daily pain charts, but directing their focus to achieving good exercise form. Some patients have back pain because they overload themselves with daily regimens at the gym. For the type A personality, we ensure that exercise is not overexecuted (for people who believe that 25 repetitions of an exercise will do them more good than the 10 that were prescribed). For the type B personality who may bargain with the clinician about doing less exercise, performing the exercise dose as prescribed should be encouraged. These two personality types require different approaches to prescribing exercise.
Some people have pain as a result of tissues that are inappropriately weak for the applied demands. In such cases the goal of exercise is to strengthen tissue, which requires a certain kind of programming. Athletes I have worked with who have recovered well from compression fractures have incorporated sufficient rest intervals to allow the injury to adapt between loading sessions. This appears to not work with collagenous disc injuries given the time required (years) for migrated nucleus material to gristle and form a plug (Adams and Dolan, 2005). Thus, the type of tissue that is the target for strengthening should determine the exercise approach.
Imbalances in joint and muscle function create odd stress patterns and more pain. For example, hip and back pain can cause gluteal muscle inhibition (Freeman, Mascia, and McGill, 2013), which makes the hamstring muscles dominant in creating hip extension moment. Because of the lines of action of these muscles, this causes more load on the anterior acetabulum and labrum of the hip (Lewis, Sahrmann, and Moran, 2009), resulting in associated hip pain.
There is also substantial support for the notion of the existence of a psychological profile associated with fitness - that is, that fitter people ignore small discomforts. As discussed in the section Why and How You Should Read This Book, fitness reduces the tendency to catastrophize pain.
How is the most appropriate exercise determined to reduce each of these pain mechanisms? Although the assessment will reveal the pain mechanism, many challenging patients must be considered experiments in progress. Tweaking the exercise form and the dosage helps you to hone in on the optimal.
Five-Stage Back Training Program
We have developed a five-stage approach to back training that begins with identifying faulty movement patterns and ends with pain-free performance readiness. Consider this the big picture, because only athletes and people who perform demanding tasks will complete all five stages. However, it is important to understand the components and objectives of each stage, as well as their order. For example, patients may be unknowingly following a strengthening regimen (stage 4) without having addressed perturbed motion patterns (stage 1). Doing so will delay their recovery, or make them worse. So when approaching the program, you must first ask, Is the objective pain reduction and rehabilitation or athletic performance? Health objectives demand a focus on motion and motor patterns, stability, and endurance to achieve low tissue loads and a low-risk environment. Performance requires more overload, which naturally results in an elevated risk. The trick in the case of performance is to stay within the lowest risk possible.
Although all five major stages are listed here, only the first three are appropriate for rehabilitation and addressed in this book. Rigorous strength, speed, and power training are only for those interested in enhancing these attributes. The average person does not need them to have good back health. I address more advanced athletic training in detail in my book Ultimate Back Fitness and Performance (McGill, 2014). Begin with an assessment to understand the pain mechanisms. Then use the appropriate approach to address the mechanisms and build the person's tolerance and work capacity. Here is a summary of all five training stages:
- Stage 1: Establish quality movement engrams (motion patterns, motor patterns, and corrective exercise).
- Identify perturbed patterns and develop appropriate corrective exercise.
- Address basic movement patterns through to complex activity patterns.
- Address basic balance challenges through to complex and specific balance challenges.
- Stage 2: Build whole-body and joint stability (focus on spine stability here).
- Build stability while sparing the joints.
- Ensure sufficient stability commensurate with the demands of the task.
- Apply these patterns to the performance of daily activities.
- Stage 3: Increase endurance.
- Address basic endurance training to ensure the capacity needed for stabilization.
- Address activity-specific endurance (duration, intensity).
- Increase the ability to repeat pristine movement patterns without fatigue-induced compromise.
- Build the base for eventual performance training (only in those with this goal).
- Stage 4: Build strength.
- Spare the joints while maximizing the neuromuscular compartment challenge.
- Progress to skill movements.
- Stage 5: Develop speed, power, and agility.
- Develop ultimate performance based on the foundation laid in stages 1 through 4.
- Focus on optimizing elastic energy storage and recovery.
- Employ the techniques of superstiffness.
If you master the first three stages, which are discussed in this chapter, you will understand how to get bad backs to respond and how to develop better rehabilitation programs.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Models for measuring biological signals to assess risk
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Biological Signal - Driven Model Approaches
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Marras Model and McGill Model
The Marras model (Marras and Sommerich, 1991a, 1991b) measures electromyograms (EMGs) from several muscles and, using known physiological relationships, assigns forces to the muscles during virtually any industrial task. As noted earlier, this approach revealed powerful evidence linking the physical demands of specific occupational tasks with the incidence of LBD.
The McGill model (see chapter 1) uses the same philosophical approach to assign forces to the muscles, but attempts to include the highest level of anatomical accuracy possible. For example, it also measures three-dimensional spine curvature to assess forces to the passive tissues, including the intervertebral discs and the ligaments. By assigning forces to muscles and passive tissues throughout the full range of spine motion, it captures the ways people perform their jobs and even how they change with repetitions of the same jobs. The obvious liability of the approach is its enormous computational requirements, postprocessing of data, and difficulty collecting such comprehensive data from a wide number of workers in the field.
The question of the validity of this type of model must be addressed along with other models based on the biological approach. Some have argued that because these models contain known biomechanical and physiological relationships, they contain a certain amount of content validity. Moreover, both the Marras model and the McGill model have been quite successful in estimating the passive tissue and muscle forces that sum together to produce flexion and extension, lateral bend, and axial twisting moments. (These moments have been well predicted, with the exception of the twisting moment.) In summary, if twisting is not a dominant moment of force in a particular job, these models appear to predict accurate distributions of forces among the support tissues.
EMG-Assisted Optimization Approach
Perhaps the current pinnacle of model evolution is a hybrid modeling approach known as EMG-assisted optimization (developed by Cholewicki and McGill, 1994) with stability analysis and tissue load prediction (Cholewicki and McGill, 1996, was an early example, and Ikeda and McGill, 2012, is a more recent example). This approach exploits the asset of the biological EMG approach to distribute loads among the tissues based on the biological behavior of the subject. It then uses optimization to fine-tune the balancing of joint torques about several low back joints. The optimization takes the biologically predicted forces and adjusts muscle forces the minimal amount possible to satisfy the three-dimensional moment axes at every joint over the length of the lumbar spine. Once the three-dimensional moments have been assigned and tissue forces determined, an analysis of spine stability is performed via comparison of the joules of work imposed on the spine through perturbation with the joules of potential energy existing in the stiffened column.
This most highly evolved of spine models provides the biomechanist or ergonomist with insight into injury mechanisms caused by instability (as witnessed by Cholewicki and McGill, 1992) such as occurs while picking up a very light load from the floor. Even though patients have reported back injury from incidents such as bending over to tie a shoe, previous modeling approaches were sensitive only to tissue damage and injury scenarios produced from large loads and moments. Now a biomechanical explanation is available to explain the subsequent tissue damage, and a method is available to detect the risk of its happening. Although the routine use of this type of sophisticated model by ergonomists is not feasible, it is useful (for trained scientists) for analyzing individual workers and identifying those who are at elevated risk of injury because of faulty personal motor patterns.
Simple or Complex Models?
In summary, the complex models provide a tool to investigate the mechanisms of injury and the effects of technique during material handling on the risk of injury. The most complex and most highly evolved models provide insight into how injury occurs with all types of heavy and light loads. On the other hand, the simpler models, although sacrificing accuracy, can be powerful tools for the routine surveillance of physical demands in the workplace, but they must be wisely interpreted in each case given their limitations and constraints. Biomechanics and ergonomics require the full continuum of models. The choice of which one to use depends on the issue in question.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Postural tests for formal assessment
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit.
Formal Assessment of Posture
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit. Some tests are posturally based, whereas others assess control of motion.The following postural tests are very helpful. Recall that screening need not involve manipulation or special positions. Some of the most useful "tests" are simply intelligent observation.
Sitting Posture
Remarkably, patients with troubled backs often sit in a way that causes more back troubles. For example, patients who show flexion intolerance during provocative tests often have a typical sitting posture that involves a lot of spine flexion. In a similar way, those who show extension intolerance often sit with the spine locked into extension. The sitting posture is the first clue in hypothesis formation because this is often the posture that is first observed in the waiting area. Sitting in the waiting room in a flexed posture often suggests flexion intolerance.
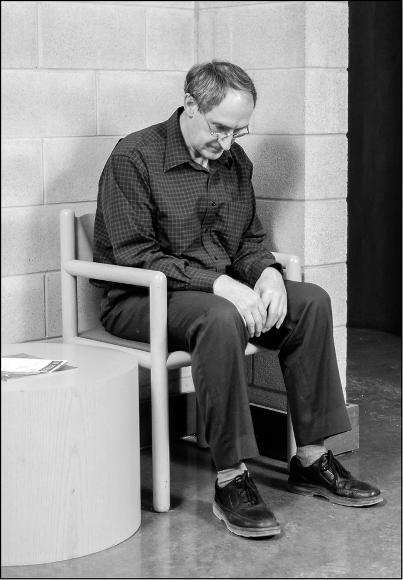
Photos from Stuart McGill
After noting the sitting posture, observe how the patient shifts from a slouched sitting posture to an upright one. Did she lift the rib cage, stressing the thoracolumbar junction ( a and b). Or did she flex the hips, rolling the pelvis forward to align the spine (c). Our recent work has shown that the best choice for most patients is to use a combination of the two (Castanhero et al., 2014) to minimize stress and avoid pain.
 |  |  |
Does the patient sit with a neutral spine (a) or a flexed spine (b)? When shifting from a slouch to a more upright posture, is the movement concentrated about the thoracolumbar junction or hips (c)?
Standing Pattern
All sorts of clues are revealed in the standing posture. Simple palpation of the standing patient's lumbar extensor muscles will reveal whether the patient is chronically crushing the back with extensor contraction. Simple postural corrections such as extending the hip, retracting the shoulders posteriorly, and pulling in the chin can shut these muscles off.
 |  |  |
|
Teach patients to palpate the erectors at the L3 level, and learn where the switch point is between muscle activation and muscle relaxation. They do this by standing upright, head erect and shoulders back, and then leaning forward slightly (a). Then they perfect this strategy to relax the muscle. Teach them that chin poking (b) and shoulder slouching (c) activate the muscles that cause fatigue cramps. Have them try the hitchhiking thumb position as a correction strategy, externally rotating the arms about the shoulders and then letting the shoulders relax into this new position (d).Having patients palpate the lumbar erectors helps them learn self-correcting strategies - are the erectors silent or active (a)? If they are active, show the patient how to shut them off by unloading the spine, which often provides immediate relief of muscular pain. Cues include shifting the head and neck from a chin poke to chin retraction position, adopting a hitchhiking posture with external rotation of the arms and shoulders, and pulling the hips forward (b, c).
 |  |  |
No amount of muscle relaxants will shut off the painful back muscles if the patient stands in a slouched posture. Standing to spare the spine requires a finely tuned blend of postural adjustments and muscle activation patterns. One correction is to steer the thumbs in external rotation, retracting the shoulders (see b and c) to a spine-sparing, corrected posture.
Some patients stand with no measurable extensor or abdominal muscle activation - they simply balance on their passive elastic spine tissues. These people tend to have thick torsos with flaccid abdominal walls. For these patients, pain reduction can be achieved with mild abdominal contraction; 2 or 3% of maximal voluntary contraction is considered normal abdominal wall muscle tone during standing (Juker et al., 1998).
Lying Pattern
Stress during lying is a function of body shape, the lying surface, and the pain mechanism. For back sleepers with protruding buttocks, lying on a hard surface causes a bridge under the lumbar spine. This causes spine flexion as the back flattens to the mattress and pain in the flexion-intolerant back. This may be addressed with support such as a folded towel (a, b). In a similar fashion, wide hips cause full, and painful, spine lateral bend in side-lying. In this case, a pillow-top surface can provide relief.
 |
|
(a-b) Painful backs with lying and sleeping postures are usually relieved with support to foster a neutral posture. This support may be in the form of mattress selection (adjusting firmness and the thickness of the pillow-top) or buttressing devices such as a folded towel in a person whose spine is bridged with protruding buttocks (a). A pillow to support the neck and knees may assist with side lying (b).
Learn more about Low Back Disorders, Third Edition With Web Resource.
Treatment isn't a recipe from a cookbook: Strategies for individualizing rehabilitation
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
Finding the Best Approach
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
- Encourage patients to train for health versus performance. The notion that athletes are healthy is generally a myth, at least from a musculoskeletal point of view. Training for superior athletic performance demands substantial overload of the muscles and tissues of the joints. An elevated risk of injury is associated with athletic training and performance. Unfortunately, many patients observe the routines used by athletes to enhance performance and wrongly conclude that copying them will help their own backs. Training for health requires quite a different philosophy; it emphasizes muscle endurance, motor control perfection, and the maintenance of sufficient spine stability in all expected tasks. Although strength is not a goal, strength gains do result. If a patient with back pain states that his objective is to play tennis or golf, then he has the wrong short-term objective. First and foremost, the objective is to eliminate pain. Then the objective may shift toward a performance objective such as participation in a sporting activity.
- Integrate prevention and rehabilitation approaches.The best therapy rigorously followed will not produce results if the cause of the back troubles is not addressed. Part II provided guidelines for reducing the risk of back troubles: the importance of removing the cause of tissue overload cannot be overstressed. Linton and van Tulder (2001) demonstrated the efficacy of exercise for prevention; exercise satisfies the objective for both better prevention and better rehabilitation outcomes. First, teach patients what is causing their troubles; then work with them to eliminate the cause.
- Work toward a slow, continuous improvement in function and pain reduction. The return of function and the reduction of pain, particularly for those with chronic bad backs, is a slow process. The typical pattern of recovery is akin to that of the stock market. Daily, and even weekly, price fluctuations eventually result in higher prices. Patients have good days and bad days. Many times lawyers have hired private investigators to make clandestine videos of people with back troubles performing tasks that appear inconsistent with those troubles. I am hired to provide comment. Some of these people are true malingerers and get caught. Others are simply having a good day when they are video-recorded. In such cases, I see all sorts of movement pathology consistent with their chronic history, and they are exonerated.
- Have the patient keep a journal of daily activities. Sometimes it is difficult to hone in on the pain mechanism and the correct dosage and exercise form. Examining daily pain and activity patterns can help identify the link with mechanical scenarios that exacerbate the pain. Two critical components should be recorded in a daily journal: how the back feels and what tasks and activities were performed. When patients encounter repeated setbacks, they should try to identify a common task or activity that preceded the pain episode. Likewise, even when progress is slow, patients should be encouraged to see some progress nonetheless. Without referring to the diary, patients sometimes do not realize that they are improving. Linking pain with a dose of activity is different from recording pain on a 10-point scale, which is typical of behavior modification programs. I have seen too many patients from these programs obsessing over their pain levels; for these people, we suggest stopping pain recording.
- Ensure a positive slope in progress. Chapters 10 and 11introduce the big three exercises in different forms. We designed these exercises to spare the spine from large loads and to groove stabilizing motor patterns. Use the three to establish a positive slope in patient improvement. Once the slope is established, you may choose to add new exercises one at a time. The patient may tolerate some exercises well and others not so well. If the improvement slope is lost after adding a new activity, remove it, go back to the big three, and reestablish the positive slope. If the patient requires advanced exercises for athletic performance, perhaps to increase spine mobility, you may add exercises to achieve such objectives after establishing the positive slope. How long should each stage be? There is no single answer for everyone. Some progress quickly, whereas others require great patience. Your job is to determine the initial challenge, to gauge progress and enhance the challenge accordingly, and to keep the patient motivated, even during periods of no apparent progress. The great clinicians blend keen clinical skills and experience with scientifically founded guidelines and knowledge.
- Determine whether the patient is willing to make a change. Obviously, the patient must change the current patterns that caused her to become a back patient. This requires motivation, which is not always easy to establish. Some have listed the importance of, and steps for developing, a change in motivation and attitude (e.g., Ranney, 1997). Briefly, such a program begins with the setting of goals - for example, returning to a specific job or partaking in a leisure activity. The employer's role in enhancing motivation is to ensure that modified work is available together with the opportunity for a graduated return to duty. Employers can also enhance motivation by fostering a culture in which worker success equates to company success, which in turn helps the worker. The second step in a motivation program is to formulate a realistic plan for reaching the goal established in the first step. It is beyond the mandate of this book to develop the components of maintaining and enhancing motivational opportunities at each stage of recovery.
- Determine whether the patient needs initial mobilization. Although everyone should incorporate spine stabilization exercises into daily activity, a small group of people will benefit from some directed soft tissue work (e.g., manipulation, trigger point therapy, Active Release Techniques, the use of foam rollers). These techniques are not the focus of this book. A word of caution is required here. Too many make the mistake of trying to mobilize a painful spine region that already has mobility. Nonetheless, there is good evidence that those with documented hypomobility may benefit from some initial manipulation or mobilization with a transition into stabilization training (Fritz, Whitman, and Childs, 2005).
- Consider other soft tissue treatments. A good manual medicine clinician may perceive local muscle spasms and odd-feeling local muscle texture. Further, these spasms and local neurocompartment disorders are associated with larger dysfunctions of the agonist and synergist muscles involved in a movement. In many cases these dysfunctions delay recovery or prevent complete recovery. Clinicians use a variety of soft tissue treatments to reduce spasm and release tissues that can impede attaining more normal muscular and joint function. Documenting them is beyond the scope of this book. We simply alert you to their potential significance and role in rehabilitation.
- Avoid spine power. Spine power is the product of velocity and force (power = force × velocity). This means that the spine is bending quickly and there is velocity in the muscles' lengthening and shortening. Techniques that involve high velocity in the spine have been shown to lead to back troubles, because they usually indicate high power (Marras et al., 1993; Stevenson et al., 2001). To minimize power and maximize safety, the forces transmitted through the trunk must be low if the spine is moving. If the forces transmitted through the trunk are high, then the velocity must be low. The power must be generated at the hips and shoulders and transmitted through an isometrically stabilized torso. Fortunately, this fundamental tenet for safety also helps to maximize performance.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Five stages to reduce back pain through exercise
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood.
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood. However, many more exercise-induced analgesic pathways are coming to light. One example is that exercise increases neurotrophin-3 production, which appears to have an analgesic role in cutaneous and deep tissue pan (Sharma et al., 2010).
Psychological components are important for some patients and influence the approach used to introduce and program exercise. For example, some patients obsess over their pain and what is going on in their bodies. Patients with high fear avoidance do better with physical therapy, which de-emphasizes anatomical findings (George et al., 2003). For these types of patients, I suggest not using daily pain charts, but directing their focus to achieving good exercise form. Some patients have back pain because they overload themselves with daily regimens at the gym. For the type A personality, we ensure that exercise is not overexecuted (for people who believe that 25 repetitions of an exercise will do them more good than the 10 that were prescribed). For the type B personality who may bargain with the clinician about doing less exercise, performing the exercise dose as prescribed should be encouraged. These two personality types require different approaches to prescribing exercise.
Some people have pain as a result of tissues that are inappropriately weak for the applied demands. In such cases the goal of exercise is to strengthen tissue, which requires a certain kind of programming. Athletes I have worked with who have recovered well from compression fractures have incorporated sufficient rest intervals to allow the injury to adapt between loading sessions. This appears to not work with collagenous disc injuries given the time required (years) for migrated nucleus material to gristle and form a plug (Adams and Dolan, 2005). Thus, the type of tissue that is the target for strengthening should determine the exercise approach.
Imbalances in joint and muscle function create odd stress patterns and more pain. For example, hip and back pain can cause gluteal muscle inhibition (Freeman, Mascia, and McGill, 2013), which makes the hamstring muscles dominant in creating hip extension moment. Because of the lines of action of these muscles, this causes more load on the anterior acetabulum and labrum of the hip (Lewis, Sahrmann, and Moran, 2009), resulting in associated hip pain.
There is also substantial support for the notion of the existence of a psychological profile associated with fitness - that is, that fitter people ignore small discomforts. As discussed in the section Why and How You Should Read This Book, fitness reduces the tendency to catastrophize pain.
How is the most appropriate exercise determined to reduce each of these pain mechanisms? Although the assessment will reveal the pain mechanism, many challenging patients must be considered experiments in progress. Tweaking the exercise form and the dosage helps you to hone in on the optimal.
Five-Stage Back Training Program
We have developed a five-stage approach to back training that begins with identifying faulty movement patterns and ends with pain-free performance readiness. Consider this the big picture, because only athletes and people who perform demanding tasks will complete all five stages. However, it is important to understand the components and objectives of each stage, as well as their order. For example, patients may be unknowingly following a strengthening regimen (stage 4) without having addressed perturbed motion patterns (stage 1). Doing so will delay their recovery, or make them worse. So when approaching the program, you must first ask, Is the objective pain reduction and rehabilitation or athletic performance? Health objectives demand a focus on motion and motor patterns, stability, and endurance to achieve low tissue loads and a low-risk environment. Performance requires more overload, which naturally results in an elevated risk. The trick in the case of performance is to stay within the lowest risk possible.
Although all five major stages are listed here, only the first three are appropriate for rehabilitation and addressed in this book. Rigorous strength, speed, and power training are only for those interested in enhancing these attributes. The average person does not need them to have good back health. I address more advanced athletic training in detail in my book Ultimate Back Fitness and Performance (McGill, 2014). Begin with an assessment to understand the pain mechanisms. Then use the appropriate approach to address the mechanisms and build the person's tolerance and work capacity. Here is a summary of all five training stages:
- Stage 1: Establish quality movement engrams (motion patterns, motor patterns, and corrective exercise).
- Identify perturbed patterns and develop appropriate corrective exercise.
- Address basic movement patterns through to complex activity patterns.
- Address basic balance challenges through to complex and specific balance challenges.
- Stage 2: Build whole-body and joint stability (focus on spine stability here).
- Build stability while sparing the joints.
- Ensure sufficient stability commensurate with the demands of the task.
- Apply these patterns to the performance of daily activities.
- Stage 3: Increase endurance.
- Address basic endurance training to ensure the capacity needed for stabilization.
- Address activity-specific endurance (duration, intensity).
- Increase the ability to repeat pristine movement patterns without fatigue-induced compromise.
- Build the base for eventual performance training (only in those with this goal).
- Stage 4: Build strength.
- Spare the joints while maximizing the neuromuscular compartment challenge.
- Progress to skill movements.
- Stage 5: Develop speed, power, and agility.
- Develop ultimate performance based on the foundation laid in stages 1 through 4.
- Focus on optimizing elastic energy storage and recovery.
- Employ the techniques of superstiffness.
If you master the first three stages, which are discussed in this chapter, you will understand how to get bad backs to respond and how to develop better rehabilitation programs.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Models for measuring biological signals to assess risk
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Biological Signal - Driven Model Approaches
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Marras Model and McGill Model
The Marras model (Marras and Sommerich, 1991a, 1991b) measures electromyograms (EMGs) from several muscles and, using known physiological relationships, assigns forces to the muscles during virtually any industrial task. As noted earlier, this approach revealed powerful evidence linking the physical demands of specific occupational tasks with the incidence of LBD.
The McGill model (see chapter 1) uses the same philosophical approach to assign forces to the muscles, but attempts to include the highest level of anatomical accuracy possible. For example, it also measures three-dimensional spine curvature to assess forces to the passive tissues, including the intervertebral discs and the ligaments. By assigning forces to muscles and passive tissues throughout the full range of spine motion, it captures the ways people perform their jobs and even how they change with repetitions of the same jobs. The obvious liability of the approach is its enormous computational requirements, postprocessing of data, and difficulty collecting such comprehensive data from a wide number of workers in the field.
The question of the validity of this type of model must be addressed along with other models based on the biological approach. Some have argued that because these models contain known biomechanical and physiological relationships, they contain a certain amount of content validity. Moreover, both the Marras model and the McGill model have been quite successful in estimating the passive tissue and muscle forces that sum together to produce flexion and extension, lateral bend, and axial twisting moments. (These moments have been well predicted, with the exception of the twisting moment.) In summary, if twisting is not a dominant moment of force in a particular job, these models appear to predict accurate distributions of forces among the support tissues.
EMG-Assisted Optimization Approach
Perhaps the current pinnacle of model evolution is a hybrid modeling approach known as EMG-assisted optimization (developed by Cholewicki and McGill, 1994) with stability analysis and tissue load prediction (Cholewicki and McGill, 1996, was an early example, and Ikeda and McGill, 2012, is a more recent example). This approach exploits the asset of the biological EMG approach to distribute loads among the tissues based on the biological behavior of the subject. It then uses optimization to fine-tune the balancing of joint torques about several low back joints. The optimization takes the biologically predicted forces and adjusts muscle forces the minimal amount possible to satisfy the three-dimensional moment axes at every joint over the length of the lumbar spine. Once the three-dimensional moments have been assigned and tissue forces determined, an analysis of spine stability is performed via comparison of the joules of work imposed on the spine through perturbation with the joules of potential energy existing in the stiffened column.
This most highly evolved of spine models provides the biomechanist or ergonomist with insight into injury mechanisms caused by instability (as witnessed by Cholewicki and McGill, 1992) such as occurs while picking up a very light load from the floor. Even though patients have reported back injury from incidents such as bending over to tie a shoe, previous modeling approaches were sensitive only to tissue damage and injury scenarios produced from large loads and moments. Now a biomechanical explanation is available to explain the subsequent tissue damage, and a method is available to detect the risk of its happening. Although the routine use of this type of sophisticated model by ergonomists is not feasible, it is useful (for trained scientists) for analyzing individual workers and identifying those who are at elevated risk of injury because of faulty personal motor patterns.
Simple or Complex Models?
In summary, the complex models provide a tool to investigate the mechanisms of injury and the effects of technique during material handling on the risk of injury. The most complex and most highly evolved models provide insight into how injury occurs with all types of heavy and light loads. On the other hand, the simpler models, although sacrificing accuracy, can be powerful tools for the routine surveillance of physical demands in the workplace, but they must be wisely interpreted in each case given their limitations and constraints. Biomechanics and ergonomics require the full continuum of models. The choice of which one to use depends on the issue in question.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Postural tests for formal assessment
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit.
Formal Assessment of Posture
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit. Some tests are posturally based, whereas others assess control of motion.The following postural tests are very helpful. Recall that screening need not involve manipulation or special positions. Some of the most useful "tests" are simply intelligent observation.
Sitting Posture
Remarkably, patients with troubled backs often sit in a way that causes more back troubles. For example, patients who show flexion intolerance during provocative tests often have a typical sitting posture that involves a lot of spine flexion. In a similar way, those who show extension intolerance often sit with the spine locked into extension. The sitting posture is the first clue in hypothesis formation because this is often the posture that is first observed in the waiting area. Sitting in the waiting room in a flexed posture often suggests flexion intolerance.
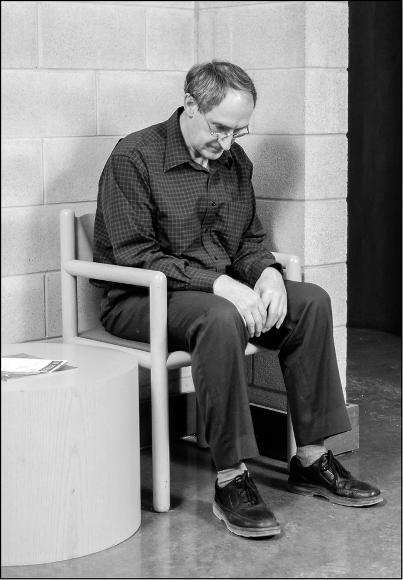
Photos from Stuart McGill
After noting the sitting posture, observe how the patient shifts from a slouched sitting posture to an upright one. Did she lift the rib cage, stressing the thoracolumbar junction ( a and b). Or did she flex the hips, rolling the pelvis forward to align the spine (c). Our recent work has shown that the best choice for most patients is to use a combination of the two (Castanhero et al., 2014) to minimize stress and avoid pain.
 |  |  |
Does the patient sit with a neutral spine (a) or a flexed spine (b)? When shifting from a slouch to a more upright posture, is the movement concentrated about the thoracolumbar junction or hips (c)?
Standing Pattern
All sorts of clues are revealed in the standing posture. Simple palpation of the standing patient's lumbar extensor muscles will reveal whether the patient is chronically crushing the back with extensor contraction. Simple postural corrections such as extending the hip, retracting the shoulders posteriorly, and pulling in the chin can shut these muscles off.
 |  |  |
|
Teach patients to palpate the erectors at the L3 level, and learn where the switch point is between muscle activation and muscle relaxation. They do this by standing upright, head erect and shoulders back, and then leaning forward slightly (a). Then they perfect this strategy to relax the muscle. Teach them that chin poking (b) and shoulder slouching (c) activate the muscles that cause fatigue cramps. Have them try the hitchhiking thumb position as a correction strategy, externally rotating the arms about the shoulders and then letting the shoulders relax into this new position (d).Having patients palpate the lumbar erectors helps them learn self-correcting strategies - are the erectors silent or active (a)? If they are active, show the patient how to shut them off by unloading the spine, which often provides immediate relief of muscular pain. Cues include shifting the head and neck from a chin poke to chin retraction position, adopting a hitchhiking posture with external rotation of the arms and shoulders, and pulling the hips forward (b, c).
 |  |  |
No amount of muscle relaxants will shut off the painful back muscles if the patient stands in a slouched posture. Standing to spare the spine requires a finely tuned blend of postural adjustments and muscle activation patterns. One correction is to steer the thumbs in external rotation, retracting the shoulders (see b and c) to a spine-sparing, corrected posture.
Some patients stand with no measurable extensor or abdominal muscle activation - they simply balance on their passive elastic spine tissues. These people tend to have thick torsos with flaccid abdominal walls. For these patients, pain reduction can be achieved with mild abdominal contraction; 2 or 3% of maximal voluntary contraction is considered normal abdominal wall muscle tone during standing (Juker et al., 1998).
Lying Pattern
Stress during lying is a function of body shape, the lying surface, and the pain mechanism. For back sleepers with protruding buttocks, lying on a hard surface causes a bridge under the lumbar spine. This causes spine flexion as the back flattens to the mattress and pain in the flexion-intolerant back. This may be addressed with support such as a folded towel (a, b). In a similar fashion, wide hips cause full, and painful, spine lateral bend in side-lying. In this case, a pillow-top surface can provide relief.
 |
|
(a-b) Painful backs with lying and sleeping postures are usually relieved with support to foster a neutral posture. This support may be in the form of mattress selection (adjusting firmness and the thickness of the pillow-top) or buttressing devices such as a folded towel in a person whose spine is bridged with protruding buttocks (a). A pillow to support the neck and knees may assist with side lying (b).
Learn more about Low Back Disorders, Third Edition With Web Resource.
Treatment isn't a recipe from a cookbook: Strategies for individualizing rehabilitation
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
Finding the Best Approach
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
- Encourage patients to train for health versus performance. The notion that athletes are healthy is generally a myth, at least from a musculoskeletal point of view. Training for superior athletic performance demands substantial overload of the muscles and tissues of the joints. An elevated risk of injury is associated with athletic training and performance. Unfortunately, many patients observe the routines used by athletes to enhance performance and wrongly conclude that copying them will help their own backs. Training for health requires quite a different philosophy; it emphasizes muscle endurance, motor control perfection, and the maintenance of sufficient spine stability in all expected tasks. Although strength is not a goal, strength gains do result. If a patient with back pain states that his objective is to play tennis or golf, then he has the wrong short-term objective. First and foremost, the objective is to eliminate pain. Then the objective may shift toward a performance objective such as participation in a sporting activity.
- Integrate prevention and rehabilitation approaches.The best therapy rigorously followed will not produce results if the cause of the back troubles is not addressed. Part II provided guidelines for reducing the risk of back troubles: the importance of removing the cause of tissue overload cannot be overstressed. Linton and van Tulder (2001) demonstrated the efficacy of exercise for prevention; exercise satisfies the objective for both better prevention and better rehabilitation outcomes. First, teach patients what is causing their troubles; then work with them to eliminate the cause.
- Work toward a slow, continuous improvement in function and pain reduction. The return of function and the reduction of pain, particularly for those with chronic bad backs, is a slow process. The typical pattern of recovery is akin to that of the stock market. Daily, and even weekly, price fluctuations eventually result in higher prices. Patients have good days and bad days. Many times lawyers have hired private investigators to make clandestine videos of people with back troubles performing tasks that appear inconsistent with those troubles. I am hired to provide comment. Some of these people are true malingerers and get caught. Others are simply having a good day when they are video-recorded. In such cases, I see all sorts of movement pathology consistent with their chronic history, and they are exonerated.
- Have the patient keep a journal of daily activities. Sometimes it is difficult to hone in on the pain mechanism and the correct dosage and exercise form. Examining daily pain and activity patterns can help identify the link with mechanical scenarios that exacerbate the pain. Two critical components should be recorded in a daily journal: how the back feels and what tasks and activities were performed. When patients encounter repeated setbacks, they should try to identify a common task or activity that preceded the pain episode. Likewise, even when progress is slow, patients should be encouraged to see some progress nonetheless. Without referring to the diary, patients sometimes do not realize that they are improving. Linking pain with a dose of activity is different from recording pain on a 10-point scale, which is typical of behavior modification programs. I have seen too many patients from these programs obsessing over their pain levels; for these people, we suggest stopping pain recording.
- Ensure a positive slope in progress. Chapters 10 and 11introduce the big three exercises in different forms. We designed these exercises to spare the spine from large loads and to groove stabilizing motor patterns. Use the three to establish a positive slope in patient improvement. Once the slope is established, you may choose to add new exercises one at a time. The patient may tolerate some exercises well and others not so well. If the improvement slope is lost after adding a new activity, remove it, go back to the big three, and reestablish the positive slope. If the patient requires advanced exercises for athletic performance, perhaps to increase spine mobility, you may add exercises to achieve such objectives after establishing the positive slope. How long should each stage be? There is no single answer for everyone. Some progress quickly, whereas others require great patience. Your job is to determine the initial challenge, to gauge progress and enhance the challenge accordingly, and to keep the patient motivated, even during periods of no apparent progress. The great clinicians blend keen clinical skills and experience with scientifically founded guidelines and knowledge.
- Determine whether the patient is willing to make a change. Obviously, the patient must change the current patterns that caused her to become a back patient. This requires motivation, which is not always easy to establish. Some have listed the importance of, and steps for developing, a change in motivation and attitude (e.g., Ranney, 1997). Briefly, such a program begins with the setting of goals - for example, returning to a specific job or partaking in a leisure activity. The employer's role in enhancing motivation is to ensure that modified work is available together with the opportunity for a graduated return to duty. Employers can also enhance motivation by fostering a culture in which worker success equates to company success, which in turn helps the worker. The second step in a motivation program is to formulate a realistic plan for reaching the goal established in the first step. It is beyond the mandate of this book to develop the components of maintaining and enhancing motivational opportunities at each stage of recovery.
- Determine whether the patient needs initial mobilization. Although everyone should incorporate spine stabilization exercises into daily activity, a small group of people will benefit from some directed soft tissue work (e.g., manipulation, trigger point therapy, Active Release Techniques, the use of foam rollers). These techniques are not the focus of this book. A word of caution is required here. Too many make the mistake of trying to mobilize a painful spine region that already has mobility. Nonetheless, there is good evidence that those with documented hypomobility may benefit from some initial manipulation or mobilization with a transition into stabilization training (Fritz, Whitman, and Childs, 2005).
- Consider other soft tissue treatments. A good manual medicine clinician may perceive local muscle spasms and odd-feeling local muscle texture. Further, these spasms and local neurocompartment disorders are associated with larger dysfunctions of the agonist and synergist muscles involved in a movement. In many cases these dysfunctions delay recovery or prevent complete recovery. Clinicians use a variety of soft tissue treatments to reduce spasm and release tissues that can impede attaining more normal muscular and joint function. Documenting them is beyond the scope of this book. We simply alert you to their potential significance and role in rehabilitation.
- Avoid spine power. Spine power is the product of velocity and force (power = force × velocity). This means that the spine is bending quickly and there is velocity in the muscles' lengthening and shortening. Techniques that involve high velocity in the spine have been shown to lead to back troubles, because they usually indicate high power (Marras et al., 1993; Stevenson et al., 2001). To minimize power and maximize safety, the forces transmitted through the trunk must be low if the spine is moving. If the forces transmitted through the trunk are high, then the velocity must be low. The power must be generated at the hips and shoulders and transmitted through an isometrically stabilized torso. Fortunately, this fundamental tenet for safety also helps to maximize performance.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Five stages to reduce back pain through exercise
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood.
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood. However, many more exercise-induced analgesic pathways are coming to light. One example is that exercise increases neurotrophin-3 production, which appears to have an analgesic role in cutaneous and deep tissue pan (Sharma et al., 2010).
Psychological components are important for some patients and influence the approach used to introduce and program exercise. For example, some patients obsess over their pain and what is going on in their bodies. Patients with high fear avoidance do better with physical therapy, which de-emphasizes anatomical findings (George et al., 2003). For these types of patients, I suggest not using daily pain charts, but directing their focus to achieving good exercise form. Some patients have back pain because they overload themselves with daily regimens at the gym. For the type A personality, we ensure that exercise is not overexecuted (for people who believe that 25 repetitions of an exercise will do them more good than the 10 that were prescribed). For the type B personality who may bargain with the clinician about doing less exercise, performing the exercise dose as prescribed should be encouraged. These two personality types require different approaches to prescribing exercise.
Some people have pain as a result of tissues that are inappropriately weak for the applied demands. In such cases the goal of exercise is to strengthen tissue, which requires a certain kind of programming. Athletes I have worked with who have recovered well from compression fractures have incorporated sufficient rest intervals to allow the injury to adapt between loading sessions. This appears to not work with collagenous disc injuries given the time required (years) for migrated nucleus material to gristle and form a plug (Adams and Dolan, 2005). Thus, the type of tissue that is the target for strengthening should determine the exercise approach.
Imbalances in joint and muscle function create odd stress patterns and more pain. For example, hip and back pain can cause gluteal muscle inhibition (Freeman, Mascia, and McGill, 2013), which makes the hamstring muscles dominant in creating hip extension moment. Because of the lines of action of these muscles, this causes more load on the anterior acetabulum and labrum of the hip (Lewis, Sahrmann, and Moran, 2009), resulting in associated hip pain.
There is also substantial support for the notion of the existence of a psychological profile associated with fitness - that is, that fitter people ignore small discomforts. As discussed in the section Why and How You Should Read This Book, fitness reduces the tendency to catastrophize pain.
How is the most appropriate exercise determined to reduce each of these pain mechanisms? Although the assessment will reveal the pain mechanism, many challenging patients must be considered experiments in progress. Tweaking the exercise form and the dosage helps you to hone in on the optimal.
Five-Stage Back Training Program
We have developed a five-stage approach to back training that begins with identifying faulty movement patterns and ends with pain-free performance readiness. Consider this the big picture, because only athletes and people who perform demanding tasks will complete all five stages. However, it is important to understand the components and objectives of each stage, as well as their order. For example, patients may be unknowingly following a strengthening regimen (stage 4) without having addressed perturbed motion patterns (stage 1). Doing so will delay their recovery, or make them worse. So when approaching the program, you must first ask, Is the objective pain reduction and rehabilitation or athletic performance? Health objectives demand a focus on motion and motor patterns, stability, and endurance to achieve low tissue loads and a low-risk environment. Performance requires more overload, which naturally results in an elevated risk. The trick in the case of performance is to stay within the lowest risk possible.
Although all five major stages are listed here, only the first three are appropriate for rehabilitation and addressed in this book. Rigorous strength, speed, and power training are only for those interested in enhancing these attributes. The average person does not need them to have good back health. I address more advanced athletic training in detail in my book Ultimate Back Fitness and Performance (McGill, 2014). Begin with an assessment to understand the pain mechanisms. Then use the appropriate approach to address the mechanisms and build the person's tolerance and work capacity. Here is a summary of all five training stages:
- Stage 1: Establish quality movement engrams (motion patterns, motor patterns, and corrective exercise).
- Identify perturbed patterns and develop appropriate corrective exercise.
- Address basic movement patterns through to complex activity patterns.
- Address basic balance challenges through to complex and specific balance challenges.
- Stage 2: Build whole-body and joint stability (focus on spine stability here).
- Build stability while sparing the joints.
- Ensure sufficient stability commensurate with the demands of the task.
- Apply these patterns to the performance of daily activities.
- Stage 3: Increase endurance.
- Address basic endurance training to ensure the capacity needed for stabilization.
- Address activity-specific endurance (duration, intensity).
- Increase the ability to repeat pristine movement patterns without fatigue-induced compromise.
- Build the base for eventual performance training (only in those with this goal).
- Stage 4: Build strength.
- Spare the joints while maximizing the neuromuscular compartment challenge.
- Progress to skill movements.
- Stage 5: Develop speed, power, and agility.
- Develop ultimate performance based on the foundation laid in stages 1 through 4.
- Focus on optimizing elastic energy storage and recovery.
- Employ the techniques of superstiffness.
If you master the first three stages, which are discussed in this chapter, you will understand how to get bad backs to respond and how to develop better rehabilitation programs.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Models for measuring biological signals to assess risk
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Biological Signal - Driven Model Approaches
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Marras Model and McGill Model
The Marras model (Marras and Sommerich, 1991a, 1991b) measures electromyograms (EMGs) from several muscles and, using known physiological relationships, assigns forces to the muscles during virtually any industrial task. As noted earlier, this approach revealed powerful evidence linking the physical demands of specific occupational tasks with the incidence of LBD.
The McGill model (see chapter 1) uses the same philosophical approach to assign forces to the muscles, but attempts to include the highest level of anatomical accuracy possible. For example, it also measures three-dimensional spine curvature to assess forces to the passive tissues, including the intervertebral discs and the ligaments. By assigning forces to muscles and passive tissues throughout the full range of spine motion, it captures the ways people perform their jobs and even how they change with repetitions of the same jobs. The obvious liability of the approach is its enormous computational requirements, postprocessing of data, and difficulty collecting such comprehensive data from a wide number of workers in the field.
The question of the validity of this type of model must be addressed along with other models based on the biological approach. Some have argued that because these models contain known biomechanical and physiological relationships, they contain a certain amount of content validity. Moreover, both the Marras model and the McGill model have been quite successful in estimating the passive tissue and muscle forces that sum together to produce flexion and extension, lateral bend, and axial twisting moments. (These moments have been well predicted, with the exception of the twisting moment.) In summary, if twisting is not a dominant moment of force in a particular job, these models appear to predict accurate distributions of forces among the support tissues.
EMG-Assisted Optimization Approach
Perhaps the current pinnacle of model evolution is a hybrid modeling approach known as EMG-assisted optimization (developed by Cholewicki and McGill, 1994) with stability analysis and tissue load prediction (Cholewicki and McGill, 1996, was an early example, and Ikeda and McGill, 2012, is a more recent example). This approach exploits the asset of the biological EMG approach to distribute loads among the tissues based on the biological behavior of the subject. It then uses optimization to fine-tune the balancing of joint torques about several low back joints. The optimization takes the biologically predicted forces and adjusts muscle forces the minimal amount possible to satisfy the three-dimensional moment axes at every joint over the length of the lumbar spine. Once the three-dimensional moments have been assigned and tissue forces determined, an analysis of spine stability is performed via comparison of the joules of work imposed on the spine through perturbation with the joules of potential energy existing in the stiffened column.
This most highly evolved of spine models provides the biomechanist or ergonomist with insight into injury mechanisms caused by instability (as witnessed by Cholewicki and McGill, 1992) such as occurs while picking up a very light load from the floor. Even though patients have reported back injury from incidents such as bending over to tie a shoe, previous modeling approaches were sensitive only to tissue damage and injury scenarios produced from large loads and moments. Now a biomechanical explanation is available to explain the subsequent tissue damage, and a method is available to detect the risk of its happening. Although the routine use of this type of sophisticated model by ergonomists is not feasible, it is useful (for trained scientists) for analyzing individual workers and identifying those who are at elevated risk of injury because of faulty personal motor patterns.
Simple or Complex Models?
In summary, the complex models provide a tool to investigate the mechanisms of injury and the effects of technique during material handling on the risk of injury. The most complex and most highly evolved models provide insight into how injury occurs with all types of heavy and light loads. On the other hand, the simpler models, although sacrificing accuracy, can be powerful tools for the routine surveillance of physical demands in the workplace, but they must be wisely interpreted in each case given their limitations and constraints. Biomechanics and ergonomics require the full continuum of models. The choice of which one to use depends on the issue in question.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Postural tests for formal assessment
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit.
Formal Assessment of Posture
A formal assessment of posture includes an assessment of sitting, standing, and lying. Pain is present because the back is currently a weak link. Functional tests help to sort out why the back is a weak link and help indicate what is required to bolster the deficit. Some tests are posturally based, whereas others assess control of motion.The following postural tests are very helpful. Recall that screening need not involve manipulation or special positions. Some of the most useful "tests" are simply intelligent observation.
Sitting Posture
Remarkably, patients with troubled backs often sit in a way that causes more back troubles. For example, patients who show flexion intolerance during provocative tests often have a typical sitting posture that involves a lot of spine flexion. In a similar way, those who show extension intolerance often sit with the spine locked into extension. The sitting posture is the first clue in hypothesis formation because this is often the posture that is first observed in the waiting area. Sitting in the waiting room in a flexed posture often suggests flexion intolerance.
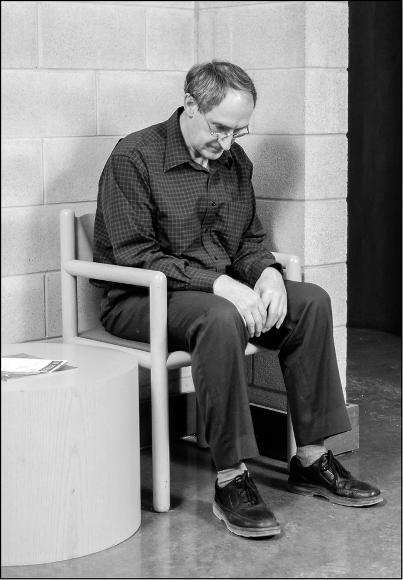
Photos from Stuart McGill
After noting the sitting posture, observe how the patient shifts from a slouched sitting posture to an upright one. Did she lift the rib cage, stressing the thoracolumbar junction ( a and b). Or did she flex the hips, rolling the pelvis forward to align the spine (c). Our recent work has shown that the best choice for most patients is to use a combination of the two (Castanhero et al., 2014) to minimize stress and avoid pain.
 |  |  |
Does the patient sit with a neutral spine (a) or a flexed spine (b)? When shifting from a slouch to a more upright posture, is the movement concentrated about the thoracolumbar junction or hips (c)?
Standing Pattern
All sorts of clues are revealed in the standing posture. Simple palpation of the standing patient's lumbar extensor muscles will reveal whether the patient is chronically crushing the back with extensor contraction. Simple postural corrections such as extending the hip, retracting the shoulders posteriorly, and pulling in the chin can shut these muscles off.
 |  |  |
|
Teach patients to palpate the erectors at the L3 level, and learn where the switch point is between muscle activation and muscle relaxation. They do this by standing upright, head erect and shoulders back, and then leaning forward slightly (a). Then they perfect this strategy to relax the muscle. Teach them that chin poking (b) and shoulder slouching (c) activate the muscles that cause fatigue cramps. Have them try the hitchhiking thumb position as a correction strategy, externally rotating the arms about the shoulders and then letting the shoulders relax into this new position (d).Having patients palpate the lumbar erectors helps them learn self-correcting strategies - are the erectors silent or active (a)? If they are active, show the patient how to shut them off by unloading the spine, which often provides immediate relief of muscular pain. Cues include shifting the head and neck from a chin poke to chin retraction position, adopting a hitchhiking posture with external rotation of the arms and shoulders, and pulling the hips forward (b, c).
 |  |  |
No amount of muscle relaxants will shut off the painful back muscles if the patient stands in a slouched posture. Standing to spare the spine requires a finely tuned blend of postural adjustments and muscle activation patterns. One correction is to steer the thumbs in external rotation, retracting the shoulders (see b and c) to a spine-sparing, corrected posture.
Some patients stand with no measurable extensor or abdominal muscle activation - they simply balance on their passive elastic spine tissues. These people tend to have thick torsos with flaccid abdominal walls. For these patients, pain reduction can be achieved with mild abdominal contraction; 2 or 3% of maximal voluntary contraction is considered normal abdominal wall muscle tone during standing (Juker et al., 1998).
Lying Pattern
Stress during lying is a function of body shape, the lying surface, and the pain mechanism. For back sleepers with protruding buttocks, lying on a hard surface causes a bridge under the lumbar spine. This causes spine flexion as the back flattens to the mattress and pain in the flexion-intolerant back. This may be addressed with support such as a folded towel (a, b). In a similar fashion, wide hips cause full, and painful, spine lateral bend in side-lying. In this case, a pillow-top surface can provide relief.
 |
|
(a-b) Painful backs with lying and sleeping postures are usually relieved with support to foster a neutral posture. This support may be in the form of mattress selection (adjusting firmness and the thickness of the pillow-top) or buttressing devices such as a folded towel in a person whose spine is bridged with protruding buttocks (a). A pillow to support the neck and knees may assist with side lying (b).
Learn more about Low Back Disorders, Third Edition With Web Resource.
Treatment isn't a recipe from a cookbook: Strategies for individualizing rehabilitation
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
Finding the Best Approach
Given the wide variety of patients with low back issues, we cannot expect to succeed in low back rehabilitation by treating everyone with the same cookbook program. The following strategies will help guide clinical decisions to individualize - and thus optimize - the rehabilitation program.
- Encourage patients to train for health versus performance. The notion that athletes are healthy is generally a myth, at least from a musculoskeletal point of view. Training for superior athletic performance demands substantial overload of the muscles and tissues of the joints. An elevated risk of injury is associated with athletic training and performance. Unfortunately, many patients observe the routines used by athletes to enhance performance and wrongly conclude that copying them will help their own backs. Training for health requires quite a different philosophy; it emphasizes muscle endurance, motor control perfection, and the maintenance of sufficient spine stability in all expected tasks. Although strength is not a goal, strength gains do result. If a patient with back pain states that his objective is to play tennis or golf, then he has the wrong short-term objective. First and foremost, the objective is to eliminate pain. Then the objective may shift toward a performance objective such as participation in a sporting activity.
- Integrate prevention and rehabilitation approaches.The best therapy rigorously followed will not produce results if the cause of the back troubles is not addressed. Part II provided guidelines for reducing the risk of back troubles: the importance of removing the cause of tissue overload cannot be overstressed. Linton and van Tulder (2001) demonstrated the efficacy of exercise for prevention; exercise satisfies the objective for both better prevention and better rehabilitation outcomes. First, teach patients what is causing their troubles; then work with them to eliminate the cause.
- Work toward a slow, continuous improvement in function and pain reduction. The return of function and the reduction of pain, particularly for those with chronic bad backs, is a slow process. The typical pattern of recovery is akin to that of the stock market. Daily, and even weekly, price fluctuations eventually result in higher prices. Patients have good days and bad days. Many times lawyers have hired private investigators to make clandestine videos of people with back troubles performing tasks that appear inconsistent with those troubles. I am hired to provide comment. Some of these people are true malingerers and get caught. Others are simply having a good day when they are video-recorded. In such cases, I see all sorts of movement pathology consistent with their chronic history, and they are exonerated.
- Have the patient keep a journal of daily activities. Sometimes it is difficult to hone in on the pain mechanism and the correct dosage and exercise form. Examining daily pain and activity patterns can help identify the link with mechanical scenarios that exacerbate the pain. Two critical components should be recorded in a daily journal: how the back feels and what tasks and activities were performed. When patients encounter repeated setbacks, they should try to identify a common task or activity that preceded the pain episode. Likewise, even when progress is slow, patients should be encouraged to see some progress nonetheless. Without referring to the diary, patients sometimes do not realize that they are improving. Linking pain with a dose of activity is different from recording pain on a 10-point scale, which is typical of behavior modification programs. I have seen too many patients from these programs obsessing over their pain levels; for these people, we suggest stopping pain recording.
- Ensure a positive slope in progress. Chapters 10 and 11introduce the big three exercises in different forms. We designed these exercises to spare the spine from large loads and to groove stabilizing motor patterns. Use the three to establish a positive slope in patient improvement. Once the slope is established, you may choose to add new exercises one at a time. The patient may tolerate some exercises well and others not so well. If the improvement slope is lost after adding a new activity, remove it, go back to the big three, and reestablish the positive slope. If the patient requires advanced exercises for athletic performance, perhaps to increase spine mobility, you may add exercises to achieve such objectives after establishing the positive slope. How long should each stage be? There is no single answer for everyone. Some progress quickly, whereas others require great patience. Your job is to determine the initial challenge, to gauge progress and enhance the challenge accordingly, and to keep the patient motivated, even during periods of no apparent progress. The great clinicians blend keen clinical skills and experience with scientifically founded guidelines and knowledge.
- Determine whether the patient is willing to make a change. Obviously, the patient must change the current patterns that caused her to become a back patient. This requires motivation, which is not always easy to establish. Some have listed the importance of, and steps for developing, a change in motivation and attitude (e.g., Ranney, 1997). Briefly, such a program begins with the setting of goals - for example, returning to a specific job or partaking in a leisure activity. The employer's role in enhancing motivation is to ensure that modified work is available together with the opportunity for a graduated return to duty. Employers can also enhance motivation by fostering a culture in which worker success equates to company success, which in turn helps the worker. The second step in a motivation program is to formulate a realistic plan for reaching the goal established in the first step. It is beyond the mandate of this book to develop the components of maintaining and enhancing motivational opportunities at each stage of recovery.
- Determine whether the patient needs initial mobilization. Although everyone should incorporate spine stabilization exercises into daily activity, a small group of people will benefit from some directed soft tissue work (e.g., manipulation, trigger point therapy, Active Release Techniques, the use of foam rollers). These techniques are not the focus of this book. A word of caution is required here. Too many make the mistake of trying to mobilize a painful spine region that already has mobility. Nonetheless, there is good evidence that those with documented hypomobility may benefit from some initial manipulation or mobilization with a transition into stabilization training (Fritz, Whitman, and Childs, 2005).
- Consider other soft tissue treatments. A good manual medicine clinician may perceive local muscle spasms and odd-feeling local muscle texture. Further, these spasms and local neurocompartment disorders are associated with larger dysfunctions of the agonist and synergist muscles involved in a movement. In many cases these dysfunctions delay recovery or prevent complete recovery. Clinicians use a variety of soft tissue treatments to reduce spasm and release tissues that can impede attaining more normal muscular and joint function. Documenting them is beyond the scope of this book. We simply alert you to their potential significance and role in rehabilitation.
- Avoid spine power. Spine power is the product of velocity and force (power = force × velocity). This means that the spine is bending quickly and there is velocity in the muscles' lengthening and shortening. Techniques that involve high velocity in the spine have been shown to lead to back troubles, because they usually indicate high power (Marras et al., 1993; Stevenson et al., 2001). To minimize power and maximize safety, the forces transmitted through the trunk must be low if the spine is moving. If the forces transmitted through the trunk are high, then the velocity must be low. The power must be generated at the hips and shoulders and transmitted through an isometrically stabilized torso. Fortunately, this fundamental tenet for safety also helps to maximize performance.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Five stages to reduce back pain through exercise
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood.
Neurophysiological mechanisms of pain are highly modulated by movement and exercise. Endorphin release has long been known to occur with exercise, but the molecular basis for these links is not well understood. However, many more exercise-induced analgesic pathways are coming to light. One example is that exercise increases neurotrophin-3 production, which appears to have an analgesic role in cutaneous and deep tissue pan (Sharma et al., 2010).
Psychological components are important for some patients and influence the approach used to introduce and program exercise. For example, some patients obsess over their pain and what is going on in their bodies. Patients with high fear avoidance do better with physical therapy, which de-emphasizes anatomical findings (George et al., 2003). For these types of patients, I suggest not using daily pain charts, but directing their focus to achieving good exercise form. Some patients have back pain because they overload themselves with daily regimens at the gym. For the type A personality, we ensure that exercise is not overexecuted (for people who believe that 25 repetitions of an exercise will do them more good than the 10 that were prescribed). For the type B personality who may bargain with the clinician about doing less exercise, performing the exercise dose as prescribed should be encouraged. These two personality types require different approaches to prescribing exercise.
Some people have pain as a result of tissues that are inappropriately weak for the applied demands. In such cases the goal of exercise is to strengthen tissue, which requires a certain kind of programming. Athletes I have worked with who have recovered well from compression fractures have incorporated sufficient rest intervals to allow the injury to adapt between loading sessions. This appears to not work with collagenous disc injuries given the time required (years) for migrated nucleus material to gristle and form a plug (Adams and Dolan, 2005). Thus, the type of tissue that is the target for strengthening should determine the exercise approach.
Imbalances in joint and muscle function create odd stress patterns and more pain. For example, hip and back pain can cause gluteal muscle inhibition (Freeman, Mascia, and McGill, 2013), which makes the hamstring muscles dominant in creating hip extension moment. Because of the lines of action of these muscles, this causes more load on the anterior acetabulum and labrum of the hip (Lewis, Sahrmann, and Moran, 2009), resulting in associated hip pain.
There is also substantial support for the notion of the existence of a psychological profile associated with fitness - that is, that fitter people ignore small discomforts. As discussed in the section Why and How You Should Read This Book, fitness reduces the tendency to catastrophize pain.
How is the most appropriate exercise determined to reduce each of these pain mechanisms? Although the assessment will reveal the pain mechanism, many challenging patients must be considered experiments in progress. Tweaking the exercise form and the dosage helps you to hone in on the optimal.
Five-Stage Back Training Program
We have developed a five-stage approach to back training that begins with identifying faulty movement patterns and ends with pain-free performance readiness. Consider this the big picture, because only athletes and people who perform demanding tasks will complete all five stages. However, it is important to understand the components and objectives of each stage, as well as their order. For example, patients may be unknowingly following a strengthening regimen (stage 4) without having addressed perturbed motion patterns (stage 1). Doing so will delay their recovery, or make them worse. So when approaching the program, you must first ask, Is the objective pain reduction and rehabilitation or athletic performance? Health objectives demand a focus on motion and motor patterns, stability, and endurance to achieve low tissue loads and a low-risk environment. Performance requires more overload, which naturally results in an elevated risk. The trick in the case of performance is to stay within the lowest risk possible.
Although all five major stages are listed here, only the first three are appropriate for rehabilitation and addressed in this book. Rigorous strength, speed, and power training are only for those interested in enhancing these attributes. The average person does not need them to have good back health. I address more advanced athletic training in detail in my book Ultimate Back Fitness and Performance (McGill, 2014). Begin with an assessment to understand the pain mechanisms. Then use the appropriate approach to address the mechanisms and build the person's tolerance and work capacity. Here is a summary of all five training stages:
- Stage 1: Establish quality movement engrams (motion patterns, motor patterns, and corrective exercise).
- Identify perturbed patterns and develop appropriate corrective exercise.
- Address basic movement patterns through to complex activity patterns.
- Address basic balance challenges through to complex and specific balance challenges.
- Stage 2: Build whole-body and joint stability (focus on spine stability here).
- Build stability while sparing the joints.
- Ensure sufficient stability commensurate with the demands of the task.
- Apply these patterns to the performance of daily activities.
- Stage 3: Increase endurance.
- Address basic endurance training to ensure the capacity needed for stabilization.
- Address activity-specific endurance (duration, intensity).
- Increase the ability to repeat pristine movement patterns without fatigue-induced compromise.
- Build the base for eventual performance training (only in those with this goal).
- Stage 4: Build strength.
- Spare the joints while maximizing the neuromuscular compartment challenge.
- Progress to skill movements.
- Stage 5: Develop speed, power, and agility.
- Develop ultimate performance based on the foundation laid in stages 1 through 4.
- Focus on optimizing elastic energy storage and recovery.
- Employ the techniques of superstiffness.
If you master the first three stages, which are discussed in this chapter, you will understand how to get bad backs to respond and how to develop better rehabilitation programs.
Learn more about Low Back Disorders, Third Edition With Web Resource.
Models for measuring biological signals to assess risk
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Biological Signal - Driven Model Approaches
The final approach for risk assessment is to measure biological signals from each subject to capture the unique ways people perform their jobs and then use sophisticated anatomical, biomechanical, and physiological relationships to assign forces to the tissues.
Marras Model and McGill Model
The Marras model (Marras and Sommerich, 1991a, 1991b) measures electromyograms (EMGs) from several muscles and, using known physiological relationships, assigns forces to the muscles during virtually any industrial task. As noted earlier, this approach revealed powerful evidence linking the physical demands of specific occupational tasks with the incidence of LBD.
The McGill model (see chapter 1) uses the same philosophical approach to assign forces to the muscles, but attempts to include the highest level of anatomical accuracy possible. For example, it also measures three-dimensional spine curvature to assess forces to the passive tissues, including the intervertebral discs and the ligaments. By assigning forces to muscles and passive tissues throughout the full range of spine motion, it captures the ways people perform their jobs and even how they change with repetitions of the same jobs. The obvious liability of the approach is its enormous computational requirements, postprocessing of data, and difficulty collecting such comprehensive data from a wide number of workers in the field.
The question of the validity of this type of model must be addressed along with other models based on the biological approach. Some have argued that because these models contain known biomechanical and physiological relationships, they contain a certain amount of content validity. Moreover, both the Marras model and the McGill model have been quite successful in estimating the passive tissue and muscle forces that sum together to produce flexion and extension, lateral bend, and axial twisting moments. (These moments have been well predicted, with the exception of the twisting moment.) In summary, if twisting is not a dominant moment of force in a particular job, these models appear to predict accurate distributions of forces among the support tissues.
EMG-Assisted Optimization Approach
Perhaps the current pinnacle of model evolution is a hybrid modeling approach known as EMG-assisted optimization (developed by Cholewicki and McGill, 1994) with stability analysis and tissue load prediction (Cholewicki and McGill, 1996, was an early example, and Ikeda and McGill, 2012, is a more recent example). This approach exploits the asset of the biological EMG approach to distribute loads among the tissues based on the biological behavior of the subject. It then uses optimization to fine-tune the balancing of joint torques about several low back joints. The optimization takes the biologically predicted forces and adjusts muscle forces the minimal amount possible to satisfy the three-dimensional moment axes at every joint over the length of the lumbar spine. Once the three-dimensional moments have been assigned and tissue forces determined, an analysis of spine stability is performed via comparison of the joules of work imposed on the spine through perturbation with the joules of potential energy existing in the stiffened column.
This most highly evolved of spine models provides the biomechanist or ergonomist with insight into injury mechanisms caused by instability (as witnessed by Cholewicki and McGill, 1992) such as occurs while picking up a very light load from the floor. Even though patients have reported back injury from incidents such as bending over to tie a shoe, previous modeling approaches were sensitive only to tissue damage and injury scenarios produced from large loads and moments. Now a biomechanical explanation is available to explain the subsequent tissue damage, and a method is available to detect the risk of its happening. Although the routine use of this type of sophisticated model by ergonomists is not feasible, it is useful (for trained scientists) for analyzing individual workers and identifying those who are at elevated risk of injury because of faulty personal motor patterns.
Simple or Complex Models?
In summary, the complex models provide a tool to investigate the mechanisms of injury and the effects of technique during material handling on the risk of injury. The most complex and most highly evolved models provide insight into how injury occurs with all types of heavy and light loads. On the other hand, the simpler models, although sacrificing accuracy, can be powerful tools for the routine surveillance of physical demands in the workplace, but they must be wisely interpreted in each case given their limitations and constraints. Biomechanics and ergonomics require the full continuum of models. The choice of which one to use depends on the issue in question.
Learn more about Low Back Disorders, Third Edition With Web Resource.