- Home
- Physical Therapy/Physiotherapy
- Medicine in Exercise and Sport
- Health Care in Exercise and Sport
- Sports Injuries Guidebook

Dr. Robert Gotlin, a former medical consultant to the New York Knicks, the New York Liberty, the New York Yankees, and the New Jersey Nets, has assembled 24 top specialists in sports medicine to create an authoritative guide covering more than 150 common sports injuries, including the following:
- Concussions
- Rotator cuff tears
- Knee injuries
- Bone fractures
- Ligament sprains
- Muscle strains and tears
- IT band syndrome
- Shin splits
This second edition also features new chapters explaining how and why injuries happen, as well as different types of injection therapies and when they may be most beneficial. You’ll also learn how to prevent injuries from occurring in the first place with proper conditioning, body maintenance, and nutrition.
With high-quality illustrations and a user-friendly format, Sports Injuries Guidebook will arm you with the expert guidance you need to understand injuries and get back in the game.
Adam Gotlin
Chapter 2. Body Maintenance, Conditioning, Strengthening, and Injury Prevention
Jeff Young
Chapter 3. Injury Types, Assessment, and Management
Matthew Gotlin and Laith Jazrawi
Chapter 4. Concussions and Head Injuries
Josh Krassen
Chapter 5. Neck and Cervical Spine Injuries
Richard Goldberg
Chapter 6. Shoulder Injuries
Edmund S. Evangelista
Chapter 7. Arm and Elbow Injuries
Andrew L. Sherman and Jesse N. Charnoff
Chapter 8. Wrist and Hand Injuries
Steven Beldner, Marcel A. Bas, and Daniel B. Polatsch
Chapter 9. Chest and Abdominal Injuries
David Perna
Chapter 10. Back Injuries
Joseph Lee
Chapter 11. Hip Injuries
Michael M. Weinik, Reed C. Williams, and Ilya Igolnikov
Chapter 12. Thigh and Hamstring Injuries
Lisa M. Bartoli
Chapter 13. Knee Injuries
Ron Noy
Chapter 14. Lower-Leg and Ankle Injuries
Christopher E Hubbard and William G. Hamilton
Chapter 15. Foot and Toe Injuries
Christopher E. Hubbard and William G. Hamilton
Chapter 16. Complementary and Integrative Health and Sports Injuries
Ann C. Cotter
Chapter 17. Injection Therapy and Biologics
Amir Mahajer and Julia Louisa Iafrate
Robert S. Gotlin, DO, was an academic and clinical authority in the subspecialty of orthopedic and sports medicine and rehabilitation. His medical school training was at the Southeastern University of the Health Sciences in Miami, Florida, after which he had his internship at the Brookdale Hospital Medical Center and his residency training at the Mount Sinai Hospital, both in New York City. His interests included sports injuries, back pain, running injuries, tailbone pain, youth sports, and exercise prescription, and he wrote extensively and lectured nationally and internationally on these topics.
Gotlin frequently appeared in the media, on radio, television, and in print. He hosted the Dr. Rob Says . . . Sports Health and Fitness show, which aired on 1050 ESPN, where he offered expertise and advice on a myriad of related topics. He served on the medical team with W. Norman Scott, MD, team physician for the New York Knicks (NBA) and New York Liberty (WNBA), and was physiatrist consultant to Michael Kelly, MD, team physician for the New Jersey Nets (NBA), and to Stuart Hershon, MD, team physician for the New York Yankees (MLB). He was also the team physician for the Harlem Wizards professional basketball team.
Dr. Gotlin passed away in June of 2022.
Flexibility training to decrease injury risk
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004).
By Jeff Young, Kinesiologist, CSCS, ACSM-EIM
Flexibility Training
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004). When restrictions exist because of lack of flexibility or mobility, movement is less efficient and the risk of injury increases. Many soft tissue injuries occur during the eccentric (lowering) phase of a movement while the muscles and tendons are under a load and on stretch (lengthening) (Verall and Dolman 2016). If a joint lacks flexibility, maximal or near-maximal lengthening of the muscles surrounding the joint will occur earlier in a movement. If this happens under a load, injury may occur. At a minimum, flexibility should be balanced around each major joint to reduce this risk (see figure 2.1).
To know objectively if a joint has restricted ROM, falls within the norms, or is hypermobile, an assessment should be performed at each major joint. It would behoove the athlete to have a joint ROM assessment performed by a qualified professional. Once this is accomplished, the athlete can be placed on a proper flexibility training program to balance flexibility around each major
joint.
Designing a flexibility program adheres to a principle known as FITT. The letters stand for Frequency, Intensity, Time (duration), and Type.

Figure 2.1 The hamstring is a commonly injured muscle group, so stretching exercises such as the supine hamstring stretch are important to help increase range of motion. Also, it is important to perform a joint range of motion assessment, and if the athlete lacks sufficient range, place the athlete on a proper flexibility training program to reduce the risk of muscle strain.
© Human Kinetics
Frequency
A stretching program should be initiated even if the athlete has normal joint ROM at each joint. In that case, the minimum recommendation of twice per week will be enough to maintain joint ROM. Increased tightness, or movement restriction, calls for an increase in volume. This can be accomplished by increasing the frequency, or sets, or both—the tighter an athlete is, the more stretching is needed. Therefore, joints that fall short of normal ROM (i.e., restricted or “tight” areas) should be stretched three to seven days per week (Garber et al. 2011). Stretching must be done properly and safely. Improper stretching has been shown to increase injury.
Intensity
Intensity lies on a subjective continuum of discomfort or pain that ranges from a “gentle” stretch to “mild discomfort,” “moderate discomfort,” “very uncomfortable,” or “painful.” Interestingly, all levels of discomfort, to include stretching to a point of pain (Muanjai, Jones, and Mickevicius 2017), have been shown to increase flexibility. Logically it is not recommended to stretch to the point of pain, and current evidence recommends stretching to the point of mild to moderate discomfort (Garber et al. 2011).
Time
Stretching durations span a continuum that ranges from 10 to 15 seconds up to several minutes in length. When the goal is to increase joint ROM, the total stretch time across multiple sets is most important. Therefore, athletes have the option of holding a stretch for a longer period of time (e.g., 90 seconds) or dividing the total time into multiple sets (e.g., three sets of 30 seconds) (Frietas et al. 2014).
Type
The several types of stretching include active, passive, dynamic, static, isometric, and proprioceptive neuromuscular facilitation (PNF). Dynamic stretching is the preferred mode of stretching as part of a warm-up prior to a workout or event. Among the other types of stretching, PNF has been shown to be superior in the short term, but all types of stretching can improve joint ROM when performed properly (Garber et al. 2011, Guissard and Duchateau 2006, Page 2012).
It is important to note that muscles are viscoelastic (Ryan et al. 2009, 2012). The viscoelastic property of muscle is what allows it to be deformed (stretched); and although its elasticity will also allow it to return back to its original form, through flexibility training joint ROM can increase above baseline values. If the goal is to maintain joint ROM, athletes should stretch until they reach an “end-range feel” for the given stretch (i.e., the feeling that it would be painful if they proceeded further into the stretch), hold, and release. But if the goal is to increase joint ROM, they should stretch until they reach their end range, hold, mentally relax into the stretch, and then increase the stretch to a new end range. This is known as muscle creep, or “creeping further into the stretch,” and the viscoelastic property of muscle, along with relaxation of the nervous system during the stretch, allows for this. The point: If athletes want to increase joint ROM but stretch only to their first end range (never taking advantage of muscle creep and neural relaxation that allows for an increase in ROM), the body is not signaled to progress, and the stretching will be fruitless. It is imperative to remember to find a second, and if possible, a third end range within each set of a stretch when the goal is to improve flexibility.
Self-myofascial release (SMR) is another method of increasing joint ROM, and while SMR will not directly decrease the chance of injury, because it assists in improving ROM and may increase performance as well, it should be included as part of a flexibility training program and warm-up (Beardsley and Skarabot 2015, Schroeder and Best 2015). While it is beyond the scope of this chapter to provide significant detail, SMR follows the FITT protocol and should be used concurrently with stretching, typically just prior to performing various stretches. Please see Cheatham and colleagues (2015) for more information.
Human factors of the biomechanics of function and injury
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete.
By Adam Gotlin, BS, MS
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete. Specifically, an athlete's age, sex, nutrition, and training all have significant effects on the biomechanics of movement. Even further, genetics, disease, and history of prior injury all influence how people move, the forces they create, and how materials in the body respond to loading. As previously discussed, injury occurs when loads exceed the tolerance of a given tissue. We now discuss the factors contributing to an individual's fitness and risk of injury.
Age
As humans grow, the musculoskeletal system undergoes many dramatic structural changes. During childhood and into the early 20s, human tissue generally develops and grows larger and stronger. In later adulthood, tissue begins to degenerate as wear and tear, toxins, and debris accumulate and outpace the healing powers of the body. The load-bearing capacity of tissue changes dramatically with age. Woo and colleagues tested the tensile strength of cadaver anterior cruciate ligaments for young adults (subject ages 22-35) and older adults (60-97). The young adult tendons could withstand roughly 2,160 N of tensile force before tearing, whereas the average peak force for older adults was 658 N (Woo et al. 1991). This is one of the primary reasons why surgeons commonly repair torn anterior cruciate ligaments using allografts, or donor ligament tissue, in older adults, and autografts, or graft tissue from another location in the patient's body, in young adults. In addition to changes in strength, different structures exist for youth athletes that must be considered when studying the biomechanics of injury. Growth plates are cartilaginous areas of long bones that act as sites for bone growth. Injury to growth plates can yield additional complications. Fractures to the area around growth plates can lead to growth that is misaligned with the normal skeleton or premature closure of the growth plate. Abnormal skeletal geometry can lead to suboptimal force distribution, which can lead to concentrated stresses and future injury.
Sex
There are many factors that contribute to differences in typical biomechanics of males and females. Sex has a large influence on structural anatomy, muscle mass, and skeletal geometry, all of which greatly influence how external forces are transmitted throughout the body. Further, hormones, sociological factors, and activity patterns may dictate why one sex is at greater risk of injury than the other. This should be taken into consideration when prescribing training and nutritional programs, as well as evaluating whether recommendations from research studies apply to one or both sexes. As an example, women are roughly five times more likely to tear an anterior cruciate ligament than men in similar sports. This seems to be due to anatomical differences combined with quadriceps dominance in muscle cocontraction over the knee during landing tasks in females (Ford et al. 2011). Sex affects not only the dimensions of the skeleton but also the coordination strategies adopted by athletes.
Nutrition
We are what we eat. Diet has a direct influence on the elements and minerals present in the body that are pivotal to proper function of the musculoskeletal system. Bone relies on calcium, an inorganic compound that the body does not produce on its own, to improve its strength and structural rigidity. Since calcium is secreted throughout the day, an adequate supply is needed in order to maintain mechanical strength. Women stop gaining new bone mass around the age of 30, so it is particularly important for them to maximize calcium intake prior to this age to reduce the chance of osteopenia or osteoporosis (diseases characterized by weak and fragile bones). Further, a core part of the adaptation and healing process is replenishing chemical and mineral deficiencies in the injured area. After an intense workout, athletes are encouraged to consume meals that contain high levels of protein and carbohydrate to facilitate the rebuilding of muscle. Proper levels of key proteins, fats, and other nutrients must exist in the body to facilitate the strengthening and healing of tissue.
Exercise
As discussed earlier, physical activity and normal loading lead to natural modeling and remodeling of body tissue. Bone responds to everyday loading by building new bone mass and remodeling existing bone mass to withstand future similar loading profiles. Normal loading through exercise also causes tendons and ligaments to grow larger or denser, increasing their stiffness and mechanical strength. Muscles respond directly to training and exercise by adapting their fiber structure and material composition. Resistance strength training will cause muscle to add fibers in series, increasing overall contractile strength; stretching will cause muscle fibers to be added in parallel, reducing stiffness and passive forces.
Other Factors
Genetics, disease, and drugs also have substantial effects on the mechanical and material properties of the musculoskeletal system. We already saw that the fast- to slow-twitch muscle fiber ratio is largely determined by genetics. Further, specific genes have been directly linked to muscle mass regulation in the body (Lee 2004). Various diseases can influence the biomechanics of movement by impeding the normal function of musculoskeletal elements. For example, rheumatoid arthritis is a disease in which the body mistakenly attacks its own joint cartilage, which can lead to pain and subsequent suboptimal gait modifications and loading patterns. Pharmaceutical drugs can have drastically positive and negative effects on an individual's biomechanics. Sometimes, the intention behind the drug is to influence biomechanics (i.e., ibuprofen to reduce pain from the inflammatory response), whereas other times the impact is a side effect (e.g., fluoroquinolones antibiotics increase the risk of tendon tear).
Platelet-rich plasma in treatment for sport injury
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology.
By Amir Mahajer, DO, FAOCPMR, FAAPMR, and Julia Louisa Iafrate, DO, CAQSM, FAAPMR
Platelet-Rich Plasma
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology. These cell lines were thought to have “stem cells” that may proliferate into different tissue types, such as cartilage or tendon in musculoskeletal injuries. This has been found not to be the case. Instead, it's believed that these injections create “intercellular communication” that leads to decreased inflammation, improved function, and even tissue healing (see figure 17.1). Platelet-rich plasma (PRP) is one of these types of therapies that holds promise for healing.

Figure 17.1 Ultrasound guided platelet-rich plasma (PRP) injection for rotator cuff tendinopathy and shoulder impingement syndrome.
© Amir Mahajer, DO
Platelet-rich plasma is a growing therapeutic modality in treating musculoskeletal disorders and particularly for sports injuries. Multiple studies have demonstrated safety and efficacy for athletes with pain and functional decline. Platelets are known to be an important component of clot formation (i.e., after a cut, the bleeding stops due to the presence of platelets). Over the past years, research has identified other possible actions of platelets. Parts of platelets known as growth factors seem to promote tissue healing.
Multiple different preparations of PRP are currently available, including leukocyte-rich versus leukocyte-poor PRP, and mixtures with higher concentrations of platelets or growth factors. The inclusion of leukocytes in these preparations is still debated due to their possible proinflammatory catabolic effect; however, they have a potential role in improved tissue remodeling and increased concentration of growth factors in cases of chronic tendinopathy. Both single- and multiple-spin PRP preparations are available, but it is unknown whether one technique is more therapeutic than the other. It is postulated that higher concentrations of platelets improve clinical outcomes. Though it makes sense to deliver higher concentrations of the factors to the localized injury site to cause recovery, having too many growth factors and cytokines may cause an imbalance in homeostasis and instead slow healing. Lastly, although PRP cryopreservation is safe and seems to preserve the ability to promote healing, storing platelets in freezing conditions can alter the morphology and decrease functional properties. Thus, fresh PRP continues to be favored at this time.
Currently, many professional and collegiate team physicians are using PRP despite a lack of consensus regarding optimal formulations and timing of treatment. While PRP injections do not seem to improve acute pain or decrease risk of relapses, they do appear to result in earlier return to sport in athletes with muscle strains and certain chronic tendinopathies. Additional research is needed to pinpoint the ideal ratio of platelet preparation methods and identify conditions and injuries that would most benefit from these treatments. A standardization for future biologic research has been proposed to help support the use of PRP or cell-based therapies and further advance the science of regenerative medicine.
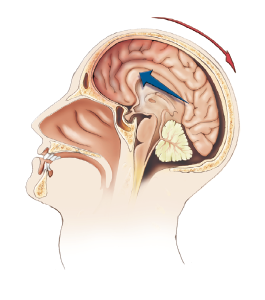
Understanding concussion and head injury
An impact to the head, neck, or elsewhere to the body causing an acceleration–deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
By Josh Krassen, DO
Concussion
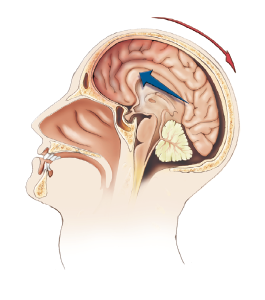
Common Causes
An impact to the head, neck, or elsewhere to the body causing an acceleration-deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
Identification and Prevention
A concussion is a traumatically induced alteration in mental status, such as confusion or amnesia, that may or may not involve a loss of consciousness (Kelly et al. 1991). It is based on functional, not structural, pathology, because imaging is often normal and not diagnostic of injury. There are 1.6 to 3.8 million sports and recreational concussions per year, and 135,000 are seen in the emergency room (Langlois JA et al. 2006). This injury most commonly occurs in American football during tackling or blocking but also occurs in other sports, such as in soccer when a player heads the ball or in ice hockey (more prevalent in women). There is good evidence that helmet use in skiing and snowboarding reduces head injuries. Limiting body checking in youth ice hockey and contact in youth football has also been shown to reduce head injuries. Teaching proper tackling techniques in football and avoidance of heading duels in soccer helps to reduce the risk of concussions. Evidence on use of mouth guards is inconsistent. Athletes with a history of previous concussions are more likely to have recurrent concussions (Guskiewicz et al. 2003).
It is important to have standard policies and protocols in place for education of players, referees, coaching staff, and parents of youth to help identify and understand the signs and symptoms of concussions. Everyone should have an understanding of its clinical features, assessment techniques, and principles for safe return to play. Concussions may involve clinical symptoms, physical signs, cognitive impairment, neurobehavioral features, and sleep-wake disturbances. Athletes can present with headaches, feelings of fogginess and drowsiness, forgetfulness, or irritability, or be emotionally unstable. Gait unsteadiness and slow reaction times are often noted. If any of these symptoms are observed, the athlete should be safely removed from practice or play.
Summary of Concussion Recommendations
- Removal from game with any sign or symptoms of concussion
- No return to play on day of injury
- Medical evaluation following injury, including neuropsychological testing and radiographs to rule out more serious intracranial pathology
- Adherence to stepwise return-to-play process:
- No activity until asymptomatic at rest and during exertion
- Light aerobic exercises
- Sport-specific exercises
- Noncontact drills
- Contact drills
- Game play
Two of the most important factors in determining next steps are the athlete's age and concussion history. Children have more prolonged and diffuse cerebral swelling and are at an increased risk for a second head injury (Pickles 1950). It is important to note that the speed of recovery is the same for all age groups, thus negating the theory that “kids heal faster.” Knowing whether the athlete has a history of concussions at the time of a new injury is important. Cumulative neuropsychological and subtle neurocognitive deficits can be seen after multiple concussions. After three or more concussions, athletes become more vulnerable to subsequent injuries (Collins et al. 2002) and therefore it is recommended that they retire from contact sports.
Overall there is a strong need for clear and practical guidelines to determine recovery and safe return to play for athletes with a sport-related concussion. One must remember that the science of concussion is incomplete, and thus management and return-to-play decisions should still be based on clinical judgment on an individualized basis.
Flexibility training to decrease injury risk
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004).
By Jeff Young, Kinesiologist, CSCS, ACSM-EIM
Flexibility Training
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004). When restrictions exist because of lack of flexibility or mobility, movement is less efficient and the risk of injury increases. Many soft tissue injuries occur during the eccentric (lowering) phase of a movement while the muscles and tendons are under a load and on stretch (lengthening) (Verall and Dolman 2016). If a joint lacks flexibility, maximal or near-maximal lengthening of the muscles surrounding the joint will occur earlier in a movement. If this happens under a load, injury may occur. At a minimum, flexibility should be balanced around each major joint to reduce this risk (see figure 2.1).
To know objectively if a joint has restricted ROM, falls within the norms, or is hypermobile, an assessment should be performed at each major joint. It would behoove the athlete to have a joint ROM assessment performed by a qualified professional. Once this is accomplished, the athlete can be placed on a proper flexibility training program to balance flexibility around each major
joint.
Designing a flexibility program adheres to a principle known as FITT. The letters stand for Frequency, Intensity, Time (duration), and Type.

Figure 2.1 The hamstring is a commonly injured muscle group, so stretching exercises such as the supine hamstring stretch are important to help increase range of motion. Also, it is important to perform a joint range of motion assessment, and if the athlete lacks sufficient range, place the athlete on a proper flexibility training program to reduce the risk of muscle strain.
© Human Kinetics
Frequency
A stretching program should be initiated even if the athlete has normal joint ROM at each joint. In that case, the minimum recommendation of twice per week will be enough to maintain joint ROM. Increased tightness, or movement restriction, calls for an increase in volume. This can be accomplished by increasing the frequency, or sets, or both—the tighter an athlete is, the more stretching is needed. Therefore, joints that fall short of normal ROM (i.e., restricted or “tight” areas) should be stretched three to seven days per week (Garber et al. 2011). Stretching must be done properly and safely. Improper stretching has been shown to increase injury.
Intensity
Intensity lies on a subjective continuum of discomfort or pain that ranges from a “gentle” stretch to “mild discomfort,” “moderate discomfort,” “very uncomfortable,” or “painful.” Interestingly, all levels of discomfort, to include stretching to a point of pain (Muanjai, Jones, and Mickevicius 2017), have been shown to increase flexibility. Logically it is not recommended to stretch to the point of pain, and current evidence recommends stretching to the point of mild to moderate discomfort (Garber et al. 2011).
Time
Stretching durations span a continuum that ranges from 10 to 15 seconds up to several minutes in length. When the goal is to increase joint ROM, the total stretch time across multiple sets is most important. Therefore, athletes have the option of holding a stretch for a longer period of time (e.g., 90 seconds) or dividing the total time into multiple sets (e.g., three sets of 30 seconds) (Frietas et al. 2014).
Type
The several types of stretching include active, passive, dynamic, static, isometric, and proprioceptive neuromuscular facilitation (PNF). Dynamic stretching is the preferred mode of stretching as part of a warm-up prior to a workout or event. Among the other types of stretching, PNF has been shown to be superior in the short term, but all types of stretching can improve joint ROM when performed properly (Garber et al. 2011, Guissard and Duchateau 2006, Page 2012).
It is important to note that muscles are viscoelastic (Ryan et al. 2009, 2012). The viscoelastic property of muscle is what allows it to be deformed (stretched); and although its elasticity will also allow it to return back to its original form, through flexibility training joint ROM can increase above baseline values. If the goal is to maintain joint ROM, athletes should stretch until they reach an “end-range feel” for the given stretch (i.e., the feeling that it would be painful if they proceeded further into the stretch), hold, and release. But if the goal is to increase joint ROM, they should stretch until they reach their end range, hold, mentally relax into the stretch, and then increase the stretch to a new end range. This is known as muscle creep, or “creeping further into the stretch,” and the viscoelastic property of muscle, along with relaxation of the nervous system during the stretch, allows for this. The point: If athletes want to increase joint ROM but stretch only to their first end range (never taking advantage of muscle creep and neural relaxation that allows for an increase in ROM), the body is not signaled to progress, and the stretching will be fruitless. It is imperative to remember to find a second, and if possible, a third end range within each set of a stretch when the goal is to improve flexibility.
Self-myofascial release (SMR) is another method of increasing joint ROM, and while SMR will not directly decrease the chance of injury, because it assists in improving ROM and may increase performance as well, it should be included as part of a flexibility training program and warm-up (Beardsley and Skarabot 2015, Schroeder and Best 2015). While it is beyond the scope of this chapter to provide significant detail, SMR follows the FITT protocol and should be used concurrently with stretching, typically just prior to performing various stretches. Please see Cheatham and colleagues (2015) for more information.
Human factors of the biomechanics of function and injury
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete.
By Adam Gotlin, BS, MS
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete. Specifically, an athlete's age, sex, nutrition, and training all have significant effects on the biomechanics of movement. Even further, genetics, disease, and history of prior injury all influence how people move, the forces they create, and how materials in the body respond to loading. As previously discussed, injury occurs when loads exceed the tolerance of a given tissue. We now discuss the factors contributing to an individual's fitness and risk of injury.
Age
As humans grow, the musculoskeletal system undergoes many dramatic structural changes. During childhood and into the early 20s, human tissue generally develops and grows larger and stronger. In later adulthood, tissue begins to degenerate as wear and tear, toxins, and debris accumulate and outpace the healing powers of the body. The load-bearing capacity of tissue changes dramatically with age. Woo and colleagues tested the tensile strength of cadaver anterior cruciate ligaments for young adults (subject ages 22-35) and older adults (60-97). The young adult tendons could withstand roughly 2,160 N of tensile force before tearing, whereas the average peak force for older adults was 658 N (Woo et al. 1991). This is one of the primary reasons why surgeons commonly repair torn anterior cruciate ligaments using allografts, or donor ligament tissue, in older adults, and autografts, or graft tissue from another location in the patient's body, in young adults. In addition to changes in strength, different structures exist for youth athletes that must be considered when studying the biomechanics of injury. Growth plates are cartilaginous areas of long bones that act as sites for bone growth. Injury to growth plates can yield additional complications. Fractures to the area around growth plates can lead to growth that is misaligned with the normal skeleton or premature closure of the growth plate. Abnormal skeletal geometry can lead to suboptimal force distribution, which can lead to concentrated stresses and future injury.
Sex
There are many factors that contribute to differences in typical biomechanics of males and females. Sex has a large influence on structural anatomy, muscle mass, and skeletal geometry, all of which greatly influence how external forces are transmitted throughout the body. Further, hormones, sociological factors, and activity patterns may dictate why one sex is at greater risk of injury than the other. This should be taken into consideration when prescribing training and nutritional programs, as well as evaluating whether recommendations from research studies apply to one or both sexes. As an example, women are roughly five times more likely to tear an anterior cruciate ligament than men in similar sports. This seems to be due to anatomical differences combined with quadriceps dominance in muscle cocontraction over the knee during landing tasks in females (Ford et al. 2011). Sex affects not only the dimensions of the skeleton but also the coordination strategies adopted by athletes.
Nutrition
We are what we eat. Diet has a direct influence on the elements and minerals present in the body that are pivotal to proper function of the musculoskeletal system. Bone relies on calcium, an inorganic compound that the body does not produce on its own, to improve its strength and structural rigidity. Since calcium is secreted throughout the day, an adequate supply is needed in order to maintain mechanical strength. Women stop gaining new bone mass around the age of 30, so it is particularly important for them to maximize calcium intake prior to this age to reduce the chance of osteopenia or osteoporosis (diseases characterized by weak and fragile bones). Further, a core part of the adaptation and healing process is replenishing chemical and mineral deficiencies in the injured area. After an intense workout, athletes are encouraged to consume meals that contain high levels of protein and carbohydrate to facilitate the rebuilding of muscle. Proper levels of key proteins, fats, and other nutrients must exist in the body to facilitate the strengthening and healing of tissue.
Exercise
As discussed earlier, physical activity and normal loading lead to natural modeling and remodeling of body tissue. Bone responds to everyday loading by building new bone mass and remodeling existing bone mass to withstand future similar loading profiles. Normal loading through exercise also causes tendons and ligaments to grow larger or denser, increasing their stiffness and mechanical strength. Muscles respond directly to training and exercise by adapting their fiber structure and material composition. Resistance strength training will cause muscle to add fibers in series, increasing overall contractile strength; stretching will cause muscle fibers to be added in parallel, reducing stiffness and passive forces.
Other Factors
Genetics, disease, and drugs also have substantial effects on the mechanical and material properties of the musculoskeletal system. We already saw that the fast- to slow-twitch muscle fiber ratio is largely determined by genetics. Further, specific genes have been directly linked to muscle mass regulation in the body (Lee 2004). Various diseases can influence the biomechanics of movement by impeding the normal function of musculoskeletal elements. For example, rheumatoid arthritis is a disease in which the body mistakenly attacks its own joint cartilage, which can lead to pain and subsequent suboptimal gait modifications and loading patterns. Pharmaceutical drugs can have drastically positive and negative effects on an individual's biomechanics. Sometimes, the intention behind the drug is to influence biomechanics (i.e., ibuprofen to reduce pain from the inflammatory response), whereas other times the impact is a side effect (e.g., fluoroquinolones antibiotics increase the risk of tendon tear).
Platelet-rich plasma in treatment for sport injury
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology.
By Amir Mahajer, DO, FAOCPMR, FAAPMR, and Julia Louisa Iafrate, DO, CAQSM, FAAPMR
Platelet-Rich Plasma
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology. These cell lines were thought to have “stem cells” that may proliferate into different tissue types, such as cartilage or tendon in musculoskeletal injuries. This has been found not to be the case. Instead, it's believed that these injections create “intercellular communication” that leads to decreased inflammation, improved function, and even tissue healing (see figure 17.1). Platelet-rich plasma (PRP) is one of these types of therapies that holds promise for healing.

Figure 17.1 Ultrasound guided platelet-rich plasma (PRP) injection for rotator cuff tendinopathy and shoulder impingement syndrome.
© Amir Mahajer, DO
Platelet-rich plasma is a growing therapeutic modality in treating musculoskeletal disorders and particularly for sports injuries. Multiple studies have demonstrated safety and efficacy for athletes with pain and functional decline. Platelets are known to be an important component of clot formation (i.e., after a cut, the bleeding stops due to the presence of platelets). Over the past years, research has identified other possible actions of platelets. Parts of platelets known as growth factors seem to promote tissue healing.
Multiple different preparations of PRP are currently available, including leukocyte-rich versus leukocyte-poor PRP, and mixtures with higher concentrations of platelets or growth factors. The inclusion of leukocytes in these preparations is still debated due to their possible proinflammatory catabolic effect; however, they have a potential role in improved tissue remodeling and increased concentration of growth factors in cases of chronic tendinopathy. Both single- and multiple-spin PRP preparations are available, but it is unknown whether one technique is more therapeutic than the other. It is postulated that higher concentrations of platelets improve clinical outcomes. Though it makes sense to deliver higher concentrations of the factors to the localized injury site to cause recovery, having too many growth factors and cytokines may cause an imbalance in homeostasis and instead slow healing. Lastly, although PRP cryopreservation is safe and seems to preserve the ability to promote healing, storing platelets in freezing conditions can alter the morphology and decrease functional properties. Thus, fresh PRP continues to be favored at this time.
Currently, many professional and collegiate team physicians are using PRP despite a lack of consensus regarding optimal formulations and timing of treatment. While PRP injections do not seem to improve acute pain or decrease risk of relapses, they do appear to result in earlier return to sport in athletes with muscle strains and certain chronic tendinopathies. Additional research is needed to pinpoint the ideal ratio of platelet preparation methods and identify conditions and injuries that would most benefit from these treatments. A standardization for future biologic research has been proposed to help support the use of PRP or cell-based therapies and further advance the science of regenerative medicine.
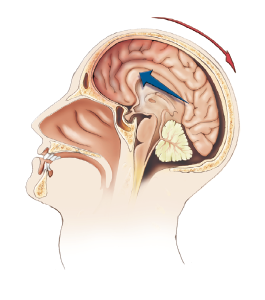
Understanding concussion and head injury
An impact to the head, neck, or elsewhere to the body causing an acceleration–deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
By Josh Krassen, DO
Concussion
Common Causes
An impact to the head, neck, or elsewhere to the body causing an acceleration-deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
Identification and Prevention
A concussion is a traumatically induced alteration in mental status, such as confusion or amnesia, that may or may not involve a loss of consciousness (Kelly et al. 1991). It is based on functional, not structural, pathology, because imaging is often normal and not diagnostic of injury. There are 1.6 to 3.8 million sports and recreational concussions per year, and 135,000 are seen in the emergency room (Langlois JA et al. 2006). This injury most commonly occurs in American football during tackling or blocking but also occurs in other sports, such as in soccer when a player heads the ball or in ice hockey (more prevalent in women). There is good evidence that helmet use in skiing and snowboarding reduces head injuries. Limiting body checking in youth ice hockey and contact in youth football has also been shown to reduce head injuries. Teaching proper tackling techniques in football and avoidance of heading duels in soccer helps to reduce the risk of concussions. Evidence on use of mouth guards is inconsistent. Athletes with a history of previous concussions are more likely to have recurrent concussions (Guskiewicz et al. 2003).
It is important to have standard policies and protocols in place for education of players, referees, coaching staff, and parents of youth to help identify and understand the signs and symptoms of concussions. Everyone should have an understanding of its clinical features, assessment techniques, and principles for safe return to play. Concussions may involve clinical symptoms, physical signs, cognitive impairment, neurobehavioral features, and sleep-wake disturbances. Athletes can present with headaches, feelings of fogginess and drowsiness, forgetfulness, or irritability, or be emotionally unstable. Gait unsteadiness and slow reaction times are often noted. If any of these symptoms are observed, the athlete should be safely removed from practice or play.
Summary of Concussion Recommendations
- Removal from game with any sign or symptoms of concussion
- No return to play on day of injury
- Medical evaluation following injury, including neuropsychological testing and radiographs to rule out more serious intracranial pathology
- Adherence to stepwise return-to-play process:
- No activity until asymptomatic at rest and during exertion
- Light aerobic exercises
- Sport-specific exercises
- Noncontact drills
- Contact drills
- Game play
Two of the most important factors in determining next steps are the athlete's age and concussion history. Children have more prolonged and diffuse cerebral swelling and are at an increased risk for a second head injury (Pickles 1950). It is important to note that the speed of recovery is the same for all age groups, thus negating the theory that “kids heal faster.” Knowing whether the athlete has a history of concussions at the time of a new injury is important. Cumulative neuropsychological and subtle neurocognitive deficits can be seen after multiple concussions. After three or more concussions, athletes become more vulnerable to subsequent injuries (Collins et al. 2002) and therefore it is recommended that they retire from contact sports.
Overall there is a strong need for clear and practical guidelines to determine recovery and safe return to play for athletes with a sport-related concussion. One must remember that the science of concussion is incomplete, and thus management and return-to-play decisions should still be based on clinical judgment on an individualized basis.
Flexibility training to decrease injury risk
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004).
By Jeff Young, Kinesiologist, CSCS, ACSM-EIM
Flexibility Training
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004). When restrictions exist because of lack of flexibility or mobility, movement is less efficient and the risk of injury increases. Many soft tissue injuries occur during the eccentric (lowering) phase of a movement while the muscles and tendons are under a load and on stretch (lengthening) (Verall and Dolman 2016). If a joint lacks flexibility, maximal or near-maximal lengthening of the muscles surrounding the joint will occur earlier in a movement. If this happens under a load, injury may occur. At a minimum, flexibility should be balanced around each major joint to reduce this risk (see figure 2.1).
To know objectively if a joint has restricted ROM, falls within the norms, or is hypermobile, an assessment should be performed at each major joint. It would behoove the athlete to have a joint ROM assessment performed by a qualified professional. Once this is accomplished, the athlete can be placed on a proper flexibility training program to balance flexibility around each major
joint.
Designing a flexibility program adheres to a principle known as FITT. The letters stand for Frequency, Intensity, Time (duration), and Type.

Figure 2.1 The hamstring is a commonly injured muscle group, so stretching exercises such as the supine hamstring stretch are important to help increase range of motion. Also, it is important to perform a joint range of motion assessment, and if the athlete lacks sufficient range, place the athlete on a proper flexibility training program to reduce the risk of muscle strain.
© Human Kinetics
Frequency
A stretching program should be initiated even if the athlete has normal joint ROM at each joint. In that case, the minimum recommendation of twice per week will be enough to maintain joint ROM. Increased tightness, or movement restriction, calls for an increase in volume. This can be accomplished by increasing the frequency, or sets, or both—the tighter an athlete is, the more stretching is needed. Therefore, joints that fall short of normal ROM (i.e., restricted or “tight” areas) should be stretched three to seven days per week (Garber et al. 2011). Stretching must be done properly and safely. Improper stretching has been shown to increase injury.
Intensity
Intensity lies on a subjective continuum of discomfort or pain that ranges from a “gentle” stretch to “mild discomfort,” “moderate discomfort,” “very uncomfortable,” or “painful.” Interestingly, all levels of discomfort, to include stretching to a point of pain (Muanjai, Jones, and Mickevicius 2017), have been shown to increase flexibility. Logically it is not recommended to stretch to the point of pain, and current evidence recommends stretching to the point of mild to moderate discomfort (Garber et al. 2011).
Time
Stretching durations span a continuum that ranges from 10 to 15 seconds up to several minutes in length. When the goal is to increase joint ROM, the total stretch time across multiple sets is most important. Therefore, athletes have the option of holding a stretch for a longer period of time (e.g., 90 seconds) or dividing the total time into multiple sets (e.g., three sets of 30 seconds) (Frietas et al. 2014).
Type
The several types of stretching include active, passive, dynamic, static, isometric, and proprioceptive neuromuscular facilitation (PNF). Dynamic stretching is the preferred mode of stretching as part of a warm-up prior to a workout or event. Among the other types of stretching, PNF has been shown to be superior in the short term, but all types of stretching can improve joint ROM when performed properly (Garber et al. 2011, Guissard and Duchateau 2006, Page 2012).
It is important to note that muscles are viscoelastic (Ryan et al. 2009, 2012). The viscoelastic property of muscle is what allows it to be deformed (stretched); and although its elasticity will also allow it to return back to its original form, through flexibility training joint ROM can increase above baseline values. If the goal is to maintain joint ROM, athletes should stretch until they reach an “end-range feel” for the given stretch (i.e., the feeling that it would be painful if they proceeded further into the stretch), hold, and release. But if the goal is to increase joint ROM, they should stretch until they reach their end range, hold, mentally relax into the stretch, and then increase the stretch to a new end range. This is known as muscle creep, or “creeping further into the stretch,” and the viscoelastic property of muscle, along with relaxation of the nervous system during the stretch, allows for this. The point: If athletes want to increase joint ROM but stretch only to their first end range (never taking advantage of muscle creep and neural relaxation that allows for an increase in ROM), the body is not signaled to progress, and the stretching will be fruitless. It is imperative to remember to find a second, and if possible, a third end range within each set of a stretch when the goal is to improve flexibility.
Self-myofascial release (SMR) is another method of increasing joint ROM, and while SMR will not directly decrease the chance of injury, because it assists in improving ROM and may increase performance as well, it should be included as part of a flexibility training program and warm-up (Beardsley and Skarabot 2015, Schroeder and Best 2015). While it is beyond the scope of this chapter to provide significant detail, SMR follows the FITT protocol and should be used concurrently with stretching, typically just prior to performing various stretches. Please see Cheatham and colleagues (2015) for more information.
Human factors of the biomechanics of function and injury
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete.
By Adam Gotlin, BS, MS
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete. Specifically, an athlete's age, sex, nutrition, and training all have significant effects on the biomechanics of movement. Even further, genetics, disease, and history of prior injury all influence how people move, the forces they create, and how materials in the body respond to loading. As previously discussed, injury occurs when loads exceed the tolerance of a given tissue. We now discuss the factors contributing to an individual's fitness and risk of injury.
Age
As humans grow, the musculoskeletal system undergoes many dramatic structural changes. During childhood and into the early 20s, human tissue generally develops and grows larger and stronger. In later adulthood, tissue begins to degenerate as wear and tear, toxins, and debris accumulate and outpace the healing powers of the body. The load-bearing capacity of tissue changes dramatically with age. Woo and colleagues tested the tensile strength of cadaver anterior cruciate ligaments for young adults (subject ages 22-35) and older adults (60-97). The young adult tendons could withstand roughly 2,160 N of tensile force before tearing, whereas the average peak force for older adults was 658 N (Woo et al. 1991). This is one of the primary reasons why surgeons commonly repair torn anterior cruciate ligaments using allografts, or donor ligament tissue, in older adults, and autografts, or graft tissue from another location in the patient's body, in young adults. In addition to changes in strength, different structures exist for youth athletes that must be considered when studying the biomechanics of injury. Growth plates are cartilaginous areas of long bones that act as sites for bone growth. Injury to growth plates can yield additional complications. Fractures to the area around growth plates can lead to growth that is misaligned with the normal skeleton or premature closure of the growth plate. Abnormal skeletal geometry can lead to suboptimal force distribution, which can lead to concentrated stresses and future injury.
Sex
There are many factors that contribute to differences in typical biomechanics of males and females. Sex has a large influence on structural anatomy, muscle mass, and skeletal geometry, all of which greatly influence how external forces are transmitted throughout the body. Further, hormones, sociological factors, and activity patterns may dictate why one sex is at greater risk of injury than the other. This should be taken into consideration when prescribing training and nutritional programs, as well as evaluating whether recommendations from research studies apply to one or both sexes. As an example, women are roughly five times more likely to tear an anterior cruciate ligament than men in similar sports. This seems to be due to anatomical differences combined with quadriceps dominance in muscle cocontraction over the knee during landing tasks in females (Ford et al. 2011). Sex affects not only the dimensions of the skeleton but also the coordination strategies adopted by athletes.
Nutrition
We are what we eat. Diet has a direct influence on the elements and minerals present in the body that are pivotal to proper function of the musculoskeletal system. Bone relies on calcium, an inorganic compound that the body does not produce on its own, to improve its strength and structural rigidity. Since calcium is secreted throughout the day, an adequate supply is needed in order to maintain mechanical strength. Women stop gaining new bone mass around the age of 30, so it is particularly important for them to maximize calcium intake prior to this age to reduce the chance of osteopenia or osteoporosis (diseases characterized by weak and fragile bones). Further, a core part of the adaptation and healing process is replenishing chemical and mineral deficiencies in the injured area. After an intense workout, athletes are encouraged to consume meals that contain high levels of protein and carbohydrate to facilitate the rebuilding of muscle. Proper levels of key proteins, fats, and other nutrients must exist in the body to facilitate the strengthening and healing of tissue.
Exercise
As discussed earlier, physical activity and normal loading lead to natural modeling and remodeling of body tissue. Bone responds to everyday loading by building new bone mass and remodeling existing bone mass to withstand future similar loading profiles. Normal loading through exercise also causes tendons and ligaments to grow larger or denser, increasing their stiffness and mechanical strength. Muscles respond directly to training and exercise by adapting their fiber structure and material composition. Resistance strength training will cause muscle to add fibers in series, increasing overall contractile strength; stretching will cause muscle fibers to be added in parallel, reducing stiffness and passive forces.
Other Factors
Genetics, disease, and drugs also have substantial effects on the mechanical and material properties of the musculoskeletal system. We already saw that the fast- to slow-twitch muscle fiber ratio is largely determined by genetics. Further, specific genes have been directly linked to muscle mass regulation in the body (Lee 2004). Various diseases can influence the biomechanics of movement by impeding the normal function of musculoskeletal elements. For example, rheumatoid arthritis is a disease in which the body mistakenly attacks its own joint cartilage, which can lead to pain and subsequent suboptimal gait modifications and loading patterns. Pharmaceutical drugs can have drastically positive and negative effects on an individual's biomechanics. Sometimes, the intention behind the drug is to influence biomechanics (i.e., ibuprofen to reduce pain from the inflammatory response), whereas other times the impact is a side effect (e.g., fluoroquinolones antibiotics increase the risk of tendon tear).
Platelet-rich plasma in treatment for sport injury
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology.
By Amir Mahajer, DO, FAOCPMR, FAAPMR, and Julia Louisa Iafrate, DO, CAQSM, FAAPMR
Platelet-Rich Plasma
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology. These cell lines were thought to have “stem cells” that may proliferate into different tissue types, such as cartilage or tendon in musculoskeletal injuries. This has been found not to be the case. Instead, it's believed that these injections create “intercellular communication” that leads to decreased inflammation, improved function, and even tissue healing (see figure 17.1). Platelet-rich plasma (PRP) is one of these types of therapies that holds promise for healing.

Figure 17.1 Ultrasound guided platelet-rich plasma (PRP) injection for rotator cuff tendinopathy and shoulder impingement syndrome.
© Amir Mahajer, DO
Platelet-rich plasma is a growing therapeutic modality in treating musculoskeletal disorders and particularly for sports injuries. Multiple studies have demonstrated safety and efficacy for athletes with pain and functional decline. Platelets are known to be an important component of clot formation (i.e., after a cut, the bleeding stops due to the presence of platelets). Over the past years, research has identified other possible actions of platelets. Parts of platelets known as growth factors seem to promote tissue healing.
Multiple different preparations of PRP are currently available, including leukocyte-rich versus leukocyte-poor PRP, and mixtures with higher concentrations of platelets or growth factors. The inclusion of leukocytes in these preparations is still debated due to their possible proinflammatory catabolic effect; however, they have a potential role in improved tissue remodeling and increased concentration of growth factors in cases of chronic tendinopathy. Both single- and multiple-spin PRP preparations are available, but it is unknown whether one technique is more therapeutic than the other. It is postulated that higher concentrations of platelets improve clinical outcomes. Though it makes sense to deliver higher concentrations of the factors to the localized injury site to cause recovery, having too many growth factors and cytokines may cause an imbalance in homeostasis and instead slow healing. Lastly, although PRP cryopreservation is safe and seems to preserve the ability to promote healing, storing platelets in freezing conditions can alter the morphology and decrease functional properties. Thus, fresh PRP continues to be favored at this time.
Currently, many professional and collegiate team physicians are using PRP despite a lack of consensus regarding optimal formulations and timing of treatment. While PRP injections do not seem to improve acute pain or decrease risk of relapses, they do appear to result in earlier return to sport in athletes with muscle strains and certain chronic tendinopathies. Additional research is needed to pinpoint the ideal ratio of platelet preparation methods and identify conditions and injuries that would most benefit from these treatments. A standardization for future biologic research has been proposed to help support the use of PRP or cell-based therapies and further advance the science of regenerative medicine.
Understanding concussion and head injury
An impact to the head, neck, or elsewhere to the body causing an acceleration–deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
By Josh Krassen, DO
Concussion
Common Causes
An impact to the head, neck, or elsewhere to the body causing an acceleration-deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
Identification and Prevention
A concussion is a traumatically induced alteration in mental status, such as confusion or amnesia, that may or may not involve a loss of consciousness (Kelly et al. 1991). It is based on functional, not structural, pathology, because imaging is often normal and not diagnostic of injury. There are 1.6 to 3.8 million sports and recreational concussions per year, and 135,000 are seen in the emergency room (Langlois JA et al. 2006). This injury most commonly occurs in American football during tackling or blocking but also occurs in other sports, such as in soccer when a player heads the ball or in ice hockey (more prevalent in women). There is good evidence that helmet use in skiing and snowboarding reduces head injuries. Limiting body checking in youth ice hockey and contact in youth football has also been shown to reduce head injuries. Teaching proper tackling techniques in football and avoidance of heading duels in soccer helps to reduce the risk of concussions. Evidence on use of mouth guards is inconsistent. Athletes with a history of previous concussions are more likely to have recurrent concussions (Guskiewicz et al. 2003).
It is important to have standard policies and protocols in place for education of players, referees, coaching staff, and parents of youth to help identify and understand the signs and symptoms of concussions. Everyone should have an understanding of its clinical features, assessment techniques, and principles for safe return to play. Concussions may involve clinical symptoms, physical signs, cognitive impairment, neurobehavioral features, and sleep-wake disturbances. Athletes can present with headaches, feelings of fogginess and drowsiness, forgetfulness, or irritability, or be emotionally unstable. Gait unsteadiness and slow reaction times are often noted. If any of these symptoms are observed, the athlete should be safely removed from practice or play.
Summary of Concussion Recommendations
- Removal from game with any sign or symptoms of concussion
- No return to play on day of injury
- Medical evaluation following injury, including neuropsychological testing and radiographs to rule out more serious intracranial pathology
- Adherence to stepwise return-to-play process:
- No activity until asymptomatic at rest and during exertion
- Light aerobic exercises
- Sport-specific exercises
- Noncontact drills
- Contact drills
- Game play
Two of the most important factors in determining next steps are the athlete's age and concussion history. Children have more prolonged and diffuse cerebral swelling and are at an increased risk for a second head injury (Pickles 1950). It is important to note that the speed of recovery is the same for all age groups, thus negating the theory that “kids heal faster.” Knowing whether the athlete has a history of concussions at the time of a new injury is important. Cumulative neuropsychological and subtle neurocognitive deficits can be seen after multiple concussions. After three or more concussions, athletes become more vulnerable to subsequent injuries (Collins et al. 2002) and therefore it is recommended that they retire from contact sports.
Overall there is a strong need for clear and practical guidelines to determine recovery and safe return to play for athletes with a sport-related concussion. One must remember that the science of concussion is incomplete, and thus management and return-to-play decisions should still be based on clinical judgment on an individualized basis.
Flexibility training to decrease injury risk
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004).
By Jeff Young, Kinesiologist, CSCS, ACSM-EIM
Flexibility Training
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004). When restrictions exist because of lack of flexibility or mobility, movement is less efficient and the risk of injury increases. Many soft tissue injuries occur during the eccentric (lowering) phase of a movement while the muscles and tendons are under a load and on stretch (lengthening) (Verall and Dolman 2016). If a joint lacks flexibility, maximal or near-maximal lengthening of the muscles surrounding the joint will occur earlier in a movement. If this happens under a load, injury may occur. At a minimum, flexibility should be balanced around each major joint to reduce this risk (see figure 2.1).
To know objectively if a joint has restricted ROM, falls within the norms, or is hypermobile, an assessment should be performed at each major joint. It would behoove the athlete to have a joint ROM assessment performed by a qualified professional. Once this is accomplished, the athlete can be placed on a proper flexibility training program to balance flexibility around each major
joint.
Designing a flexibility program adheres to a principle known as FITT. The letters stand for Frequency, Intensity, Time (duration), and Type.

Figure 2.1 The hamstring is a commonly injured muscle group, so stretching exercises such as the supine hamstring stretch are important to help increase range of motion. Also, it is important to perform a joint range of motion assessment, and if the athlete lacks sufficient range, place the athlete on a proper flexibility training program to reduce the risk of muscle strain.
© Human Kinetics
Frequency
A stretching program should be initiated even if the athlete has normal joint ROM at each joint. In that case, the minimum recommendation of twice per week will be enough to maintain joint ROM. Increased tightness, or movement restriction, calls for an increase in volume. This can be accomplished by increasing the frequency, or sets, or both—the tighter an athlete is, the more stretching is needed. Therefore, joints that fall short of normal ROM (i.e., restricted or “tight” areas) should be stretched three to seven days per week (Garber et al. 2011). Stretching must be done properly and safely. Improper stretching has been shown to increase injury.
Intensity
Intensity lies on a subjective continuum of discomfort or pain that ranges from a “gentle” stretch to “mild discomfort,” “moderate discomfort,” “very uncomfortable,” or “painful.” Interestingly, all levels of discomfort, to include stretching to a point of pain (Muanjai, Jones, and Mickevicius 2017), have been shown to increase flexibility. Logically it is not recommended to stretch to the point of pain, and current evidence recommends stretching to the point of mild to moderate discomfort (Garber et al. 2011).
Time
Stretching durations span a continuum that ranges from 10 to 15 seconds up to several minutes in length. When the goal is to increase joint ROM, the total stretch time across multiple sets is most important. Therefore, athletes have the option of holding a stretch for a longer period of time (e.g., 90 seconds) or dividing the total time into multiple sets (e.g., three sets of 30 seconds) (Frietas et al. 2014).
Type
The several types of stretching include active, passive, dynamic, static, isometric, and proprioceptive neuromuscular facilitation (PNF). Dynamic stretching is the preferred mode of stretching as part of a warm-up prior to a workout or event. Among the other types of stretching, PNF has been shown to be superior in the short term, but all types of stretching can improve joint ROM when performed properly (Garber et al. 2011, Guissard and Duchateau 2006, Page 2012).
It is important to note that muscles are viscoelastic (Ryan et al. 2009, 2012). The viscoelastic property of muscle is what allows it to be deformed (stretched); and although its elasticity will also allow it to return back to its original form, through flexibility training joint ROM can increase above baseline values. If the goal is to maintain joint ROM, athletes should stretch until they reach an “end-range feel” for the given stretch (i.e., the feeling that it would be painful if they proceeded further into the stretch), hold, and release. But if the goal is to increase joint ROM, they should stretch until they reach their end range, hold, mentally relax into the stretch, and then increase the stretch to a new end range. This is known as muscle creep, or “creeping further into the stretch,” and the viscoelastic property of muscle, along with relaxation of the nervous system during the stretch, allows for this. The point: If athletes want to increase joint ROM but stretch only to their first end range (never taking advantage of muscle creep and neural relaxation that allows for an increase in ROM), the body is not signaled to progress, and the stretching will be fruitless. It is imperative to remember to find a second, and if possible, a third end range within each set of a stretch when the goal is to improve flexibility.
Self-myofascial release (SMR) is another method of increasing joint ROM, and while SMR will not directly decrease the chance of injury, because it assists in improving ROM and may increase performance as well, it should be included as part of a flexibility training program and warm-up (Beardsley and Skarabot 2015, Schroeder and Best 2015). While it is beyond the scope of this chapter to provide significant detail, SMR follows the FITT protocol and should be used concurrently with stretching, typically just prior to performing various stretches. Please see Cheatham and colleagues (2015) for more information.
Human factors of the biomechanics of function and injury
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete.
By Adam Gotlin, BS, MS
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete. Specifically, an athlete's age, sex, nutrition, and training all have significant effects on the biomechanics of movement. Even further, genetics, disease, and history of prior injury all influence how people move, the forces they create, and how materials in the body respond to loading. As previously discussed, injury occurs when loads exceed the tolerance of a given tissue. We now discuss the factors contributing to an individual's fitness and risk of injury.
Age
As humans grow, the musculoskeletal system undergoes many dramatic structural changes. During childhood and into the early 20s, human tissue generally develops and grows larger and stronger. In later adulthood, tissue begins to degenerate as wear and tear, toxins, and debris accumulate and outpace the healing powers of the body. The load-bearing capacity of tissue changes dramatically with age. Woo and colleagues tested the tensile strength of cadaver anterior cruciate ligaments for young adults (subject ages 22-35) and older adults (60-97). The young adult tendons could withstand roughly 2,160 N of tensile force before tearing, whereas the average peak force for older adults was 658 N (Woo et al. 1991). This is one of the primary reasons why surgeons commonly repair torn anterior cruciate ligaments using allografts, or donor ligament tissue, in older adults, and autografts, or graft tissue from another location in the patient's body, in young adults. In addition to changes in strength, different structures exist for youth athletes that must be considered when studying the biomechanics of injury. Growth plates are cartilaginous areas of long bones that act as sites for bone growth. Injury to growth plates can yield additional complications. Fractures to the area around growth plates can lead to growth that is misaligned with the normal skeleton or premature closure of the growth plate. Abnormal skeletal geometry can lead to suboptimal force distribution, which can lead to concentrated stresses and future injury.
Sex
There are many factors that contribute to differences in typical biomechanics of males and females. Sex has a large influence on structural anatomy, muscle mass, and skeletal geometry, all of which greatly influence how external forces are transmitted throughout the body. Further, hormones, sociological factors, and activity patterns may dictate why one sex is at greater risk of injury than the other. This should be taken into consideration when prescribing training and nutritional programs, as well as evaluating whether recommendations from research studies apply to one or both sexes. As an example, women are roughly five times more likely to tear an anterior cruciate ligament than men in similar sports. This seems to be due to anatomical differences combined with quadriceps dominance in muscle cocontraction over the knee during landing tasks in females (Ford et al. 2011). Sex affects not only the dimensions of the skeleton but also the coordination strategies adopted by athletes.
Nutrition
We are what we eat. Diet has a direct influence on the elements and minerals present in the body that are pivotal to proper function of the musculoskeletal system. Bone relies on calcium, an inorganic compound that the body does not produce on its own, to improve its strength and structural rigidity. Since calcium is secreted throughout the day, an adequate supply is needed in order to maintain mechanical strength. Women stop gaining new bone mass around the age of 30, so it is particularly important for them to maximize calcium intake prior to this age to reduce the chance of osteopenia or osteoporosis (diseases characterized by weak and fragile bones). Further, a core part of the adaptation and healing process is replenishing chemical and mineral deficiencies in the injured area. After an intense workout, athletes are encouraged to consume meals that contain high levels of protein and carbohydrate to facilitate the rebuilding of muscle. Proper levels of key proteins, fats, and other nutrients must exist in the body to facilitate the strengthening and healing of tissue.
Exercise
As discussed earlier, physical activity and normal loading lead to natural modeling and remodeling of body tissue. Bone responds to everyday loading by building new bone mass and remodeling existing bone mass to withstand future similar loading profiles. Normal loading through exercise also causes tendons and ligaments to grow larger or denser, increasing their stiffness and mechanical strength. Muscles respond directly to training and exercise by adapting their fiber structure and material composition. Resistance strength training will cause muscle to add fibers in series, increasing overall contractile strength; stretching will cause muscle fibers to be added in parallel, reducing stiffness and passive forces.
Other Factors
Genetics, disease, and drugs also have substantial effects on the mechanical and material properties of the musculoskeletal system. We already saw that the fast- to slow-twitch muscle fiber ratio is largely determined by genetics. Further, specific genes have been directly linked to muscle mass regulation in the body (Lee 2004). Various diseases can influence the biomechanics of movement by impeding the normal function of musculoskeletal elements. For example, rheumatoid arthritis is a disease in which the body mistakenly attacks its own joint cartilage, which can lead to pain and subsequent suboptimal gait modifications and loading patterns. Pharmaceutical drugs can have drastically positive and negative effects on an individual's biomechanics. Sometimes, the intention behind the drug is to influence biomechanics (i.e., ibuprofen to reduce pain from the inflammatory response), whereas other times the impact is a side effect (e.g., fluoroquinolones antibiotics increase the risk of tendon tear).
Platelet-rich plasma in treatment for sport injury
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology.
By Amir Mahajer, DO, FAOCPMR, FAAPMR, and Julia Louisa Iafrate, DO, CAQSM, FAAPMR
Platelet-Rich Plasma
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology. These cell lines were thought to have “stem cells” that may proliferate into different tissue types, such as cartilage or tendon in musculoskeletal injuries. This has been found not to be the case. Instead, it's believed that these injections create “intercellular communication” that leads to decreased inflammation, improved function, and even tissue healing (see figure 17.1). Platelet-rich plasma (PRP) is one of these types of therapies that holds promise for healing.

Figure 17.1 Ultrasound guided platelet-rich plasma (PRP) injection for rotator cuff tendinopathy and shoulder impingement syndrome.
© Amir Mahajer, DO
Platelet-rich plasma is a growing therapeutic modality in treating musculoskeletal disorders and particularly for sports injuries. Multiple studies have demonstrated safety and efficacy for athletes with pain and functional decline. Platelets are known to be an important component of clot formation (i.e., after a cut, the bleeding stops due to the presence of platelets). Over the past years, research has identified other possible actions of platelets. Parts of platelets known as growth factors seem to promote tissue healing.
Multiple different preparations of PRP are currently available, including leukocyte-rich versus leukocyte-poor PRP, and mixtures with higher concentrations of platelets or growth factors. The inclusion of leukocytes in these preparations is still debated due to their possible proinflammatory catabolic effect; however, they have a potential role in improved tissue remodeling and increased concentration of growth factors in cases of chronic tendinopathy. Both single- and multiple-spin PRP preparations are available, but it is unknown whether one technique is more therapeutic than the other. It is postulated that higher concentrations of platelets improve clinical outcomes. Though it makes sense to deliver higher concentrations of the factors to the localized injury site to cause recovery, having too many growth factors and cytokines may cause an imbalance in homeostasis and instead slow healing. Lastly, although PRP cryopreservation is safe and seems to preserve the ability to promote healing, storing platelets in freezing conditions can alter the morphology and decrease functional properties. Thus, fresh PRP continues to be favored at this time.
Currently, many professional and collegiate team physicians are using PRP despite a lack of consensus regarding optimal formulations and timing of treatment. While PRP injections do not seem to improve acute pain or decrease risk of relapses, they do appear to result in earlier return to sport in athletes with muscle strains and certain chronic tendinopathies. Additional research is needed to pinpoint the ideal ratio of platelet preparation methods and identify conditions and injuries that would most benefit from these treatments. A standardization for future biologic research has been proposed to help support the use of PRP or cell-based therapies and further advance the science of regenerative medicine.
Understanding concussion and head injury
An impact to the head, neck, or elsewhere to the body causing an acceleration–deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
By Josh Krassen, DO
Concussion
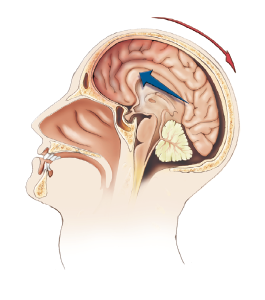
Common Causes
An impact to the head, neck, or elsewhere to the body causing an acceleration-deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
Identification and Prevention
A concussion is a traumatically induced alteration in mental status, such as confusion or amnesia, that may or may not involve a loss of consciousness (Kelly et al. 1991). It is based on functional, not structural, pathology, because imaging is often normal and not diagnostic of injury. There are 1.6 to 3.8 million sports and recreational concussions per year, and 135,000 are seen in the emergency room (Langlois JA et al. 2006). This injury most commonly occurs in American football during tackling or blocking but also occurs in other sports, such as in soccer when a player heads the ball or in ice hockey (more prevalent in women). There is good evidence that helmet use in skiing and snowboarding reduces head injuries. Limiting body checking in youth ice hockey and contact in youth football has also been shown to reduce head injuries. Teaching proper tackling techniques in football and avoidance of heading duels in soccer helps to reduce the risk of concussions. Evidence on use of mouth guards is inconsistent. Athletes with a history of previous concussions are more likely to have recurrent concussions (Guskiewicz et al. 2003).
It is important to have standard policies and protocols in place for education of players, referees, coaching staff, and parents of youth to help identify and understand the signs and symptoms of concussions. Everyone should have an understanding of its clinical features, assessment techniques, and principles for safe return to play. Concussions may involve clinical symptoms, physical signs, cognitive impairment, neurobehavioral features, and sleep-wake disturbances. Athletes can present with headaches, feelings of fogginess and drowsiness, forgetfulness, or irritability, or be emotionally unstable. Gait unsteadiness and slow reaction times are often noted. If any of these symptoms are observed, the athlete should be safely removed from practice or play.
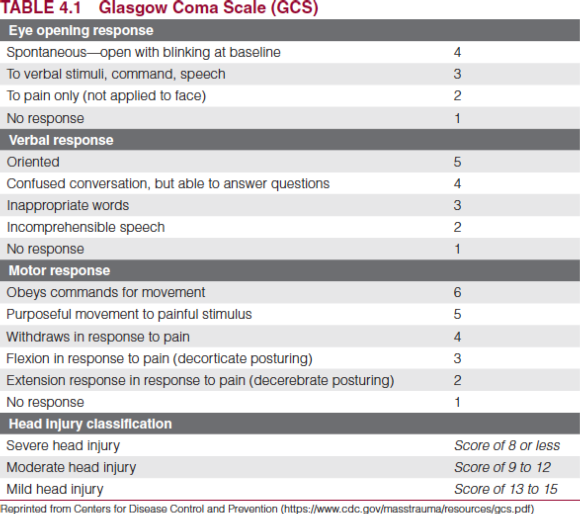
Summary of Concussion Recommendations
- Removal from game with any sign or symptoms of concussion
- No return to play on day of injury
- Medical evaluation following injury, including neuropsychological testing and radiographs to rule out more serious intracranial pathology
- Adherence to stepwise return-to-play process:
- No activity until asymptomatic at rest and during exertion
- Light aerobic exercises
- Sport-specific exercises
- Noncontact drills
- Contact drills
- Game play
Two of the most important factors in determining next steps are the athlete's age and concussion history. Children have more prolonged and diffuse cerebral swelling and are at an increased risk for a second head injury (Pickles 1950). It is important to note that the speed of recovery is the same for all age groups, thus negating the theory that “kids heal faster.” Knowing whether the athlete has a history of concussions at the time of a new injury is important. Cumulative neuropsychological and subtle neurocognitive deficits can be seen after multiple concussions. After three or more concussions, athletes become more vulnerable to subsequent injuries (Collins et al. 2002) and therefore it is recommended that they retire from contact sports.
Overall there is a strong need for clear and practical guidelines to determine recovery and safe return to play for athletes with a sport-related concussion. One must remember that the science of concussion is incomplete, and thus management and return-to-play decisions should still be based on clinical judgment on an individualized basis.
Flexibility training to decrease injury risk
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004).
By Jeff Young, Kinesiologist, CSCS, ACSM-EIM
Flexibility Training
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004). When restrictions exist because of lack of flexibility or mobility, movement is less efficient and the risk of injury increases. Many soft tissue injuries occur during the eccentric (lowering) phase of a movement while the muscles and tendons are under a load and on stretch (lengthening) (Verall and Dolman 2016). If a joint lacks flexibility, maximal or near-maximal lengthening of the muscles surrounding the joint will occur earlier in a movement. If this happens under a load, injury may occur. At a minimum, flexibility should be balanced around each major joint to reduce this risk (see figure 2.1).
To know objectively if a joint has restricted ROM, falls within the norms, or is hypermobile, an assessment should be performed at each major joint. It would behoove the athlete to have a joint ROM assessment performed by a qualified professional. Once this is accomplished, the athlete can be placed on a proper flexibility training program to balance flexibility around each major
joint.
Designing a flexibility program adheres to a principle known as FITT. The letters stand for Frequency, Intensity, Time (duration), and Type.

Figure 2.1 The hamstring is a commonly injured muscle group, so stretching exercises such as the supine hamstring stretch are important to help increase range of motion. Also, it is important to perform a joint range of motion assessment, and if the athlete lacks sufficient range, place the athlete on a proper flexibility training program to reduce the risk of muscle strain.
© Human Kinetics
Frequency
A stretching program should be initiated even if the athlete has normal joint ROM at each joint. In that case, the minimum recommendation of twice per week will be enough to maintain joint ROM. Increased tightness, or movement restriction, calls for an increase in volume. This can be accomplished by increasing the frequency, or sets, or both—the tighter an athlete is, the more stretching is needed. Therefore, joints that fall short of normal ROM (i.e., restricted or “tight” areas) should be stretched three to seven days per week (Garber et al. 2011). Stretching must be done properly and safely. Improper stretching has been shown to increase injury.
Intensity
Intensity lies on a subjective continuum of discomfort or pain that ranges from a “gentle” stretch to “mild discomfort,” “moderate discomfort,” “very uncomfortable,” or “painful.” Interestingly, all levels of discomfort, to include stretching to a point of pain (Muanjai, Jones, and Mickevicius 2017), have been shown to increase flexibility. Logically it is not recommended to stretch to the point of pain, and current evidence recommends stretching to the point of mild to moderate discomfort (Garber et al. 2011).
Time
Stretching durations span a continuum that ranges from 10 to 15 seconds up to several minutes in length. When the goal is to increase joint ROM, the total stretch time across multiple sets is most important. Therefore, athletes have the option of holding a stretch for a longer period of time (e.g., 90 seconds) or dividing the total time into multiple sets (e.g., three sets of 30 seconds) (Frietas et al. 2014).
Type
The several types of stretching include active, passive, dynamic, static, isometric, and proprioceptive neuromuscular facilitation (PNF). Dynamic stretching is the preferred mode of stretching as part of a warm-up prior to a workout or event. Among the other types of stretching, PNF has been shown to be superior in the short term, but all types of stretching can improve joint ROM when performed properly (Garber et al. 2011, Guissard and Duchateau 2006, Page 2012).
It is important to note that muscles are viscoelastic (Ryan et al. 2009, 2012). The viscoelastic property of muscle is what allows it to be deformed (stretched); and although its elasticity will also allow it to return back to its original form, through flexibility training joint ROM can increase above baseline values. If the goal is to maintain joint ROM, athletes should stretch until they reach an “end-range feel” for the given stretch (i.e., the feeling that it would be painful if they proceeded further into the stretch), hold, and release. But if the goal is to increase joint ROM, they should stretch until they reach their end range, hold, mentally relax into the stretch, and then increase the stretch to a new end range. This is known as muscle creep, or “creeping further into the stretch,” and the viscoelastic property of muscle, along with relaxation of the nervous system during the stretch, allows for this. The point: If athletes want to increase joint ROM but stretch only to their first end range (never taking advantage of muscle creep and neural relaxation that allows for an increase in ROM), the body is not signaled to progress, and the stretching will be fruitless. It is imperative to remember to find a second, and if possible, a third end range within each set of a stretch when the goal is to improve flexibility.
Self-myofascial release (SMR) is another method of increasing joint ROM, and while SMR will not directly decrease the chance of injury, because it assists in improving ROM and may increase performance as well, it should be included as part of a flexibility training program and warm-up (Beardsley and Skarabot 2015, Schroeder and Best 2015). While it is beyond the scope of this chapter to provide significant detail, SMR follows the FITT protocol and should be used concurrently with stretching, typically just prior to performing various stretches. Please see Cheatham and colleagues (2015) for more information.
Human factors of the biomechanics of function and injury
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete.
By Adam Gotlin, BS, MS
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete. Specifically, an athlete's age, sex, nutrition, and training all have significant effects on the biomechanics of movement. Even further, genetics, disease, and history of prior injury all influence how people move, the forces they create, and how materials in the body respond to loading. As previously discussed, injury occurs when loads exceed the tolerance of a given tissue. We now discuss the factors contributing to an individual's fitness and risk of injury.
Age
As humans grow, the musculoskeletal system undergoes many dramatic structural changes. During childhood and into the early 20s, human tissue generally develops and grows larger and stronger. In later adulthood, tissue begins to degenerate as wear and tear, toxins, and debris accumulate and outpace the healing powers of the body. The load-bearing capacity of tissue changes dramatically with age. Woo and colleagues tested the tensile strength of cadaver anterior cruciate ligaments for young adults (subject ages 22-35) and older adults (60-97). The young adult tendons could withstand roughly 2,160 N of tensile force before tearing, whereas the average peak force for older adults was 658 N (Woo et al. 1991). This is one of the primary reasons why surgeons commonly repair torn anterior cruciate ligaments using allografts, or donor ligament tissue, in older adults, and autografts, or graft tissue from another location in the patient's body, in young adults. In addition to changes in strength, different structures exist for youth athletes that must be considered when studying the biomechanics of injury. Growth plates are cartilaginous areas of long bones that act as sites for bone growth. Injury to growth plates can yield additional complications. Fractures to the area around growth plates can lead to growth that is misaligned with the normal skeleton or premature closure of the growth plate. Abnormal skeletal geometry can lead to suboptimal force distribution, which can lead to concentrated stresses and future injury.
Sex
There are many factors that contribute to differences in typical biomechanics of males and females. Sex has a large influence on structural anatomy, muscle mass, and skeletal geometry, all of which greatly influence how external forces are transmitted throughout the body. Further, hormones, sociological factors, and activity patterns may dictate why one sex is at greater risk of injury than the other. This should be taken into consideration when prescribing training and nutritional programs, as well as evaluating whether recommendations from research studies apply to one or both sexes. As an example, women are roughly five times more likely to tear an anterior cruciate ligament than men in similar sports. This seems to be due to anatomical differences combined with quadriceps dominance in muscle cocontraction over the knee during landing tasks in females (Ford et al. 2011). Sex affects not only the dimensions of the skeleton but also the coordination strategies adopted by athletes.
Nutrition
We are what we eat. Diet has a direct influence on the elements and minerals present in the body that are pivotal to proper function of the musculoskeletal system. Bone relies on calcium, an inorganic compound that the body does not produce on its own, to improve its strength and structural rigidity. Since calcium is secreted throughout the day, an adequate supply is needed in order to maintain mechanical strength. Women stop gaining new bone mass around the age of 30, so it is particularly important for them to maximize calcium intake prior to this age to reduce the chance of osteopenia or osteoporosis (diseases characterized by weak and fragile bones). Further, a core part of the adaptation and healing process is replenishing chemical and mineral deficiencies in the injured area. After an intense workout, athletes are encouraged to consume meals that contain high levels of protein and carbohydrate to facilitate the rebuilding of muscle. Proper levels of key proteins, fats, and other nutrients must exist in the body to facilitate the strengthening and healing of tissue.
Exercise
As discussed earlier, physical activity and normal loading lead to natural modeling and remodeling of body tissue. Bone responds to everyday loading by building new bone mass and remodeling existing bone mass to withstand future similar loading profiles. Normal loading through exercise also causes tendons and ligaments to grow larger or denser, increasing their stiffness and mechanical strength. Muscles respond directly to training and exercise by adapting their fiber structure and material composition. Resistance strength training will cause muscle to add fibers in series, increasing overall contractile strength; stretching will cause muscle fibers to be added in parallel, reducing stiffness and passive forces.
Other Factors
Genetics, disease, and drugs also have substantial effects on the mechanical and material properties of the musculoskeletal system. We already saw that the fast- to slow-twitch muscle fiber ratio is largely determined by genetics. Further, specific genes have been directly linked to muscle mass regulation in the body (Lee 2004). Various diseases can influence the biomechanics of movement by impeding the normal function of musculoskeletal elements. For example, rheumatoid arthritis is a disease in which the body mistakenly attacks its own joint cartilage, which can lead to pain and subsequent suboptimal gait modifications and loading patterns. Pharmaceutical drugs can have drastically positive and negative effects on an individual's biomechanics. Sometimes, the intention behind the drug is to influence biomechanics (i.e., ibuprofen to reduce pain from the inflammatory response), whereas other times the impact is a side effect (e.g., fluoroquinolones antibiotics increase the risk of tendon tear).
Platelet-rich plasma in treatment for sport injury
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology.
By Amir Mahajer, DO, FAOCPMR, FAAPMR, and Julia Louisa Iafrate, DO, CAQSM, FAAPMR
Platelet-Rich Plasma
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology. These cell lines were thought to have “stem cells” that may proliferate into different tissue types, such as cartilage or tendon in musculoskeletal injuries. This has been found not to be the case. Instead, it's believed that these injections create “intercellular communication” that leads to decreased inflammation, improved function, and even tissue healing (see figure 17.1). Platelet-rich plasma (PRP) is one of these types of therapies that holds promise for healing.

Figure 17.1 Ultrasound guided platelet-rich plasma (PRP) injection for rotator cuff tendinopathy and shoulder impingement syndrome.
© Amir Mahajer, DO
Platelet-rich plasma is a growing therapeutic modality in treating musculoskeletal disorders and particularly for sports injuries. Multiple studies have demonstrated safety and efficacy for athletes with pain and functional decline. Platelets are known to be an important component of clot formation (i.e., after a cut, the bleeding stops due to the presence of platelets). Over the past years, research has identified other possible actions of platelets. Parts of platelets known as growth factors seem to promote tissue healing.
Multiple different preparations of PRP are currently available, including leukocyte-rich versus leukocyte-poor PRP, and mixtures with higher concentrations of platelets or growth factors. The inclusion of leukocytes in these preparations is still debated due to their possible proinflammatory catabolic effect; however, they have a potential role in improved tissue remodeling and increased concentration of growth factors in cases of chronic tendinopathy. Both single- and multiple-spin PRP preparations are available, but it is unknown whether one technique is more therapeutic than the other. It is postulated that higher concentrations of platelets improve clinical outcomes. Though it makes sense to deliver higher concentrations of the factors to the localized injury site to cause recovery, having too many growth factors and cytokines may cause an imbalance in homeostasis and instead slow healing. Lastly, although PRP cryopreservation is safe and seems to preserve the ability to promote healing, storing platelets in freezing conditions can alter the morphology and decrease functional properties. Thus, fresh PRP continues to be favored at this time.
Currently, many professional and collegiate team physicians are using PRP despite a lack of consensus regarding optimal formulations and timing of treatment. While PRP injections do not seem to improve acute pain or decrease risk of relapses, they do appear to result in earlier return to sport in athletes with muscle strains and certain chronic tendinopathies. Additional research is needed to pinpoint the ideal ratio of platelet preparation methods and identify conditions and injuries that would most benefit from these treatments. A standardization for future biologic research has been proposed to help support the use of PRP or cell-based therapies and further advance the science of regenerative medicine.
Understanding concussion and head injury
An impact to the head, neck, or elsewhere to the body causing an acceleration–deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
By Josh Krassen, DO
Concussion
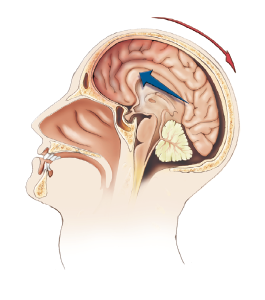
Common Causes
An impact to the head, neck, or elsewhere to the body causing an acceleration-deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
Identification and Prevention
A concussion is a traumatically induced alteration in mental status, such as confusion or amnesia, that may or may not involve a loss of consciousness (Kelly et al. 1991). It is based on functional, not structural, pathology, because imaging is often normal and not diagnostic of injury. There are 1.6 to 3.8 million sports and recreational concussions per year, and 135,000 are seen in the emergency room (Langlois JA et al. 2006). This injury most commonly occurs in American football during tackling or blocking but also occurs in other sports, such as in soccer when a player heads the ball or in ice hockey (more prevalent in women). There is good evidence that helmet use in skiing and snowboarding reduces head injuries. Limiting body checking in youth ice hockey and contact in youth football has also been shown to reduce head injuries. Teaching proper tackling techniques in football and avoidance of heading duels in soccer helps to reduce the risk of concussions. Evidence on use of mouth guards is inconsistent. Athletes with a history of previous concussions are more likely to have recurrent concussions (Guskiewicz et al. 2003).
It is important to have standard policies and protocols in place for education of players, referees, coaching staff, and parents of youth to help identify and understand the signs and symptoms of concussions. Everyone should have an understanding of its clinical features, assessment techniques, and principles for safe return to play. Concussions may involve clinical symptoms, physical signs, cognitive impairment, neurobehavioral features, and sleep-wake disturbances. Athletes can present with headaches, feelings of fogginess and drowsiness, forgetfulness, or irritability, or be emotionally unstable. Gait unsteadiness and slow reaction times are often noted. If any of these symptoms are observed, the athlete should be safely removed from practice or play.
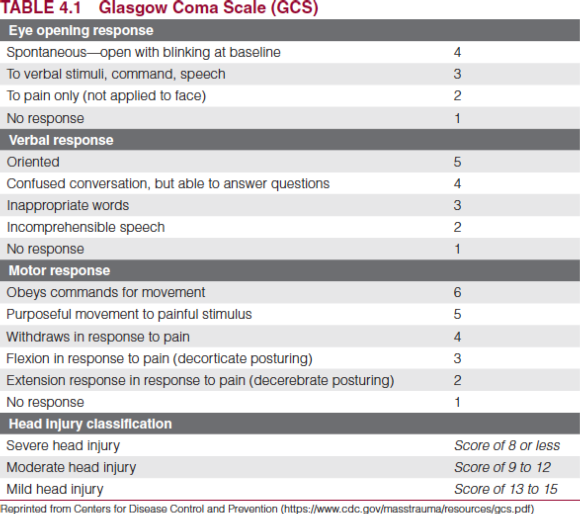
Summary of Concussion Recommendations
- Removal from game with any sign or symptoms of concussion
- No return to play on day of injury
- Medical evaluation following injury, including neuropsychological testing and radiographs to rule out more serious intracranial pathology
- Adherence to stepwise return-to-play process:
- No activity until asymptomatic at rest and during exertion
- Light aerobic exercises
- Sport-specific exercises
- Noncontact drills
- Contact drills
- Game play
Two of the most important factors in determining next steps are the athlete's age and concussion history. Children have more prolonged and diffuse cerebral swelling and are at an increased risk for a second head injury (Pickles 1950). It is important to note that the speed of recovery is the same for all age groups, thus negating the theory that “kids heal faster.” Knowing whether the athlete has a history of concussions at the time of a new injury is important. Cumulative neuropsychological and subtle neurocognitive deficits can be seen after multiple concussions. After three or more concussions, athletes become more vulnerable to subsequent injuries (Collins et al. 2002) and therefore it is recommended that they retire from contact sports.
Overall there is a strong need for clear and practical guidelines to determine recovery and safe return to play for athletes with a sport-related concussion. One must remember that the science of concussion is incomplete, and thus management and return-to-play decisions should still be based on clinical judgment on an individualized basis.
Flexibility training to decrease injury risk
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004).
By Jeff Young, Kinesiologist, CSCS, ACSM-EIM
Flexibility Training
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004). When restrictions exist because of lack of flexibility or mobility, movement is less efficient and the risk of injury increases. Many soft tissue injuries occur during the eccentric (lowering) phase of a movement while the muscles and tendons are under a load and on stretch (lengthening) (Verall and Dolman 2016). If a joint lacks flexibility, maximal or near-maximal lengthening of the muscles surrounding the joint will occur earlier in a movement. If this happens under a load, injury may occur. At a minimum, flexibility should be balanced around each major joint to reduce this risk (see figure 2.1).
To know objectively if a joint has restricted ROM, falls within the norms, or is hypermobile, an assessment should be performed at each major joint. It would behoove the athlete to have a joint ROM assessment performed by a qualified professional. Once this is accomplished, the athlete can be placed on a proper flexibility training program to balance flexibility around each major
joint.
Designing a flexibility program adheres to a principle known as FITT. The letters stand for Frequency, Intensity, Time (duration), and Type.

Figure 2.1 The hamstring is a commonly injured muscle group, so stretching exercises such as the supine hamstring stretch are important to help increase range of motion. Also, it is important to perform a joint range of motion assessment, and if the athlete lacks sufficient range, place the athlete on a proper flexibility training program to reduce the risk of muscle strain.
© Human Kinetics
Frequency
A stretching program should be initiated even if the athlete has normal joint ROM at each joint. In that case, the minimum recommendation of twice per week will be enough to maintain joint ROM. Increased tightness, or movement restriction, calls for an increase in volume. This can be accomplished by increasing the frequency, or sets, or both—the tighter an athlete is, the more stretching is needed. Therefore, joints that fall short of normal ROM (i.e., restricted or “tight” areas) should be stretched three to seven days per week (Garber et al. 2011). Stretching must be done properly and safely. Improper stretching has been shown to increase injury.
Intensity
Intensity lies on a subjective continuum of discomfort or pain that ranges from a “gentle” stretch to “mild discomfort,” “moderate discomfort,” “very uncomfortable,” or “painful.” Interestingly, all levels of discomfort, to include stretching to a point of pain (Muanjai, Jones, and Mickevicius 2017), have been shown to increase flexibility. Logically it is not recommended to stretch to the point of pain, and current evidence recommends stretching to the point of mild to moderate discomfort (Garber et al. 2011).
Time
Stretching durations span a continuum that ranges from 10 to 15 seconds up to several minutes in length. When the goal is to increase joint ROM, the total stretch time across multiple sets is most important. Therefore, athletes have the option of holding a stretch for a longer period of time (e.g., 90 seconds) or dividing the total time into multiple sets (e.g., three sets of 30 seconds) (Frietas et al. 2014).
Type
The several types of stretching include active, passive, dynamic, static, isometric, and proprioceptive neuromuscular facilitation (PNF). Dynamic stretching is the preferred mode of stretching as part of a warm-up prior to a workout or event. Among the other types of stretching, PNF has been shown to be superior in the short term, but all types of stretching can improve joint ROM when performed properly (Garber et al. 2011, Guissard and Duchateau 2006, Page 2012).
It is important to note that muscles are viscoelastic (Ryan et al. 2009, 2012). The viscoelastic property of muscle is what allows it to be deformed (stretched); and although its elasticity will also allow it to return back to its original form, through flexibility training joint ROM can increase above baseline values. If the goal is to maintain joint ROM, athletes should stretch until they reach an “end-range feel” for the given stretch (i.e., the feeling that it would be painful if they proceeded further into the stretch), hold, and release. But if the goal is to increase joint ROM, they should stretch until they reach their end range, hold, mentally relax into the stretch, and then increase the stretch to a new end range. This is known as muscle creep, or “creeping further into the stretch,” and the viscoelastic property of muscle, along with relaxation of the nervous system during the stretch, allows for this. The point: If athletes want to increase joint ROM but stretch only to their first end range (never taking advantage of muscle creep and neural relaxation that allows for an increase in ROM), the body is not signaled to progress, and the stretching will be fruitless. It is imperative to remember to find a second, and if possible, a third end range within each set of a stretch when the goal is to improve flexibility.
Self-myofascial release (SMR) is another method of increasing joint ROM, and while SMR will not directly decrease the chance of injury, because it assists in improving ROM and may increase performance as well, it should be included as part of a flexibility training program and warm-up (Beardsley and Skarabot 2015, Schroeder and Best 2015). While it is beyond the scope of this chapter to provide significant detail, SMR follows the FITT protocol and should be used concurrently with stretching, typically just prior to performing various stretches. Please see Cheatham and colleagues (2015) for more information.
Human factors of the biomechanics of function and injury
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete.
By Adam Gotlin, BS, MS
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete. Specifically, an athlete's age, sex, nutrition, and training all have significant effects on the biomechanics of movement. Even further, genetics, disease, and history of prior injury all influence how people move, the forces they create, and how materials in the body respond to loading. As previously discussed, injury occurs when loads exceed the tolerance of a given tissue. We now discuss the factors contributing to an individual's fitness and risk of injury.
Age
As humans grow, the musculoskeletal system undergoes many dramatic structural changes. During childhood and into the early 20s, human tissue generally develops and grows larger and stronger. In later adulthood, tissue begins to degenerate as wear and tear, toxins, and debris accumulate and outpace the healing powers of the body. The load-bearing capacity of tissue changes dramatically with age. Woo and colleagues tested the tensile strength of cadaver anterior cruciate ligaments for young adults (subject ages 22-35) and older adults (60-97). The young adult tendons could withstand roughly 2,160 N of tensile force before tearing, whereas the average peak force for older adults was 658 N (Woo et al. 1991). This is one of the primary reasons why surgeons commonly repair torn anterior cruciate ligaments using allografts, or donor ligament tissue, in older adults, and autografts, or graft tissue from another location in the patient's body, in young adults. In addition to changes in strength, different structures exist for youth athletes that must be considered when studying the biomechanics of injury. Growth plates are cartilaginous areas of long bones that act as sites for bone growth. Injury to growth plates can yield additional complications. Fractures to the area around growth plates can lead to growth that is misaligned with the normal skeleton or premature closure of the growth plate. Abnormal skeletal geometry can lead to suboptimal force distribution, which can lead to concentrated stresses and future injury.
Sex
There are many factors that contribute to differences in typical biomechanics of males and females. Sex has a large influence on structural anatomy, muscle mass, and skeletal geometry, all of which greatly influence how external forces are transmitted throughout the body. Further, hormones, sociological factors, and activity patterns may dictate why one sex is at greater risk of injury than the other. This should be taken into consideration when prescribing training and nutritional programs, as well as evaluating whether recommendations from research studies apply to one or both sexes. As an example, women are roughly five times more likely to tear an anterior cruciate ligament than men in similar sports. This seems to be due to anatomical differences combined with quadriceps dominance in muscle cocontraction over the knee during landing tasks in females (Ford et al. 2011). Sex affects not only the dimensions of the skeleton but also the coordination strategies adopted by athletes.
Nutrition
We are what we eat. Diet has a direct influence on the elements and minerals present in the body that are pivotal to proper function of the musculoskeletal system. Bone relies on calcium, an inorganic compound that the body does not produce on its own, to improve its strength and structural rigidity. Since calcium is secreted throughout the day, an adequate supply is needed in order to maintain mechanical strength. Women stop gaining new bone mass around the age of 30, so it is particularly important for them to maximize calcium intake prior to this age to reduce the chance of osteopenia or osteoporosis (diseases characterized by weak and fragile bones). Further, a core part of the adaptation and healing process is replenishing chemical and mineral deficiencies in the injured area. After an intense workout, athletes are encouraged to consume meals that contain high levels of protein and carbohydrate to facilitate the rebuilding of muscle. Proper levels of key proteins, fats, and other nutrients must exist in the body to facilitate the strengthening and healing of tissue.
Exercise
As discussed earlier, physical activity and normal loading lead to natural modeling and remodeling of body tissue. Bone responds to everyday loading by building new bone mass and remodeling existing bone mass to withstand future similar loading profiles. Normal loading through exercise also causes tendons and ligaments to grow larger or denser, increasing their stiffness and mechanical strength. Muscles respond directly to training and exercise by adapting their fiber structure and material composition. Resistance strength training will cause muscle to add fibers in series, increasing overall contractile strength; stretching will cause muscle fibers to be added in parallel, reducing stiffness and passive forces.
Other Factors
Genetics, disease, and drugs also have substantial effects on the mechanical and material properties of the musculoskeletal system. We already saw that the fast- to slow-twitch muscle fiber ratio is largely determined by genetics. Further, specific genes have been directly linked to muscle mass regulation in the body (Lee 2004). Various diseases can influence the biomechanics of movement by impeding the normal function of musculoskeletal elements. For example, rheumatoid arthritis is a disease in which the body mistakenly attacks its own joint cartilage, which can lead to pain and subsequent suboptimal gait modifications and loading patterns. Pharmaceutical drugs can have drastically positive and negative effects on an individual's biomechanics. Sometimes, the intention behind the drug is to influence biomechanics (i.e., ibuprofen to reduce pain from the inflammatory response), whereas other times the impact is a side effect (e.g., fluoroquinolones antibiotics increase the risk of tendon tear).
Platelet-rich plasma in treatment for sport injury
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology.
By Amir Mahajer, DO, FAOCPMR, FAAPMR, and Julia Louisa Iafrate, DO, CAQSM, FAAPMR
Platelet-Rich Plasma
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology. These cell lines were thought to have “stem cells” that may proliferate into different tissue types, such as cartilage or tendon in musculoskeletal injuries. This has been found not to be the case. Instead, it's believed that these injections create “intercellular communication” that leads to decreased inflammation, improved function, and even tissue healing (see figure 17.1). Platelet-rich plasma (PRP) is one of these types of therapies that holds promise for healing.

Figure 17.1 Ultrasound guided platelet-rich plasma (PRP) injection for rotator cuff tendinopathy and shoulder impingement syndrome.
© Amir Mahajer, DO
Platelet-rich plasma is a growing therapeutic modality in treating musculoskeletal disorders and particularly for sports injuries. Multiple studies have demonstrated safety and efficacy for athletes with pain and functional decline. Platelets are known to be an important component of clot formation (i.e., after a cut, the bleeding stops due to the presence of platelets). Over the past years, research has identified other possible actions of platelets. Parts of platelets known as growth factors seem to promote tissue healing.
Multiple different preparations of PRP are currently available, including leukocyte-rich versus leukocyte-poor PRP, and mixtures with higher concentrations of platelets or growth factors. The inclusion of leukocytes in these preparations is still debated due to their possible proinflammatory catabolic effect; however, they have a potential role in improved tissue remodeling and increased concentration of growth factors in cases of chronic tendinopathy. Both single- and multiple-spin PRP preparations are available, but it is unknown whether one technique is more therapeutic than the other. It is postulated that higher concentrations of platelets improve clinical outcomes. Though it makes sense to deliver higher concentrations of the factors to the localized injury site to cause recovery, having too many growth factors and cytokines may cause an imbalance in homeostasis and instead slow healing. Lastly, although PRP cryopreservation is safe and seems to preserve the ability to promote healing, storing platelets in freezing conditions can alter the morphology and decrease functional properties. Thus, fresh PRP continues to be favored at this time.
Currently, many professional and collegiate team physicians are using PRP despite a lack of consensus regarding optimal formulations and timing of treatment. While PRP injections do not seem to improve acute pain or decrease risk of relapses, they do appear to result in earlier return to sport in athletes with muscle strains and certain chronic tendinopathies. Additional research is needed to pinpoint the ideal ratio of platelet preparation methods and identify conditions and injuries that would most benefit from these treatments. A standardization for future biologic research has been proposed to help support the use of PRP or cell-based therapies and further advance the science of regenerative medicine.
Understanding concussion and head injury
An impact to the head, neck, or elsewhere to the body causing an acceleration–deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
By Josh Krassen, DO
Concussion
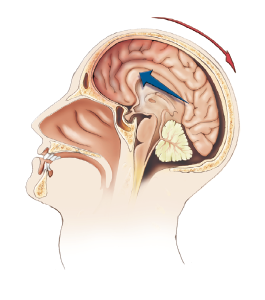
Common Causes
An impact to the head, neck, or elsewhere to the body causing an acceleration-deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
Identification and Prevention
A concussion is a traumatically induced alteration in mental status, such as confusion or amnesia, that may or may not involve a loss of consciousness (Kelly et al. 1991). It is based on functional, not structural, pathology, because imaging is often normal and not diagnostic of injury. There are 1.6 to 3.8 million sports and recreational concussions per year, and 135,000 are seen in the emergency room (Langlois JA et al. 2006). This injury most commonly occurs in American football during tackling or blocking but also occurs in other sports, such as in soccer when a player heads the ball or in ice hockey (more prevalent in women). There is good evidence that helmet use in skiing and snowboarding reduces head injuries. Limiting body checking in youth ice hockey and contact in youth football has also been shown to reduce head injuries. Teaching proper tackling techniques in football and avoidance of heading duels in soccer helps to reduce the risk of concussions. Evidence on use of mouth guards is inconsistent. Athletes with a history of previous concussions are more likely to have recurrent concussions (Guskiewicz et al. 2003).
It is important to have standard policies and protocols in place for education of players, referees, coaching staff, and parents of youth to help identify and understand the signs and symptoms of concussions. Everyone should have an understanding of its clinical features, assessment techniques, and principles for safe return to play. Concussions may involve clinical symptoms, physical signs, cognitive impairment, neurobehavioral features, and sleep-wake disturbances. Athletes can present with headaches, feelings of fogginess and drowsiness, forgetfulness, or irritability, or be emotionally unstable. Gait unsteadiness and slow reaction times are often noted. If any of these symptoms are observed, the athlete should be safely removed from practice or play.
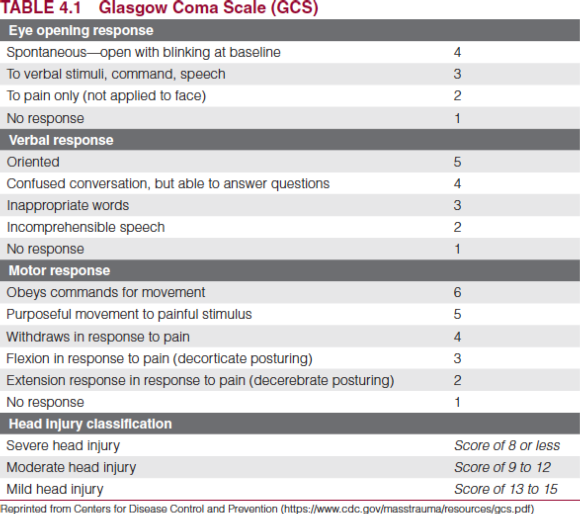
Summary of Concussion Recommendations
- Removal from game with any sign or symptoms of concussion
- No return to play on day of injury
- Medical evaluation following injury, including neuropsychological testing and radiographs to rule out more serious intracranial pathology
- Adherence to stepwise return-to-play process:
- No activity until asymptomatic at rest and during exertion
- Light aerobic exercises
- Sport-specific exercises
- Noncontact drills
- Contact drills
- Game play
Two of the most important factors in determining next steps are the athlete's age and concussion history. Children have more prolonged and diffuse cerebral swelling and are at an increased risk for a second head injury (Pickles 1950). It is important to note that the speed of recovery is the same for all age groups, thus negating the theory that “kids heal faster.” Knowing whether the athlete has a history of concussions at the time of a new injury is important. Cumulative neuropsychological and subtle neurocognitive deficits can be seen after multiple concussions. After three or more concussions, athletes become more vulnerable to subsequent injuries (Collins et al. 2002) and therefore it is recommended that they retire from contact sports.
Overall there is a strong need for clear and practical guidelines to determine recovery and safe return to play for athletes with a sport-related concussion. One must remember that the science of concussion is incomplete, and thus management and return-to-play decisions should still be based on clinical judgment on an individualized basis.
Flexibility training to decrease injury risk
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004).
By Jeff Young, Kinesiologist, CSCS, ACSM-EIM
Flexibility Training
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004). When restrictions exist because of lack of flexibility or mobility, movement is less efficient and the risk of injury increases. Many soft tissue injuries occur during the eccentric (lowering) phase of a movement while the muscles and tendons are under a load and on stretch (lengthening) (Verall and Dolman 2016). If a joint lacks flexibility, maximal or near-maximal lengthening of the muscles surrounding the joint will occur earlier in a movement. If this happens under a load, injury may occur. At a minimum, flexibility should be balanced around each major joint to reduce this risk (see figure 2.1).
To know objectively if a joint has restricted ROM, falls within the norms, or is hypermobile, an assessment should be performed at each major joint. It would behoove the athlete to have a joint ROM assessment performed by a qualified professional. Once this is accomplished, the athlete can be placed on a proper flexibility training program to balance flexibility around each major
joint.
Designing a flexibility program adheres to a principle known as FITT. The letters stand for Frequency, Intensity, Time (duration), and Type.

Figure 2.1 The hamstring is a commonly injured muscle group, so stretching exercises such as the supine hamstring stretch are important to help increase range of motion. Also, it is important to perform a joint range of motion assessment, and if the athlete lacks sufficient range, place the athlete on a proper flexibility training program to reduce the risk of muscle strain.
© Human Kinetics
Frequency
A stretching program should be initiated even if the athlete has normal joint ROM at each joint. In that case, the minimum recommendation of twice per week will be enough to maintain joint ROM. Increased tightness, or movement restriction, calls for an increase in volume. This can be accomplished by increasing the frequency, or sets, or both—the tighter an athlete is, the more stretching is needed. Therefore, joints that fall short of normal ROM (i.e., restricted or “tight” areas) should be stretched three to seven days per week (Garber et al. 2011). Stretching must be done properly and safely. Improper stretching has been shown to increase injury.
Intensity
Intensity lies on a subjective continuum of discomfort or pain that ranges from a “gentle” stretch to “mild discomfort,” “moderate discomfort,” “very uncomfortable,” or “painful.” Interestingly, all levels of discomfort, to include stretching to a point of pain (Muanjai, Jones, and Mickevicius 2017), have been shown to increase flexibility. Logically it is not recommended to stretch to the point of pain, and current evidence recommends stretching to the point of mild to moderate discomfort (Garber et al. 2011).
Time
Stretching durations span a continuum that ranges from 10 to 15 seconds up to several minutes in length. When the goal is to increase joint ROM, the total stretch time across multiple sets is most important. Therefore, athletes have the option of holding a stretch for a longer period of time (e.g., 90 seconds) or dividing the total time into multiple sets (e.g., three sets of 30 seconds) (Frietas et al. 2014).
Type
The several types of stretching include active, passive, dynamic, static, isometric, and proprioceptive neuromuscular facilitation (PNF). Dynamic stretching is the preferred mode of stretching as part of a warm-up prior to a workout or event. Among the other types of stretching, PNF has been shown to be superior in the short term, but all types of stretching can improve joint ROM when performed properly (Garber et al. 2011, Guissard and Duchateau 2006, Page 2012).
It is important to note that muscles are viscoelastic (Ryan et al. 2009, 2012). The viscoelastic property of muscle is what allows it to be deformed (stretched); and although its elasticity will also allow it to return back to its original form, through flexibility training joint ROM can increase above baseline values. If the goal is to maintain joint ROM, athletes should stretch until they reach an “end-range feel” for the given stretch (i.e., the feeling that it would be painful if they proceeded further into the stretch), hold, and release. But if the goal is to increase joint ROM, they should stretch until they reach their end range, hold, mentally relax into the stretch, and then increase the stretch to a new end range. This is known as muscle creep, or “creeping further into the stretch,” and the viscoelastic property of muscle, along with relaxation of the nervous system during the stretch, allows for this. The point: If athletes want to increase joint ROM but stretch only to their first end range (never taking advantage of muscle creep and neural relaxation that allows for an increase in ROM), the body is not signaled to progress, and the stretching will be fruitless. It is imperative to remember to find a second, and if possible, a third end range within each set of a stretch when the goal is to improve flexibility.
Self-myofascial release (SMR) is another method of increasing joint ROM, and while SMR will not directly decrease the chance of injury, because it assists in improving ROM and may increase performance as well, it should be included as part of a flexibility training program and warm-up (Beardsley and Skarabot 2015, Schroeder and Best 2015). While it is beyond the scope of this chapter to provide significant detail, SMR follows the FITT protocol and should be used concurrently with stretching, typically just prior to performing various stretches. Please see Cheatham and colleagues (2015) for more information.
Human factors of the biomechanics of function and injury
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete.
By Adam Gotlin, BS, MS
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete. Specifically, an athlete's age, sex, nutrition, and training all have significant effects on the biomechanics of movement. Even further, genetics, disease, and history of prior injury all influence how people move, the forces they create, and how materials in the body respond to loading. As previously discussed, injury occurs when loads exceed the tolerance of a given tissue. We now discuss the factors contributing to an individual's fitness and risk of injury.
Age
As humans grow, the musculoskeletal system undergoes many dramatic structural changes. During childhood and into the early 20s, human tissue generally develops and grows larger and stronger. In later adulthood, tissue begins to degenerate as wear and tear, toxins, and debris accumulate and outpace the healing powers of the body. The load-bearing capacity of tissue changes dramatically with age. Woo and colleagues tested the tensile strength of cadaver anterior cruciate ligaments for young adults (subject ages 22-35) and older adults (60-97). The young adult tendons could withstand roughly 2,160 N of tensile force before tearing, whereas the average peak force for older adults was 658 N (Woo et al. 1991). This is one of the primary reasons why surgeons commonly repair torn anterior cruciate ligaments using allografts, or donor ligament tissue, in older adults, and autografts, or graft tissue from another location in the patient's body, in young adults. In addition to changes in strength, different structures exist for youth athletes that must be considered when studying the biomechanics of injury. Growth plates are cartilaginous areas of long bones that act as sites for bone growth. Injury to growth plates can yield additional complications. Fractures to the area around growth plates can lead to growth that is misaligned with the normal skeleton or premature closure of the growth plate. Abnormal skeletal geometry can lead to suboptimal force distribution, which can lead to concentrated stresses and future injury.
Sex
There are many factors that contribute to differences in typical biomechanics of males and females. Sex has a large influence on structural anatomy, muscle mass, and skeletal geometry, all of which greatly influence how external forces are transmitted throughout the body. Further, hormones, sociological factors, and activity patterns may dictate why one sex is at greater risk of injury than the other. This should be taken into consideration when prescribing training and nutritional programs, as well as evaluating whether recommendations from research studies apply to one or both sexes. As an example, women are roughly five times more likely to tear an anterior cruciate ligament than men in similar sports. This seems to be due to anatomical differences combined with quadriceps dominance in muscle cocontraction over the knee during landing tasks in females (Ford et al. 2011). Sex affects not only the dimensions of the skeleton but also the coordination strategies adopted by athletes.
Nutrition
We are what we eat. Diet has a direct influence on the elements and minerals present in the body that are pivotal to proper function of the musculoskeletal system. Bone relies on calcium, an inorganic compound that the body does not produce on its own, to improve its strength and structural rigidity. Since calcium is secreted throughout the day, an adequate supply is needed in order to maintain mechanical strength. Women stop gaining new bone mass around the age of 30, so it is particularly important for them to maximize calcium intake prior to this age to reduce the chance of osteopenia or osteoporosis (diseases characterized by weak and fragile bones). Further, a core part of the adaptation and healing process is replenishing chemical and mineral deficiencies in the injured area. After an intense workout, athletes are encouraged to consume meals that contain high levels of protein and carbohydrate to facilitate the rebuilding of muscle. Proper levels of key proteins, fats, and other nutrients must exist in the body to facilitate the strengthening and healing of tissue.
Exercise
As discussed earlier, physical activity and normal loading lead to natural modeling and remodeling of body tissue. Bone responds to everyday loading by building new bone mass and remodeling existing bone mass to withstand future similar loading profiles. Normal loading through exercise also causes tendons and ligaments to grow larger or denser, increasing their stiffness and mechanical strength. Muscles respond directly to training and exercise by adapting their fiber structure and material composition. Resistance strength training will cause muscle to add fibers in series, increasing overall contractile strength; stretching will cause muscle fibers to be added in parallel, reducing stiffness and passive forces.
Other Factors
Genetics, disease, and drugs also have substantial effects on the mechanical and material properties of the musculoskeletal system. We already saw that the fast- to slow-twitch muscle fiber ratio is largely determined by genetics. Further, specific genes have been directly linked to muscle mass regulation in the body (Lee 2004). Various diseases can influence the biomechanics of movement by impeding the normal function of musculoskeletal elements. For example, rheumatoid arthritis is a disease in which the body mistakenly attacks its own joint cartilage, which can lead to pain and subsequent suboptimal gait modifications and loading patterns. Pharmaceutical drugs can have drastically positive and negative effects on an individual's biomechanics. Sometimes, the intention behind the drug is to influence biomechanics (i.e., ibuprofen to reduce pain from the inflammatory response), whereas other times the impact is a side effect (e.g., fluoroquinolones antibiotics increase the risk of tendon tear).
Platelet-rich plasma in treatment for sport injury
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology.
By Amir Mahajer, DO, FAOCPMR, FAAPMR, and Julia Louisa Iafrate, DO, CAQSM, FAAPMR
Platelet-Rich Plasma
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology. These cell lines were thought to have “stem cells” that may proliferate into different tissue types, such as cartilage or tendon in musculoskeletal injuries. This has been found not to be the case. Instead, it's believed that these injections create “intercellular communication” that leads to decreased inflammation, improved function, and even tissue healing (see figure 17.1). Platelet-rich plasma (PRP) is one of these types of therapies that holds promise for healing.

Figure 17.1 Ultrasound guided platelet-rich plasma (PRP) injection for rotator cuff tendinopathy and shoulder impingement syndrome.
© Amir Mahajer, DO
Platelet-rich plasma is a growing therapeutic modality in treating musculoskeletal disorders and particularly for sports injuries. Multiple studies have demonstrated safety and efficacy for athletes with pain and functional decline. Platelets are known to be an important component of clot formation (i.e., after a cut, the bleeding stops due to the presence of platelets). Over the past years, research has identified other possible actions of platelets. Parts of platelets known as growth factors seem to promote tissue healing.
Multiple different preparations of PRP are currently available, including leukocyte-rich versus leukocyte-poor PRP, and mixtures with higher concentrations of platelets or growth factors. The inclusion of leukocytes in these preparations is still debated due to their possible proinflammatory catabolic effect; however, they have a potential role in improved tissue remodeling and increased concentration of growth factors in cases of chronic tendinopathy. Both single- and multiple-spin PRP preparations are available, but it is unknown whether one technique is more therapeutic than the other. It is postulated that higher concentrations of platelets improve clinical outcomes. Though it makes sense to deliver higher concentrations of the factors to the localized injury site to cause recovery, having too many growth factors and cytokines may cause an imbalance in homeostasis and instead slow healing. Lastly, although PRP cryopreservation is safe and seems to preserve the ability to promote healing, storing platelets in freezing conditions can alter the morphology and decrease functional properties. Thus, fresh PRP continues to be favored at this time.
Currently, many professional and collegiate team physicians are using PRP despite a lack of consensus regarding optimal formulations and timing of treatment. While PRP injections do not seem to improve acute pain or decrease risk of relapses, they do appear to result in earlier return to sport in athletes with muscle strains and certain chronic tendinopathies. Additional research is needed to pinpoint the ideal ratio of platelet preparation methods and identify conditions and injuries that would most benefit from these treatments. A standardization for future biologic research has been proposed to help support the use of PRP or cell-based therapies and further advance the science of regenerative medicine.
Understanding concussion and head injury
An impact to the head, neck, or elsewhere to the body causing an acceleration–deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
By Josh Krassen, DO
Concussion
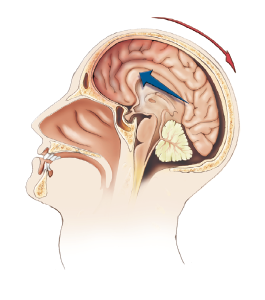
Common Causes
An impact to the head, neck, or elsewhere to the body causing an acceleration-deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
Identification and Prevention
A concussion is a traumatically induced alteration in mental status, such as confusion or amnesia, that may or may not involve a loss of consciousness (Kelly et al. 1991). It is based on functional, not structural, pathology, because imaging is often normal and not diagnostic of injury. There are 1.6 to 3.8 million sports and recreational concussions per year, and 135,000 are seen in the emergency room (Langlois JA et al. 2006). This injury most commonly occurs in American football during tackling or blocking but also occurs in other sports, such as in soccer when a player heads the ball or in ice hockey (more prevalent in women). There is good evidence that helmet use in skiing and snowboarding reduces head injuries. Limiting body checking in youth ice hockey and contact in youth football has also been shown to reduce head injuries. Teaching proper tackling techniques in football and avoidance of heading duels in soccer helps to reduce the risk of concussions. Evidence on use of mouth guards is inconsistent. Athletes with a history of previous concussions are more likely to have recurrent concussions (Guskiewicz et al. 2003).
It is important to have standard policies and protocols in place for education of players, referees, coaching staff, and parents of youth to help identify and understand the signs and symptoms of concussions. Everyone should have an understanding of its clinical features, assessment techniques, and principles for safe return to play. Concussions may involve clinical symptoms, physical signs, cognitive impairment, neurobehavioral features, and sleep-wake disturbances. Athletes can present with headaches, feelings of fogginess and drowsiness, forgetfulness, or irritability, or be emotionally unstable. Gait unsteadiness and slow reaction times are often noted. If any of these symptoms are observed, the athlete should be safely removed from practice or play.
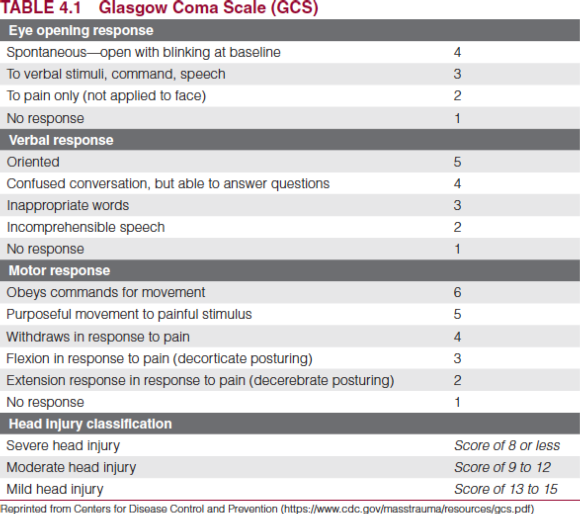
Summary of Concussion Recommendations
- Removal from game with any sign or symptoms of concussion
- No return to play on day of injury
- Medical evaluation following injury, including neuropsychological testing and radiographs to rule out more serious intracranial pathology
- Adherence to stepwise return-to-play process:
- No activity until asymptomatic at rest and during exertion
- Light aerobic exercises
- Sport-specific exercises
- Noncontact drills
- Contact drills
- Game play
Two of the most important factors in determining next steps are the athlete's age and concussion history. Children have more prolonged and diffuse cerebral swelling and are at an increased risk for a second head injury (Pickles 1950). It is important to note that the speed of recovery is the same for all age groups, thus negating the theory that “kids heal faster.” Knowing whether the athlete has a history of concussions at the time of a new injury is important. Cumulative neuropsychological and subtle neurocognitive deficits can be seen after multiple concussions. After three or more concussions, athletes become more vulnerable to subsequent injuries (Collins et al. 2002) and therefore it is recommended that they retire from contact sports.
Overall there is a strong need for clear and practical guidelines to determine recovery and safe return to play for athletes with a sport-related concussion. One must remember that the science of concussion is incomplete, and thus management and return-to-play decisions should still be based on clinical judgment on an individualized basis.
Flexibility training to decrease injury risk
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004).
By Jeff Young, Kinesiologist, CSCS, ACSM-EIM
Flexibility Training
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004). When restrictions exist because of lack of flexibility or mobility, movement is less efficient and the risk of injury increases. Many soft tissue injuries occur during the eccentric (lowering) phase of a movement while the muscles and tendons are under a load and on stretch (lengthening) (Verall and Dolman 2016). If a joint lacks flexibility, maximal or near-maximal lengthening of the muscles surrounding the joint will occur earlier in a movement. If this happens under a load, injury may occur. At a minimum, flexibility should be balanced around each major joint to reduce this risk (see figure 2.1).
To know objectively if a joint has restricted ROM, falls within the norms, or is hypermobile, an assessment should be performed at each major joint. It would behoove the athlete to have a joint ROM assessment performed by a qualified professional. Once this is accomplished, the athlete can be placed on a proper flexibility training program to balance flexibility around each major
joint.
Designing a flexibility program adheres to a principle known as FITT. The letters stand for Frequency, Intensity, Time (duration), and Type.

Figure 2.1 The hamstring is a commonly injured muscle group, so stretching exercises such as the supine hamstring stretch are important to help increase range of motion. Also, it is important to perform a joint range of motion assessment, and if the athlete lacks sufficient range, place the athlete on a proper flexibility training program to reduce the risk of muscle strain.
© Human Kinetics
Frequency
A stretching program should be initiated even if the athlete has normal joint ROM at each joint. In that case, the minimum recommendation of twice per week will be enough to maintain joint ROM. Increased tightness, or movement restriction, calls for an increase in volume. This can be accomplished by increasing the frequency, or sets, or both—the tighter an athlete is, the more stretching is needed. Therefore, joints that fall short of normal ROM (i.e., restricted or “tight” areas) should be stretched three to seven days per week (Garber et al. 2011). Stretching must be done properly and safely. Improper stretching has been shown to increase injury.
Intensity
Intensity lies on a subjective continuum of discomfort or pain that ranges from a “gentle” stretch to “mild discomfort,” “moderate discomfort,” “very uncomfortable,” or “painful.” Interestingly, all levels of discomfort, to include stretching to a point of pain (Muanjai, Jones, and Mickevicius 2017), have been shown to increase flexibility. Logically it is not recommended to stretch to the point of pain, and current evidence recommends stretching to the point of mild to moderate discomfort (Garber et al. 2011).
Time
Stretching durations span a continuum that ranges from 10 to 15 seconds up to several minutes in length. When the goal is to increase joint ROM, the total stretch time across multiple sets is most important. Therefore, athletes have the option of holding a stretch for a longer period of time (e.g., 90 seconds) or dividing the total time into multiple sets (e.g., three sets of 30 seconds) (Frietas et al. 2014).
Type
The several types of stretching include active, passive, dynamic, static, isometric, and proprioceptive neuromuscular facilitation (PNF). Dynamic stretching is the preferred mode of stretching as part of a warm-up prior to a workout or event. Among the other types of stretching, PNF has been shown to be superior in the short term, but all types of stretching can improve joint ROM when performed properly (Garber et al. 2011, Guissard and Duchateau 2006, Page 2012).
It is important to note that muscles are viscoelastic (Ryan et al. 2009, 2012). The viscoelastic property of muscle is what allows it to be deformed (stretched); and although its elasticity will also allow it to return back to its original form, through flexibility training joint ROM can increase above baseline values. If the goal is to maintain joint ROM, athletes should stretch until they reach an “end-range feel” for the given stretch (i.e., the feeling that it would be painful if they proceeded further into the stretch), hold, and release. But if the goal is to increase joint ROM, they should stretch until they reach their end range, hold, mentally relax into the stretch, and then increase the stretch to a new end range. This is known as muscle creep, or “creeping further into the stretch,” and the viscoelastic property of muscle, along with relaxation of the nervous system during the stretch, allows for this. The point: If athletes want to increase joint ROM but stretch only to their first end range (never taking advantage of muscle creep and neural relaxation that allows for an increase in ROM), the body is not signaled to progress, and the stretching will be fruitless. It is imperative to remember to find a second, and if possible, a third end range within each set of a stretch when the goal is to improve flexibility.
Self-myofascial release (SMR) is another method of increasing joint ROM, and while SMR will not directly decrease the chance of injury, because it assists in improving ROM and may increase performance as well, it should be included as part of a flexibility training program and warm-up (Beardsley and Skarabot 2015, Schroeder and Best 2015). While it is beyond the scope of this chapter to provide significant detail, SMR follows the FITT protocol and should be used concurrently with stretching, typically just prior to performing various stretches. Please see Cheatham and colleagues (2015) for more information.
Human factors of the biomechanics of function and injury
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete.
By Adam Gotlin, BS, MS
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete. Specifically, an athlete's age, sex, nutrition, and training all have significant effects on the biomechanics of movement. Even further, genetics, disease, and history of prior injury all influence how people move, the forces they create, and how materials in the body respond to loading. As previously discussed, injury occurs when loads exceed the tolerance of a given tissue. We now discuss the factors contributing to an individual's fitness and risk of injury.
Age
As humans grow, the musculoskeletal system undergoes many dramatic structural changes. During childhood and into the early 20s, human tissue generally develops and grows larger and stronger. In later adulthood, tissue begins to degenerate as wear and tear, toxins, and debris accumulate and outpace the healing powers of the body. The load-bearing capacity of tissue changes dramatically with age. Woo and colleagues tested the tensile strength of cadaver anterior cruciate ligaments for young adults (subject ages 22-35) and older adults (60-97). The young adult tendons could withstand roughly 2,160 N of tensile force before tearing, whereas the average peak force for older adults was 658 N (Woo et al. 1991). This is one of the primary reasons why surgeons commonly repair torn anterior cruciate ligaments using allografts, or donor ligament tissue, in older adults, and autografts, or graft tissue from another location in the patient's body, in young adults. In addition to changes in strength, different structures exist for youth athletes that must be considered when studying the biomechanics of injury. Growth plates are cartilaginous areas of long bones that act as sites for bone growth. Injury to growth plates can yield additional complications. Fractures to the area around growth plates can lead to growth that is misaligned with the normal skeleton or premature closure of the growth plate. Abnormal skeletal geometry can lead to suboptimal force distribution, which can lead to concentrated stresses and future injury.
Sex
There are many factors that contribute to differences in typical biomechanics of males and females. Sex has a large influence on structural anatomy, muscle mass, and skeletal geometry, all of which greatly influence how external forces are transmitted throughout the body. Further, hormones, sociological factors, and activity patterns may dictate why one sex is at greater risk of injury than the other. This should be taken into consideration when prescribing training and nutritional programs, as well as evaluating whether recommendations from research studies apply to one or both sexes. As an example, women are roughly five times more likely to tear an anterior cruciate ligament than men in similar sports. This seems to be due to anatomical differences combined with quadriceps dominance in muscle cocontraction over the knee during landing tasks in females (Ford et al. 2011). Sex affects not only the dimensions of the skeleton but also the coordination strategies adopted by athletes.
Nutrition
We are what we eat. Diet has a direct influence on the elements and minerals present in the body that are pivotal to proper function of the musculoskeletal system. Bone relies on calcium, an inorganic compound that the body does not produce on its own, to improve its strength and structural rigidity. Since calcium is secreted throughout the day, an adequate supply is needed in order to maintain mechanical strength. Women stop gaining new bone mass around the age of 30, so it is particularly important for them to maximize calcium intake prior to this age to reduce the chance of osteopenia or osteoporosis (diseases characterized by weak and fragile bones). Further, a core part of the adaptation and healing process is replenishing chemical and mineral deficiencies in the injured area. After an intense workout, athletes are encouraged to consume meals that contain high levels of protein and carbohydrate to facilitate the rebuilding of muscle. Proper levels of key proteins, fats, and other nutrients must exist in the body to facilitate the strengthening and healing of tissue.
Exercise
As discussed earlier, physical activity and normal loading lead to natural modeling and remodeling of body tissue. Bone responds to everyday loading by building new bone mass and remodeling existing bone mass to withstand future similar loading profiles. Normal loading through exercise also causes tendons and ligaments to grow larger or denser, increasing their stiffness and mechanical strength. Muscles respond directly to training and exercise by adapting their fiber structure and material composition. Resistance strength training will cause muscle to add fibers in series, increasing overall contractile strength; stretching will cause muscle fibers to be added in parallel, reducing stiffness and passive forces.
Other Factors
Genetics, disease, and drugs also have substantial effects on the mechanical and material properties of the musculoskeletal system. We already saw that the fast- to slow-twitch muscle fiber ratio is largely determined by genetics. Further, specific genes have been directly linked to muscle mass regulation in the body (Lee 2004). Various diseases can influence the biomechanics of movement by impeding the normal function of musculoskeletal elements. For example, rheumatoid arthritis is a disease in which the body mistakenly attacks its own joint cartilage, which can lead to pain and subsequent suboptimal gait modifications and loading patterns. Pharmaceutical drugs can have drastically positive and negative effects on an individual's biomechanics. Sometimes, the intention behind the drug is to influence biomechanics (i.e., ibuprofen to reduce pain from the inflammatory response), whereas other times the impact is a side effect (e.g., fluoroquinolones antibiotics increase the risk of tendon tear).
Platelet-rich plasma in treatment for sport injury
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology.
By Amir Mahajer, DO, FAOCPMR, FAAPMR, and Julia Louisa Iafrate, DO, CAQSM, FAAPMR
Platelet-Rich Plasma
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology. These cell lines were thought to have “stem cells” that may proliferate into different tissue types, such as cartilage or tendon in musculoskeletal injuries. This has been found not to be the case. Instead, it's believed that these injections create “intercellular communication” that leads to decreased inflammation, improved function, and even tissue healing (see figure 17.1). Platelet-rich plasma (PRP) is one of these types of therapies that holds promise for healing.

Figure 17.1 Ultrasound guided platelet-rich plasma (PRP) injection for rotator cuff tendinopathy and shoulder impingement syndrome.
© Amir Mahajer, DO
Platelet-rich plasma is a growing therapeutic modality in treating musculoskeletal disorders and particularly for sports injuries. Multiple studies have demonstrated safety and efficacy for athletes with pain and functional decline. Platelets are known to be an important component of clot formation (i.e., after a cut, the bleeding stops due to the presence of platelets). Over the past years, research has identified other possible actions of platelets. Parts of platelets known as growth factors seem to promote tissue healing.
Multiple different preparations of PRP are currently available, including leukocyte-rich versus leukocyte-poor PRP, and mixtures with higher concentrations of platelets or growth factors. The inclusion of leukocytes in these preparations is still debated due to their possible proinflammatory catabolic effect; however, they have a potential role in improved tissue remodeling and increased concentration of growth factors in cases of chronic tendinopathy. Both single- and multiple-spin PRP preparations are available, but it is unknown whether one technique is more therapeutic than the other. It is postulated that higher concentrations of platelets improve clinical outcomes. Though it makes sense to deliver higher concentrations of the factors to the localized injury site to cause recovery, having too many growth factors and cytokines may cause an imbalance in homeostasis and instead slow healing. Lastly, although PRP cryopreservation is safe and seems to preserve the ability to promote healing, storing platelets in freezing conditions can alter the morphology and decrease functional properties. Thus, fresh PRP continues to be favored at this time.
Currently, many professional and collegiate team physicians are using PRP despite a lack of consensus regarding optimal formulations and timing of treatment. While PRP injections do not seem to improve acute pain or decrease risk of relapses, they do appear to result in earlier return to sport in athletes with muscle strains and certain chronic tendinopathies. Additional research is needed to pinpoint the ideal ratio of platelet preparation methods and identify conditions and injuries that would most benefit from these treatments. A standardization for future biologic research has been proposed to help support the use of PRP or cell-based therapies and further advance the science of regenerative medicine.
Understanding concussion and head injury
An impact to the head, neck, or elsewhere to the body causing an acceleration–deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
By Josh Krassen, DO
Concussion
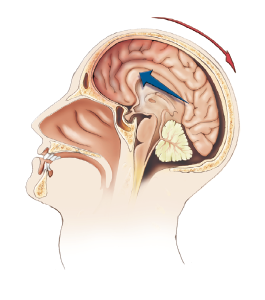
Common Causes
An impact to the head, neck, or elsewhere to the body causing an acceleration-deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
Identification and Prevention
A concussion is a traumatically induced alteration in mental status, such as confusion or amnesia, that may or may not involve a loss of consciousness (Kelly et al. 1991). It is based on functional, not structural, pathology, because imaging is often normal and not diagnostic of injury. There are 1.6 to 3.8 million sports and recreational concussions per year, and 135,000 are seen in the emergency room (Langlois JA et al. 2006). This injury most commonly occurs in American football during tackling or blocking but also occurs in other sports, such as in soccer when a player heads the ball or in ice hockey (more prevalent in women). There is good evidence that helmet use in skiing and snowboarding reduces head injuries. Limiting body checking in youth ice hockey and contact in youth football has also been shown to reduce head injuries. Teaching proper tackling techniques in football and avoidance of heading duels in soccer helps to reduce the risk of concussions. Evidence on use of mouth guards is inconsistent. Athletes with a history of previous concussions are more likely to have recurrent concussions (Guskiewicz et al. 2003).
It is important to have standard policies and protocols in place for education of players, referees, coaching staff, and parents of youth to help identify and understand the signs and symptoms of concussions. Everyone should have an understanding of its clinical features, assessment techniques, and principles for safe return to play. Concussions may involve clinical symptoms, physical signs, cognitive impairment, neurobehavioral features, and sleep-wake disturbances. Athletes can present with headaches, feelings of fogginess and drowsiness, forgetfulness, or irritability, or be emotionally unstable. Gait unsteadiness and slow reaction times are often noted. If any of these symptoms are observed, the athlete should be safely removed from practice or play.
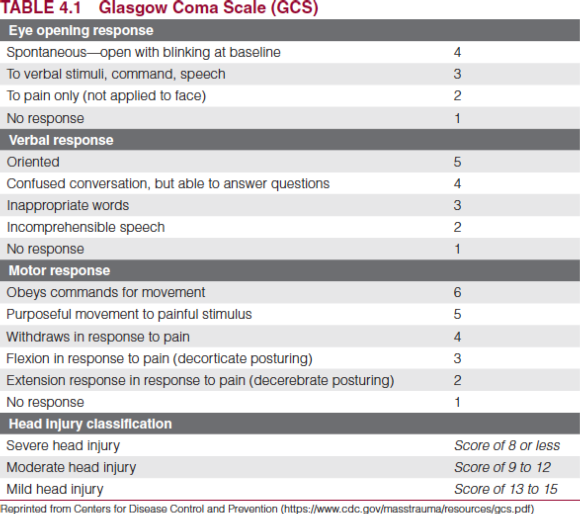
Summary of Concussion Recommendations
- Removal from game with any sign or symptoms of concussion
- No return to play on day of injury
- Medical evaluation following injury, including neuropsychological testing and radiographs to rule out more serious intracranial pathology
- Adherence to stepwise return-to-play process:
- No activity until asymptomatic at rest and during exertion
- Light aerobic exercises
- Sport-specific exercises
- Noncontact drills
- Contact drills
- Game play
Two of the most important factors in determining next steps are the athlete's age and concussion history. Children have more prolonged and diffuse cerebral swelling and are at an increased risk for a second head injury (Pickles 1950). It is important to note that the speed of recovery is the same for all age groups, thus negating the theory that “kids heal faster.” Knowing whether the athlete has a history of concussions at the time of a new injury is important. Cumulative neuropsychological and subtle neurocognitive deficits can be seen after multiple concussions. After three or more concussions, athletes become more vulnerable to subsequent injuries (Collins et al. 2002) and therefore it is recommended that they retire from contact sports.
Overall there is a strong need for clear and practical guidelines to determine recovery and safe return to play for athletes with a sport-related concussion. One must remember that the science of concussion is incomplete, and thus management and return-to-play decisions should still be based on clinical judgment on an individualized basis.
Flexibility training to decrease injury risk
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004).
By Jeff Young, Kinesiologist, CSCS, ACSM-EIM
Flexibility Training
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004). When restrictions exist because of lack of flexibility or mobility, movement is less efficient and the risk of injury increases. Many soft tissue injuries occur during the eccentric (lowering) phase of a movement while the muscles and tendons are under a load and on stretch (lengthening) (Verall and Dolman 2016). If a joint lacks flexibility, maximal or near-maximal lengthening of the muscles surrounding the joint will occur earlier in a movement. If this happens under a load, injury may occur. At a minimum, flexibility should be balanced around each major joint to reduce this risk (see figure 2.1).
To know objectively if a joint has restricted ROM, falls within the norms, or is hypermobile, an assessment should be performed at each major joint. It would behoove the athlete to have a joint ROM assessment performed by a qualified professional. Once this is accomplished, the athlete can be placed on a proper flexibility training program to balance flexibility around each major
joint.
Designing a flexibility program adheres to a principle known as FITT. The letters stand for Frequency, Intensity, Time (duration), and Type.

Figure 2.1 The hamstring is a commonly injured muscle group, so stretching exercises such as the supine hamstring stretch are important to help increase range of motion. Also, it is important to perform a joint range of motion assessment, and if the athlete lacks sufficient range, place the athlete on a proper flexibility training program to reduce the risk of muscle strain.
© Human Kinetics
Frequency
A stretching program should be initiated even if the athlete has normal joint ROM at each joint. In that case, the minimum recommendation of twice per week will be enough to maintain joint ROM. Increased tightness, or movement restriction, calls for an increase in volume. This can be accomplished by increasing the frequency, or sets, or both—the tighter an athlete is, the more stretching is needed. Therefore, joints that fall short of normal ROM (i.e., restricted or “tight” areas) should be stretched three to seven days per week (Garber et al. 2011). Stretching must be done properly and safely. Improper stretching has been shown to increase injury.
Intensity
Intensity lies on a subjective continuum of discomfort or pain that ranges from a “gentle” stretch to “mild discomfort,” “moderate discomfort,” “very uncomfortable,” or “painful.” Interestingly, all levels of discomfort, to include stretching to a point of pain (Muanjai, Jones, and Mickevicius 2017), have been shown to increase flexibility. Logically it is not recommended to stretch to the point of pain, and current evidence recommends stretching to the point of mild to moderate discomfort (Garber et al. 2011).
Time
Stretching durations span a continuum that ranges from 10 to 15 seconds up to several minutes in length. When the goal is to increase joint ROM, the total stretch time across multiple sets is most important. Therefore, athletes have the option of holding a stretch for a longer period of time (e.g., 90 seconds) or dividing the total time into multiple sets (e.g., three sets of 30 seconds) (Frietas et al. 2014).
Type
The several types of stretching include active, passive, dynamic, static, isometric, and proprioceptive neuromuscular facilitation (PNF). Dynamic stretching is the preferred mode of stretching as part of a warm-up prior to a workout or event. Among the other types of stretching, PNF has been shown to be superior in the short term, but all types of stretching can improve joint ROM when performed properly (Garber et al. 2011, Guissard and Duchateau 2006, Page 2012).
It is important to note that muscles are viscoelastic (Ryan et al. 2009, 2012). The viscoelastic property of muscle is what allows it to be deformed (stretched); and although its elasticity will also allow it to return back to its original form, through flexibility training joint ROM can increase above baseline values. If the goal is to maintain joint ROM, athletes should stretch until they reach an “end-range feel” for the given stretch (i.e., the feeling that it would be painful if they proceeded further into the stretch), hold, and release. But if the goal is to increase joint ROM, they should stretch until they reach their end range, hold, mentally relax into the stretch, and then increase the stretch to a new end range. This is known as muscle creep, or “creeping further into the stretch,” and the viscoelastic property of muscle, along with relaxation of the nervous system during the stretch, allows for this. The point: If athletes want to increase joint ROM but stretch only to their first end range (never taking advantage of muscle creep and neural relaxation that allows for an increase in ROM), the body is not signaled to progress, and the stretching will be fruitless. It is imperative to remember to find a second, and if possible, a third end range within each set of a stretch when the goal is to improve flexibility.
Self-myofascial release (SMR) is another method of increasing joint ROM, and while SMR will not directly decrease the chance of injury, because it assists in improving ROM and may increase performance as well, it should be included as part of a flexibility training program and warm-up (Beardsley and Skarabot 2015, Schroeder and Best 2015). While it is beyond the scope of this chapter to provide significant detail, SMR follows the FITT protocol and should be used concurrently with stretching, typically just prior to performing various stretches. Please see Cheatham and colleagues (2015) for more information.
Human factors of the biomechanics of function and injury
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete.
By Adam Gotlin, BS, MS
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete. Specifically, an athlete's age, sex, nutrition, and training all have significant effects on the biomechanics of movement. Even further, genetics, disease, and history of prior injury all influence how people move, the forces they create, and how materials in the body respond to loading. As previously discussed, injury occurs when loads exceed the tolerance of a given tissue. We now discuss the factors contributing to an individual's fitness and risk of injury.
Age
As humans grow, the musculoskeletal system undergoes many dramatic structural changes. During childhood and into the early 20s, human tissue generally develops and grows larger and stronger. In later adulthood, tissue begins to degenerate as wear and tear, toxins, and debris accumulate and outpace the healing powers of the body. The load-bearing capacity of tissue changes dramatically with age. Woo and colleagues tested the tensile strength of cadaver anterior cruciate ligaments for young adults (subject ages 22-35) and older adults (60-97). The young adult tendons could withstand roughly 2,160 N of tensile force before tearing, whereas the average peak force for older adults was 658 N (Woo et al. 1991). This is one of the primary reasons why surgeons commonly repair torn anterior cruciate ligaments using allografts, or donor ligament tissue, in older adults, and autografts, or graft tissue from another location in the patient's body, in young adults. In addition to changes in strength, different structures exist for youth athletes that must be considered when studying the biomechanics of injury. Growth plates are cartilaginous areas of long bones that act as sites for bone growth. Injury to growth plates can yield additional complications. Fractures to the area around growth plates can lead to growth that is misaligned with the normal skeleton or premature closure of the growth plate. Abnormal skeletal geometry can lead to suboptimal force distribution, which can lead to concentrated stresses and future injury.
Sex
There are many factors that contribute to differences in typical biomechanics of males and females. Sex has a large influence on structural anatomy, muscle mass, and skeletal geometry, all of which greatly influence how external forces are transmitted throughout the body. Further, hormones, sociological factors, and activity patterns may dictate why one sex is at greater risk of injury than the other. This should be taken into consideration when prescribing training and nutritional programs, as well as evaluating whether recommendations from research studies apply to one or both sexes. As an example, women are roughly five times more likely to tear an anterior cruciate ligament than men in similar sports. This seems to be due to anatomical differences combined with quadriceps dominance in muscle cocontraction over the knee during landing tasks in females (Ford et al. 2011). Sex affects not only the dimensions of the skeleton but also the coordination strategies adopted by athletes.
Nutrition
We are what we eat. Diet has a direct influence on the elements and minerals present in the body that are pivotal to proper function of the musculoskeletal system. Bone relies on calcium, an inorganic compound that the body does not produce on its own, to improve its strength and structural rigidity. Since calcium is secreted throughout the day, an adequate supply is needed in order to maintain mechanical strength. Women stop gaining new bone mass around the age of 30, so it is particularly important for them to maximize calcium intake prior to this age to reduce the chance of osteopenia or osteoporosis (diseases characterized by weak and fragile bones). Further, a core part of the adaptation and healing process is replenishing chemical and mineral deficiencies in the injured area. After an intense workout, athletes are encouraged to consume meals that contain high levels of protein and carbohydrate to facilitate the rebuilding of muscle. Proper levels of key proteins, fats, and other nutrients must exist in the body to facilitate the strengthening and healing of tissue.
Exercise
As discussed earlier, physical activity and normal loading lead to natural modeling and remodeling of body tissue. Bone responds to everyday loading by building new bone mass and remodeling existing bone mass to withstand future similar loading profiles. Normal loading through exercise also causes tendons and ligaments to grow larger or denser, increasing their stiffness and mechanical strength. Muscles respond directly to training and exercise by adapting their fiber structure and material composition. Resistance strength training will cause muscle to add fibers in series, increasing overall contractile strength; stretching will cause muscle fibers to be added in parallel, reducing stiffness and passive forces.
Other Factors
Genetics, disease, and drugs also have substantial effects on the mechanical and material properties of the musculoskeletal system. We already saw that the fast- to slow-twitch muscle fiber ratio is largely determined by genetics. Further, specific genes have been directly linked to muscle mass regulation in the body (Lee 2004). Various diseases can influence the biomechanics of movement by impeding the normal function of musculoskeletal elements. For example, rheumatoid arthritis is a disease in which the body mistakenly attacks its own joint cartilage, which can lead to pain and subsequent suboptimal gait modifications and loading patterns. Pharmaceutical drugs can have drastically positive and negative effects on an individual's biomechanics. Sometimes, the intention behind the drug is to influence biomechanics (i.e., ibuprofen to reduce pain from the inflammatory response), whereas other times the impact is a side effect (e.g., fluoroquinolones antibiotics increase the risk of tendon tear).
Platelet-rich plasma in treatment for sport injury
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology.
By Amir Mahajer, DO, FAOCPMR, FAAPMR, and Julia Louisa Iafrate, DO, CAQSM, FAAPMR
Platelet-Rich Plasma
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology. These cell lines were thought to have “stem cells” that may proliferate into different tissue types, such as cartilage or tendon in musculoskeletal injuries. This has been found not to be the case. Instead, it's believed that these injections create “intercellular communication” that leads to decreased inflammation, improved function, and even tissue healing (see figure 17.1). Platelet-rich plasma (PRP) is one of these types of therapies that holds promise for healing.

Figure 17.1 Ultrasound guided platelet-rich plasma (PRP) injection for rotator cuff tendinopathy and shoulder impingement syndrome.
© Amir Mahajer, DO
Platelet-rich plasma is a growing therapeutic modality in treating musculoskeletal disorders and particularly for sports injuries. Multiple studies have demonstrated safety and efficacy for athletes with pain and functional decline. Platelets are known to be an important component of clot formation (i.e., after a cut, the bleeding stops due to the presence of platelets). Over the past years, research has identified other possible actions of platelets. Parts of platelets known as growth factors seem to promote tissue healing.
Multiple different preparations of PRP are currently available, including leukocyte-rich versus leukocyte-poor PRP, and mixtures with higher concentrations of platelets or growth factors. The inclusion of leukocytes in these preparations is still debated due to their possible proinflammatory catabolic effect; however, they have a potential role in improved tissue remodeling and increased concentration of growth factors in cases of chronic tendinopathy. Both single- and multiple-spin PRP preparations are available, but it is unknown whether one technique is more therapeutic than the other. It is postulated that higher concentrations of platelets improve clinical outcomes. Though it makes sense to deliver higher concentrations of the factors to the localized injury site to cause recovery, having too many growth factors and cytokines may cause an imbalance in homeostasis and instead slow healing. Lastly, although PRP cryopreservation is safe and seems to preserve the ability to promote healing, storing platelets in freezing conditions can alter the morphology and decrease functional properties. Thus, fresh PRP continues to be favored at this time.
Currently, many professional and collegiate team physicians are using PRP despite a lack of consensus regarding optimal formulations and timing of treatment. While PRP injections do not seem to improve acute pain or decrease risk of relapses, they do appear to result in earlier return to sport in athletes with muscle strains and certain chronic tendinopathies. Additional research is needed to pinpoint the ideal ratio of platelet preparation methods and identify conditions and injuries that would most benefit from these treatments. A standardization for future biologic research has been proposed to help support the use of PRP or cell-based therapies and further advance the science of regenerative medicine.
Understanding concussion and head injury
An impact to the head, neck, or elsewhere to the body causing an acceleration–deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
By Josh Krassen, DO
Concussion
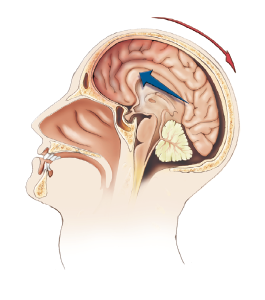
Common Causes
An impact to the head, neck, or elsewhere to the body causing an acceleration-deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
Identification and Prevention
A concussion is a traumatically induced alteration in mental status, such as confusion or amnesia, that may or may not involve a loss of consciousness (Kelly et al. 1991). It is based on functional, not structural, pathology, because imaging is often normal and not diagnostic of injury. There are 1.6 to 3.8 million sports and recreational concussions per year, and 135,000 are seen in the emergency room (Langlois JA et al. 2006). This injury most commonly occurs in American football during tackling or blocking but also occurs in other sports, such as in soccer when a player heads the ball or in ice hockey (more prevalent in women). There is good evidence that helmet use in skiing and snowboarding reduces head injuries. Limiting body checking in youth ice hockey and contact in youth football has also been shown to reduce head injuries. Teaching proper tackling techniques in football and avoidance of heading duels in soccer helps to reduce the risk of concussions. Evidence on use of mouth guards is inconsistent. Athletes with a history of previous concussions are more likely to have recurrent concussions (Guskiewicz et al. 2003).
It is important to have standard policies and protocols in place for education of players, referees, coaching staff, and parents of youth to help identify and understand the signs and symptoms of concussions. Everyone should have an understanding of its clinical features, assessment techniques, and principles for safe return to play. Concussions may involve clinical symptoms, physical signs, cognitive impairment, neurobehavioral features, and sleep-wake disturbances. Athletes can present with headaches, feelings of fogginess and drowsiness, forgetfulness, or irritability, or be emotionally unstable. Gait unsteadiness and slow reaction times are often noted. If any of these symptoms are observed, the athlete should be safely removed from practice or play.
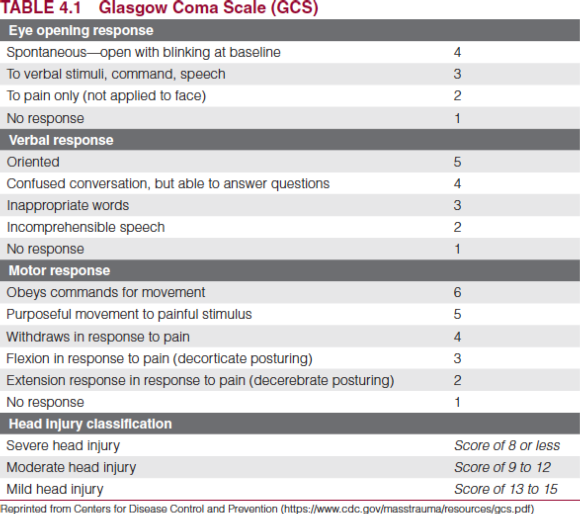
Summary of Concussion Recommendations
- Removal from game with any sign or symptoms of concussion
- No return to play on day of injury
- Medical evaluation following injury, including neuropsychological testing and radiographs to rule out more serious intracranial pathology
- Adherence to stepwise return-to-play process:
- No activity until asymptomatic at rest and during exertion
- Light aerobic exercises
- Sport-specific exercises
- Noncontact drills
- Contact drills
- Game play
Two of the most important factors in determining next steps are the athlete's age and concussion history. Children have more prolonged and diffuse cerebral swelling and are at an increased risk for a second head injury (Pickles 1950). It is important to note that the speed of recovery is the same for all age groups, thus negating the theory that “kids heal faster.” Knowing whether the athlete has a history of concussions at the time of a new injury is important. Cumulative neuropsychological and subtle neurocognitive deficits can be seen after multiple concussions. After three or more concussions, athletes become more vulnerable to subsequent injuries (Collins et al. 2002) and therefore it is recommended that they retire from contact sports.
Overall there is a strong need for clear and practical guidelines to determine recovery and safe return to play for athletes with a sport-related concussion. One must remember that the science of concussion is incomplete, and thus management and return-to-play decisions should still be based on clinical judgment on an individualized basis.
Flexibility training to decrease injury risk
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004).
By Jeff Young, Kinesiologist, CSCS, ACSM-EIM
Flexibility Training
Flexibility, the available range of motion (ROM) around each joint, and mobility, the amount of usable ROM in dynamic, loaded conditions, are important components of both movement and injury prevention (Page 2012, Witvrouw, Mahieu, and Danneels 2004). When restrictions exist because of lack of flexibility or mobility, movement is less efficient and the risk of injury increases. Many soft tissue injuries occur during the eccentric (lowering) phase of a movement while the muscles and tendons are under a load and on stretch (lengthening) (Verall and Dolman 2016). If a joint lacks flexibility, maximal or near-maximal lengthening of the muscles surrounding the joint will occur earlier in a movement. If this happens under a load, injury may occur. At a minimum, flexibility should be balanced around each major joint to reduce this risk (see figure 2.1).
To know objectively if a joint has restricted ROM, falls within the norms, or is hypermobile, an assessment should be performed at each major joint. It would behoove the athlete to have a joint ROM assessment performed by a qualified professional. Once this is accomplished, the athlete can be placed on a proper flexibility training program to balance flexibility around each major
joint.
Designing a flexibility program adheres to a principle known as FITT. The letters stand for Frequency, Intensity, Time (duration), and Type.

Figure 2.1 The hamstring is a commonly injured muscle group, so stretching exercises such as the supine hamstring stretch are important to help increase range of motion. Also, it is important to perform a joint range of motion assessment, and if the athlete lacks sufficient range, place the athlete on a proper flexibility training program to reduce the risk of muscle strain.
© Human Kinetics
Frequency
A stretching program should be initiated even if the athlete has normal joint ROM at each joint. In that case, the minimum recommendation of twice per week will be enough to maintain joint ROM. Increased tightness, or movement restriction, calls for an increase in volume. This can be accomplished by increasing the frequency, or sets, or both—the tighter an athlete is, the more stretching is needed. Therefore, joints that fall short of normal ROM (i.e., restricted or “tight” areas) should be stretched three to seven days per week (Garber et al. 2011). Stretching must be done properly and safely. Improper stretching has been shown to increase injury.
Intensity
Intensity lies on a subjective continuum of discomfort or pain that ranges from a “gentle” stretch to “mild discomfort,” “moderate discomfort,” “very uncomfortable,” or “painful.” Interestingly, all levels of discomfort, to include stretching to a point of pain (Muanjai, Jones, and Mickevicius 2017), have been shown to increase flexibility. Logically it is not recommended to stretch to the point of pain, and current evidence recommends stretching to the point of mild to moderate discomfort (Garber et al. 2011).
Time
Stretching durations span a continuum that ranges from 10 to 15 seconds up to several minutes in length. When the goal is to increase joint ROM, the total stretch time across multiple sets is most important. Therefore, athletes have the option of holding a stretch for a longer period of time (e.g., 90 seconds) or dividing the total time into multiple sets (e.g., three sets of 30 seconds) (Frietas et al. 2014).
Type
The several types of stretching include active, passive, dynamic, static, isometric, and proprioceptive neuromuscular facilitation (PNF). Dynamic stretching is the preferred mode of stretching as part of a warm-up prior to a workout or event. Among the other types of stretching, PNF has been shown to be superior in the short term, but all types of stretching can improve joint ROM when performed properly (Garber et al. 2011, Guissard and Duchateau 2006, Page 2012).
It is important to note that muscles are viscoelastic (Ryan et al. 2009, 2012). The viscoelastic property of muscle is what allows it to be deformed (stretched); and although its elasticity will also allow it to return back to its original form, through flexibility training joint ROM can increase above baseline values. If the goal is to maintain joint ROM, athletes should stretch until they reach an “end-range feel” for the given stretch (i.e., the feeling that it would be painful if they proceeded further into the stretch), hold, and release. But if the goal is to increase joint ROM, they should stretch until they reach their end range, hold, mentally relax into the stretch, and then increase the stretch to a new end range. This is known as muscle creep, or “creeping further into the stretch,” and the viscoelastic property of muscle, along with relaxation of the nervous system during the stretch, allows for this. The point: If athletes want to increase joint ROM but stretch only to their first end range (never taking advantage of muscle creep and neural relaxation that allows for an increase in ROM), the body is not signaled to progress, and the stretching will be fruitless. It is imperative to remember to find a second, and if possible, a third end range within each set of a stretch when the goal is to improve flexibility.
Self-myofascial release (SMR) is another method of increasing joint ROM, and while SMR will not directly decrease the chance of injury, because it assists in improving ROM and may increase performance as well, it should be included as part of a flexibility training program and warm-up (Beardsley and Skarabot 2015, Schroeder and Best 2015). While it is beyond the scope of this chapter to provide significant detail, SMR follows the FITT protocol and should be used concurrently with stretching, typically just prior to performing various stretches. Please see Cheatham and colleagues (2015) for more information.
Human factors of the biomechanics of function and injury
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete.
By Adam Gotlin, BS, MS
It would be irresponsible to present an overview of the biomechanics of function and injury without considering the centerpiece of the entire discussion: the athlete. Specifically, an athlete's age, sex, nutrition, and training all have significant effects on the biomechanics of movement. Even further, genetics, disease, and history of prior injury all influence how people move, the forces they create, and how materials in the body respond to loading. As previously discussed, injury occurs when loads exceed the tolerance of a given tissue. We now discuss the factors contributing to an individual's fitness and risk of injury.
Age
As humans grow, the musculoskeletal system undergoes many dramatic structural changes. During childhood and into the early 20s, human tissue generally develops and grows larger and stronger. In later adulthood, tissue begins to degenerate as wear and tear, toxins, and debris accumulate and outpace the healing powers of the body. The load-bearing capacity of tissue changes dramatically with age. Woo and colleagues tested the tensile strength of cadaver anterior cruciate ligaments for young adults (subject ages 22-35) and older adults (60-97). The young adult tendons could withstand roughly 2,160 N of tensile force before tearing, whereas the average peak force for older adults was 658 N (Woo et al. 1991). This is one of the primary reasons why surgeons commonly repair torn anterior cruciate ligaments using allografts, or donor ligament tissue, in older adults, and autografts, or graft tissue from another location in the patient's body, in young adults. In addition to changes in strength, different structures exist for youth athletes that must be considered when studying the biomechanics of injury. Growth plates are cartilaginous areas of long bones that act as sites for bone growth. Injury to growth plates can yield additional complications. Fractures to the area around growth plates can lead to growth that is misaligned with the normal skeleton or premature closure of the growth plate. Abnormal skeletal geometry can lead to suboptimal force distribution, which can lead to concentrated stresses and future injury.
Sex
There are many factors that contribute to differences in typical biomechanics of males and females. Sex has a large influence on structural anatomy, muscle mass, and skeletal geometry, all of which greatly influence how external forces are transmitted throughout the body. Further, hormones, sociological factors, and activity patterns may dictate why one sex is at greater risk of injury than the other. This should be taken into consideration when prescribing training and nutritional programs, as well as evaluating whether recommendations from research studies apply to one or both sexes. As an example, women are roughly five times more likely to tear an anterior cruciate ligament than men in similar sports. This seems to be due to anatomical differences combined with quadriceps dominance in muscle cocontraction over the knee during landing tasks in females (Ford et al. 2011). Sex affects not only the dimensions of the skeleton but also the coordination strategies adopted by athletes.
Nutrition
We are what we eat. Diet has a direct influence on the elements and minerals present in the body that are pivotal to proper function of the musculoskeletal system. Bone relies on calcium, an inorganic compound that the body does not produce on its own, to improve its strength and structural rigidity. Since calcium is secreted throughout the day, an adequate supply is needed in order to maintain mechanical strength. Women stop gaining new bone mass around the age of 30, so it is particularly important for them to maximize calcium intake prior to this age to reduce the chance of osteopenia or osteoporosis (diseases characterized by weak and fragile bones). Further, a core part of the adaptation and healing process is replenishing chemical and mineral deficiencies in the injured area. After an intense workout, athletes are encouraged to consume meals that contain high levels of protein and carbohydrate to facilitate the rebuilding of muscle. Proper levels of key proteins, fats, and other nutrients must exist in the body to facilitate the strengthening and healing of tissue.
Exercise
As discussed earlier, physical activity and normal loading lead to natural modeling and remodeling of body tissue. Bone responds to everyday loading by building new bone mass and remodeling existing bone mass to withstand future similar loading profiles. Normal loading through exercise also causes tendons and ligaments to grow larger or denser, increasing their stiffness and mechanical strength. Muscles respond directly to training and exercise by adapting their fiber structure and material composition. Resistance strength training will cause muscle to add fibers in series, increasing overall contractile strength; stretching will cause muscle fibers to be added in parallel, reducing stiffness and passive forces.
Other Factors
Genetics, disease, and drugs also have substantial effects on the mechanical and material properties of the musculoskeletal system. We already saw that the fast- to slow-twitch muscle fiber ratio is largely determined by genetics. Further, specific genes have been directly linked to muscle mass regulation in the body (Lee 2004). Various diseases can influence the biomechanics of movement by impeding the normal function of musculoskeletal elements. For example, rheumatoid arthritis is a disease in which the body mistakenly attacks its own joint cartilage, which can lead to pain and subsequent suboptimal gait modifications and loading patterns. Pharmaceutical drugs can have drastically positive and negative effects on an individual's biomechanics. Sometimes, the intention behind the drug is to influence biomechanics (i.e., ibuprofen to reduce pain from the inflammatory response), whereas other times the impact is a side effect (e.g., fluoroquinolones antibiotics increase the risk of tendon tear).
Platelet-rich plasma in treatment for sport injury
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology.
By Amir Mahajer, DO, FAOCPMR, FAAPMR, and Julia Louisa Iafrate, DO, CAQSM, FAAPMR
Platelet-Rich Plasma
Advances in regenerative treatments include cell-based and plasma-based therapies. The idea of regenerative medicine therapies includes injecting live cells originating from bone marrow or adipose (fat) tissue directly at the site of injury or pathology. These cell lines were thought to have “stem cells” that may proliferate into different tissue types, such as cartilage or tendon in musculoskeletal injuries. This has been found not to be the case. Instead, it's believed that these injections create “intercellular communication” that leads to decreased inflammation, improved function, and even tissue healing (see figure 17.1). Platelet-rich plasma (PRP) is one of these types of therapies that holds promise for healing.

Figure 17.1 Ultrasound guided platelet-rich plasma (PRP) injection for rotator cuff tendinopathy and shoulder impingement syndrome.
© Amir Mahajer, DO
Platelet-rich plasma is a growing therapeutic modality in treating musculoskeletal disorders and particularly for sports injuries. Multiple studies have demonstrated safety and efficacy for athletes with pain and functional decline. Platelets are known to be an important component of clot formation (i.e., after a cut, the bleeding stops due to the presence of platelets). Over the past years, research has identified other possible actions of platelets. Parts of platelets known as growth factors seem to promote tissue healing.
Multiple different preparations of PRP are currently available, including leukocyte-rich versus leukocyte-poor PRP, and mixtures with higher concentrations of platelets or growth factors. The inclusion of leukocytes in these preparations is still debated due to their possible proinflammatory catabolic effect; however, they have a potential role in improved tissue remodeling and increased concentration of growth factors in cases of chronic tendinopathy. Both single- and multiple-spin PRP preparations are available, but it is unknown whether one technique is more therapeutic than the other. It is postulated that higher concentrations of platelets improve clinical outcomes. Though it makes sense to deliver higher concentrations of the factors to the localized injury site to cause recovery, having too many growth factors and cytokines may cause an imbalance in homeostasis and instead slow healing. Lastly, although PRP cryopreservation is safe and seems to preserve the ability to promote healing, storing platelets in freezing conditions can alter the morphology and decrease functional properties. Thus, fresh PRP continues to be favored at this time.
Currently, many professional and collegiate team physicians are using PRP despite a lack of consensus regarding optimal formulations and timing of treatment. While PRP injections do not seem to improve acute pain or decrease risk of relapses, they do appear to result in earlier return to sport in athletes with muscle strains and certain chronic tendinopathies. Additional research is needed to pinpoint the ideal ratio of platelet preparation methods and identify conditions and injuries that would most benefit from these treatments. A standardization for future biologic research has been proposed to help support the use of PRP or cell-based therapies and further advance the science of regenerative medicine.
Understanding concussion and head injury
An impact to the head, neck, or elsewhere to the body causing an acceleration–deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
By Josh Krassen, DO
Concussion
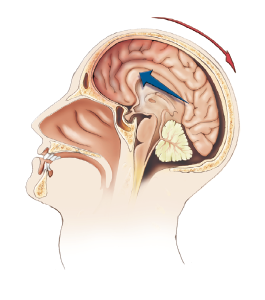
Common Causes
An impact to the head, neck, or elsewhere to the body causing an acceleration-deceleration force to the head may result in a concussion (note that a cervical spine injury should also be suspected with such an injury; see chapter 5).
Identification and Prevention
A concussion is a traumatically induced alteration in mental status, such as confusion or amnesia, that may or may not involve a loss of consciousness (Kelly et al. 1991). It is based on functional, not structural, pathology, because imaging is often normal and not diagnostic of injury. There are 1.6 to 3.8 million sports and recreational concussions per year, and 135,000 are seen in the emergency room (Langlois JA et al. 2006). This injury most commonly occurs in American football during tackling or blocking but also occurs in other sports, such as in soccer when a player heads the ball or in ice hockey (more prevalent in women). There is good evidence that helmet use in skiing and snowboarding reduces head injuries. Limiting body checking in youth ice hockey and contact in youth football has also been shown to reduce head injuries. Teaching proper tackling techniques in football and avoidance of heading duels in soccer helps to reduce the risk of concussions. Evidence on use of mouth guards is inconsistent. Athletes with a history of previous concussions are more likely to have recurrent concussions (Guskiewicz et al. 2003).
It is important to have standard policies and protocols in place for education of players, referees, coaching staff, and parents of youth to help identify and understand the signs and symptoms of concussions. Everyone should have an understanding of its clinical features, assessment techniques, and principles for safe return to play. Concussions may involve clinical symptoms, physical signs, cognitive impairment, neurobehavioral features, and sleep-wake disturbances. Athletes can present with headaches, feelings of fogginess and drowsiness, forgetfulness, or irritability, or be emotionally unstable. Gait unsteadiness and slow reaction times are often noted. If any of these symptoms are observed, the athlete should be safely removed from practice or play.
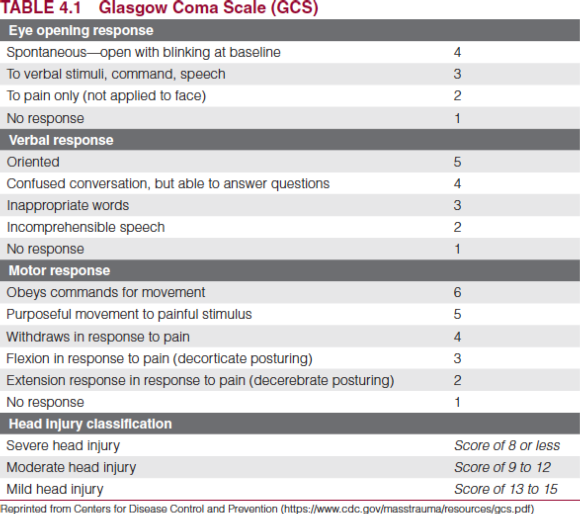
Summary of Concussion Recommendations
- Removal from game with any sign or symptoms of concussion
- No return to play on day of injury
- Medical evaluation following injury, including neuropsychological testing and radiographs to rule out more serious intracranial pathology
- Adherence to stepwise return-to-play process:
- No activity until asymptomatic at rest and during exertion
- Light aerobic exercises
- Sport-specific exercises
- Noncontact drills
- Contact drills
- Game play
Two of the most important factors in determining next steps are the athlete's age and concussion history. Children have more prolonged and diffuse cerebral swelling and are at an increased risk for a second head injury (Pickles 1950). It is important to note that the speed of recovery is the same for all age groups, thus negating the theory that “kids heal faster.” Knowing whether the athlete has a history of concussions at the time of a new injury is important. Cumulative neuropsychological and subtle neurocognitive deficits can be seen after multiple concussions. After three or more concussions, athletes become more vulnerable to subsequent injuries (Collins et al. 2002) and therefore it is recommended that they retire from contact sports.
Overall there is a strong need for clear and practical guidelines to determine recovery and safe return to play for athletes with a sport-related concussion. One must remember that the science of concussion is incomplete, and thus management and return-to-play decisions should still be based on clinical judgment on an individualized basis.