- Home
- Medicine in Exercise and Sport
- Health Care in Exercise and Sport
- Health Care for Special Conditions
- ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities

ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities
Edited by Geoffrey E. Moore, J. Larry Durstine and Patricia L. Painter
by American College of Sports Medicine
416 Pages
The fourth edition of ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities reveals common ground between medical and exercise professionals, creating a more collaborative approach to patient care. Developed by the American College of Sports Medicine (ACSM) with contributions from a specialized team of experts, this text presents a framework for optimizing patients’ and clients’ functionality by keeping them physically active. Featuring new content on common comorbid conditions, this edition is streamlined and updated to better suit chronic populations.
This fourth edition of ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities outlines why exercise is significant in the treatment and prevention of disease, advises medical and exercise professionals in considering proper exercise prescription protocols, and provides evidence-informed guidance on devising individualized exercise programs.
Major advancements and features of the fourth edition include the following:
• Current evidence on exercise management for persons with multiple conditions, providing guidance on working with these common yet complex populations
• A refocused goal of using physical activity to optimize patients’ and clients’ functionality and participation in life activities rather than only to treat and prevent disease
• Specific content to help physicians prescribe physical activity and exercise to patients for promotion of health, well-being, and longevity
• Reorganization of case studies into one streamlined chapter along with commentary from the senior editor to encourage critical thinking and recognize the unique needs of each patient
The case studies in the text are real-life scenarios that help professionals and clinicians combine scientific knowledge with experience to find appropriate solutions for each individual. Commentary on the case studies from the senior editor illustrates when improvisation may be appropriate and where further research is needed. Tables are highlighted throughout the text to help readers quickly reference important clinical information. Evidence-informed guidelines, suggested websites, and additional readings further encourage practical use of information and identify further learning opportunities. For instructors, an ancillary PowerPoint presentation package aids in classroom discussion.
The critical element that distinguishes the fourth edition of ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities is its unifying mission to incorporate physical activity and exercise in both disease treatment and prevention. Its emphasis on assisting people with multiple conditions, which is ever present in health care today, moves beyond primary and secondary prevention to focus on how patients and clients can be kept physically active and functionally fit.
Part I. Foundations of Exercise in Chronic Disease and Disability
Geoffrey E. Moore, J. Larry Durstine, and Patricia L. Painter
Chapter 1. Exercise Is Medicine in Chronic Care
Robert Sallis and Geoffrey E. Moore
Exercise Is Medicine
Take-Home Message
Suggested Readings
Chapter 2. Basic Physical Activity and Exercise Recommendations for Persons With Chronic Conditions
Benjamin T. Gordon, J. Larry Durstine, Patricia L. Painter, and Geoffrey E. Moore
Definitions Used in This Book
Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
How to Prescribe Physical Activity or Exercise in Chronic Care
Graded Exercise Testing
Minimum Exercise Recommendations When an Exercise Test Is Not Available
Clinically Supervised Exercise Programming
ACSM’s Exercise Personnel Certifications
Suggested Readings
Chapter 3. Art of Clinical Exercise Programming
Patricia L. Painter and Geoffrey E. Moore
Step 1: Assess Current Health Status
Step 2: Assess Current Level of Physical Activity
Step 3: Identify Exertional Symptoms That Limit Physical Activity
Step 4: Evaluate Physical Function and Performance
Step 5: Selecting Physical Performance Assessments
Activities of Daily Living and Instrumental Activities of Daily Living
Commonly Used Tests of Physical Functioning
Step 6: Considerations for Formal Exercise Tolerance Testing
Step 7: Considerations for Program Referral
Step 8: Develop a Strategy for Monitoring Progress
Take-Home Message
Suggested Readings
Additional Resources
Chapter 4. Art of Exercise Medicine: Counseling and Socioecological Factors
Geoffrey E. Moore, Michael Costello, and Patricia L. Painter
Common Behavioral Techniques Used in Exercise Counseling
Other Aspects of Exercise Counseling
Socioecological Disparities and Exercise in Chronic Conditions
Integration Into a Medical Home Model
Suggested Readings
Additional Resource
Part II. Common Chronic Conditions and Comorbidities
Geoffrey E. Moore and J. Larry Durstine
Chapter 5. Approach to the Common Chronic Conditions
Geoffrey E. Moore, Patricia L. Painter, J. Larry Durstine, and Benjamin T. Gordon
Nature of Multiple Conditions and Related Comorbidities
General Recommendations for Exercise
Recommendations for Exercise Assessment
Recommendations for Exercise Programming
CDD4 Alternative Recommendation: The Functional Exercise Trial
General Solutions for Common Chronic Conditions
Integration Into a Medical Home Model
Suggested Readings
Chapter 6. Chronic Conditions Strongly Associated With Physical Inactivity
J. Larry Durstine, Geoffrey E. Moore, Patricia L. Painter, Richard Macko, Benjamin T. Gordon, and William E. Kraus
Hypertension and Dyslipidemia
Overweight, Obesity, Prediabetes, and Type 2 Diabetes Mellitus
Arthritis and Back Pain
Osteoporosis
Suggested Readings
Additional Resources
Web Resources
Chapter 7. Chronic Conditions Very Strongly Associated With Tobacco
Christopher B. Cooper, Brett A. Dolezal, J. Larry Durstine, Benjamin T. Gordon, Sherry O. Pinkstaff, Abraham S. Babu, and Shane A. Phillips
Chronic Obstructive Pulmonary Disease
Coronary Artery Disease and Atherosclerosis
Angina and Silent Ischemia
Peripheral Arterial Disease
Suggested Readings
Additional Resources
Chapter 8. Cancer
Kathryn Schmitz
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Suggested Readings
Additional Resources
Chapter 9. Significant Sequelae Related to Common Chronic Conditions
Jessica S. Oldham, Patricia L. Painter, Elizabeth J. Protas, Geoffrey E. Moore, and Richard Macko
Depression as a Comorbidity
Lower-Limb Amputation
Frailty
Suggested Readings
Additional Resource
Part III. Cardiovascular Diseases
Jonathan N. Myers and Peter H. Burbaker
Chapter 10. Chronic Heart Failure
Peter H. Brubaker and Jonathan N. Myers
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 11. Atrial Fibrillation
Jonathan N. Myers and J. Edwin Atwood
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 12. Pacemakers and Implantable Cardioverter-Defibrillators
Clinton A. Brawner and Barry Lewis
Permanent Pacemakers
Implantable Cardioverter-Defibrillators
Combination Pacemaker–Defibrillator Devices
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Suggested Readings
Additional Resources
Chapter 13. Valvular Heart Disease
Matthew W. Parker
Basic Pathophysiology
Mitral Valve Disease
Aortic Valve Disease
Right-Sided Valvular Heart Disease
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 14. Heart Transplantation
Audrey B. Silva and Gerson Cipriano Jr.
Effects on the Exercise Response
Effects of Exercise Training
Management and Medications
Recommendations for Exercise Testing
Recommendations for Exercise Training
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 15. Aneurysms
Holly Fonda and Jonathan N. Myers
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Part IV. Pulmonary Diseases
Tony Babb
Chapter 16. Chronic Restrictive Pulmonary Disease
Connie C. W. Hsia
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Chapter 17. Asthma
Kenneth W. Rundell
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 18. Cystic Fibrosis
Erik Hulzebos, Maarten S. Werkman, Bart C. Bongers, and Tim Takken
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 19. Pulmonary Hypertension
Kelly Chin
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resource
Part V. Immunological, Hematological, and Organ Failure
David C. Nieman
Chapter 20. Chronic Kidney and Liver Disease
Patricia L. Painter
Renal Disease
Liver Disease
Management and Medications for Kidney Disease
Management and Medications for Liver Disease
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 21. Acquired Immune Deficiency Syndrome
David C. Nieman, Gregory A. Hand, G. William Lyerly, and Wesley D. Dudgeon
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 22. Chronic Fatigue Syndrome
Steven P. Bailey and David C. Nieman
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 23. Fibromyalgia
David C. Nieman
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 24. Hemostasis Disorders
Michael Lockard and David C. Nieman
Basic Pathophysiology of Hemorrhagic Disorders
Basic Pathophysiology of Thrombotic Disorders
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Part VI. Neuromuscular Conditions
Elizabeth J. Protas and Richard Macko
Chapter 25. Stroke, Brain Trauma, and Spinal Cord Injuries
Richard Macko
Basic Pathophysiology of Stroke
Basic Pathophysiology of Traumatic Brain Injury
Basic Pathophysiology of Spinal Cord Injury
Common Elements
Systemic Effects of Central Nervous System Injury
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Chapter 26. Peripheral Neuropathy, Myopathy, and Myasthenia Gravis
Charlene Hafer-Macko
Basic Pathophysiology of Peripheral Neuropathy
Basic Pathophysiology of Myopathy
Basic Pathophysiology of Myasthenia Gravis
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 27. Cerebral Palsy
Désirée Maltais
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 28. Multiple Sclerosis
Tara Patterson and Jill Seale
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 29. Parkinson’s Disease
Elizabeth J. Protas and Rhonda K. Stanley
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 30. Muscular Dystrophy
Janke de Groot and Bart Bartels
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Part VII. Cognitive and Psychological Disorders
Bradley D. Hatfield
Chapter 31. Dementia and Alzheimer’s Disease
Jessica S. Oldham, Jo B. Zimmerman, and Bradley D. Hatfield
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Chapter 32. Depression and Anxiety Disorders
Jessica S. Oldham, Jo B. Zimmerman, and Bradley D. Hatfield
Basic Pathophysiology
Management and Medications
Effects on the Exercise Response
Effects of Exercise Training
Recommendations for Exercise Testing
Recommendations for Exercise Programming
Integration Into a Medical Home Model
Take-Home Message
Suggested Readings
Additional Resources
Part VIII Case Studies
Geoffrey E. Moore
Abdominal Aortic Aneurism
Amyotrophic Lateral Sclerosis
Asthma
Atrial Fibrillation
Becker Muscular Dystrophy
Breast Cancer Survivor
Cerebral Palsy
Chronic Fatigue Syndrome
Chronic Heart Failure With Mild COPD
Chronic Kidney Disease: Stage 4, Renal Insufficiency
Chronic Kidney Disease: Stage 5, Treated With Hemodialysis
Chronic Kidney Disease: Status/Post–Renal Transplantation
Chronic Obstructive Pulmonary Disease
Coronary Artery Disease and Dyslipidemia, Status Post-Angioplasty With Stent Placement
Cystic Fibrosis
Deep Venous Thrombosis
Dementia and Frailty
Fibromyalgia
Hearing Impairment
Heart Transplant
Human Immunodeficiency Virus
Hypertension, Dyslipidemia, and Obesity
Interstitial Lung Disease (Chronic Restrictive Lung Disease)
Major Depressive Disorder
Multiple Sclerosis
Myasthenia Gravis
Myocardial Infarction
Parkinson’s Disease
Peripheral Artery Disease
Pulmonary Hypertension
Refractory Angina
Spinal Cord Injury
Stroke
Type 2 Diabetes and Disability From Morbid Obesity With Multiple Chronic Conditions
Type 2 Diabetes and Obesity With Osteoarthrosis
Valvular Heart Disease
Visual Impairment
The American College of Sports Medicine (ACSM), founded in 1954, is a professional membership society with more than 50,000 national, regional, and international members in more than 90 countries dedicated to improving health through science, education, and medicine. ACSM members work in a range of medical specialties, allied health professions, and scientific disciplines. Members are committed to the diagnosis, treatment, and prevention of sport-related injuries and the advancement of the science of exercise.
The ACSM promotes and integrates scientific research, education, and practical applications of sports medicine and exercise science to maintain and enhance physical performance, fitness, health, and quality of life.
Risk factors for coronary artery disease
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis.
Hypertension and Dyslipidemia
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis. When both conditions are present, the likelihood of having clinically significant CAD is drastically increased because atherosclerosis develops in areas of arteries that experience high blood pressure when high levels of low-density lipoprotein (LDL) are present. Because of this interrelationship and the role of exercise in mitigating these two conditions, hypertension and dyslipidemia are discussed here as linked CAD risk factors.
Basic Pathophysiology
The basic pathophysiology of these conditions is closely interrelated but is discussed separately to highlight key issues.
Hypertension
Hypertension (HTN) is a very common chronic condition, affecting about one in five people; it is defined as either
- systolic blood pressure (BP) over 139 mmHg or
- diastolic BP over 89 mmHg.
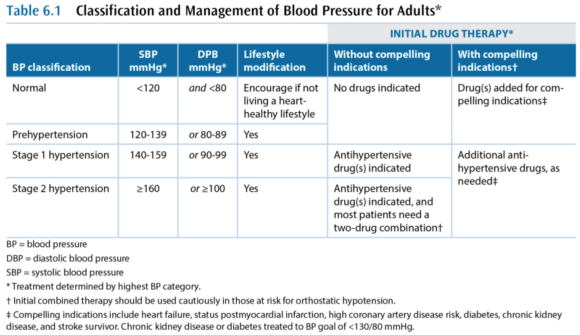
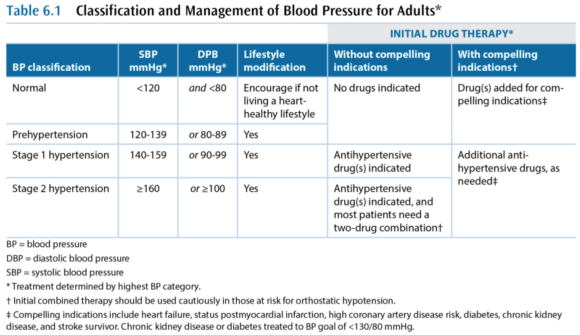
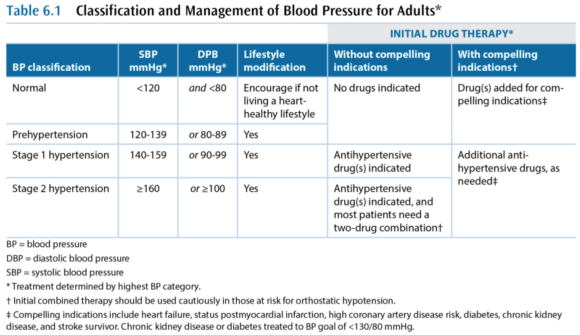
Table 6.1 has a more complete description of the classes of hypertension. High BP increases the risk for nonfatal and fatal cardiovascular disease, particularly CAD, kidney disease, and stroke. Even BP that is increased but not meeting the criteria for hypertension causes cardiovascular disease.
While hypertension is a common condition, the cause is not very well understood. In more than 95% of hypertension cases, the etiology is unknown and the condition is referred to as primary or essential or idiopathic hypertension. The remaining 5% of cases are secondary hypertension, so named because there is an identifiable underlying cause such as sleep apnea, drug-induced or drug-related causes (e.g., chronic corticosteroid therapy), chronic kidney disease, renovascular disease, aldosteronism, Cushing's syndrome, pheochromocytoma, coarctation of the aorta, and hyperthyroidism.
Dyslipidemia
Dyslipidemia - a high level of blood lipids - is a complex set of conditions, but the main concern is a high level of cholesterol. Cholesterol is critically important to every cell in the body, as a constituent of cell membranes that helps regulate their stability. Cholesterol is also an intermediary compound in steroid hormones, but the amount of cholesterol needed for hormones is many orders of magnitude lower than that needed for cell membranes. Cholesterol is synthesized and metabolized in the liver and then transported between the liver and the rest of the body. Cholesterol is not soluble in blood plasma and therefore has to be transported in the blood by lipoproteins. There are many different lipoproteins, each functioning to guide the cholesterol it carries to the proper metabolic pathway. This is the basic triad of lipoproteins:
- Very low-density lipoprotein (VLDL)
- Low-density lipoprotein (LDL)
- High-density lipoprotein (HDL)
The VLDL fraction carries about 80% triglycerides and 20% cholesterol, while the LDL and HDL mainly carry cholesterol. The total blood cholesterol is the sum of the cholesterol bound to VLDL, LDL, and HDL, and these cholesterol subcomponents are indicated with a -C suffix (e.g., LDL-C). Several subclassifications also exist, including two notable subclasses of LDL:
- Lipoprotein (a)
- Small dense LDL
Cholesterol metabolism is extremely complex, but the most important issue is that elevated total cholesterol and low-density lipoprotein cholesterol (LDL-C) are associated with an increased risk of CAD. Lipoprotein (a), or Lp(a), increases risk of CAD and of developing a thrombus, and small dense LDL also increases CAD risk. In contrast, high-density lipoprotein cholesterol (HDL-C) decreases CAD risk, through a cardioprotective effect that is partially related to this lipoprotein's role in the reverse cholesterol transport. In reverse transport, the cholesterol in HDL-C is transported to the liver where it is catabolized and excreted as bile.
Terms Often Used to Refer to Blood Lipids
- dyslipidemia - elevated triglycerides and cholesterol
- hypercholesterolemia - only cholesterol is elevated
- hypertriglyceridemia - only triglycerides are elevated
- exaggerated postprandial lipemia - prolonged elevation of triglycerides following consumption of dietary fat
- hyperlipoproteinemia or dyslipoproteinemia - high lipoprotein concentrations from genetic abnormalities or an underlying condition such as diabetes, renal disease, hypothyroidism, biliary obstruction, or dysproteinemia
Management and Medications
Medical management in persons who have the common chronic conditions often involves one or more medications for each condition, such that people with cardiometabolic conditions are often on five to eight prescription medicines. Again, this discussion treats these independently, but readers should expect to see multiple medications in persons in this group.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Case Study: Diabetes and Obesity with Osteoarthrosis
I intend to live into my 90s but I can’t get there unless I’m dancing. A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk.
Type 2 Diabetes and Obesity With Osteoarthrosis
Presenter: Geoffrey E. Moore, MD, FACSM
S
"I intend to live into my 90s but I can't get there unless I'm dancing."
A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk. Her recent A1c values had been 6.5-6.6, and her a.m. fasting glucose was recently 102. She qualified as T2DM by A1c criteria but wasn't working on her diet or weight and had refused to start taking metformin, and her primary care physician was increasingly concerned.
She expressed a desire to be more active through dance, which she had loved since childhood and felt was a part of her culture (having immigrated to the United States as a child). She expressed little concern about her weight and was more worried that the pain in her L shoulder kept her from dancing. She had first experienced the shoulder problem 10 years earlier while swimming backstroke. She had been to physical therapy (PT) twice, which made it worse. She also had received subacromial cortisone injections, but the relief didn't last. Her shoulder is worse at night (rolls over on her left side); the pain was rated 8/10 and was daily and constant except for sharp pain that radiated to the side of the neck when she moved the shoulder too much. She tried not to take pain or anti-inflammatory medications because she said they "wreck her stomach." Acupuncture (cupping) helped.
She also noted a history of her L knee "giving out," causing falls, and of having 2 knee arthroscopic surgeries (4 and 10 years earlier). When she overdoes weight-bearing activity, her left knee swells "like a watermelon." She did PT after the surgeries and gets to her normal daily activities but can't dance.
O
- Height: 5 ft 4¾ in. (1.65 m)
- Weight: 234.4 lb (106.3 kg)
- BMI: 39 kg/m2
- HR: 65 contractions/min
- BP: 188/98 mmHg
Pertinent Exam
- General: normal development, good nutrition, obese body habitus, no deformities
- CV: regular rhythm with normal S1 and S2, without rubs, gallops, or murmurs; distal pulses/circulation normal; no edema
- Musculoskeletal:
- Normal gait and station, muscular build especially of lower extremities
- Valgus alignment of both knees, no tenderness but the L knee has a small effusion
- Normal ROM without pain, substantial crepitus in both knees
- Left shoulder-specific tests:
- + Painful arc
- + Glenohumeral laxity, with crepitus
- + Neer test, +/- Hawkins test, +/- Speed's test
- + Painful with resisted external rotation, - pain with resisted internal rotation
- + AC joint tenderness
X Rays
- Osteoarthrosis in the acromioclavicular joint; severe osteoarthrosis in the glenohumeral joint with advanced sclerosis, subchondral cysts, and spurring; subluxed position of the humeral head at rest
Medications
- Coreg 10 mg once daily
- Diovan HCT 320/12.5 once daily
- Multivitamin once daily
A
- Increased CV risk: HTN, hyperlipidemia, diabetes by A1c criteria, sleep apnea, obesity
- Advanced glenohumeral osteoarthrosis and reduced function due to pain, status post - bilateral partial meniscectomies
Her shoulder markedly diminishes quality of life, impairing her ability to sleep and to recreate. Dance is her preferred form of physical activity, which she wants to do as her approach to improve the blood glucose and reduce her CV risk profile.
P
- L shoulder OA: refer to PT shoulder specialist
- It was explained that her shoulder would take a long time to get better, but she was likely to have some gains in reduced pain and better function after 3-6 months of PT
- Ibuprofen 500 mg every 8-12 hours and prior to bedtime as needed for pain
- Dance for exercise, but any dances that cause pain should be avoided
- Review on the difference between pain and discomfort
- High cardiovascular risk: She was not interested in addressing her cardiometabolic risk at the time of the first visit.
Goals
- Pain-free near-normal physical functioning of L shoulder
- Dance, including tango, for recreation and physical activity
- Physical therapy focused on rotator cuff and scapular stabilizer strengthening, postural control, manual therapy, and education on pain avoidance
- Gentle dancing that avoids painful arm movements started, daily for 30 min
- Dancing and daily activities to be increased as tolerated (i.e., shoulder discomfort)
Exercise Program
- Physical therapy twice weekly
- Home exercises daily, as advised by therapist
- Dancing that does not cause pain allowed as tolerated
Follow-Up
- L shoulder OA
- Pain-avoidance techniques gave rapidly improved physical functioning of L upper extremity.
- Physical therapy made good progress over 3 months to near-normal physical functioning.
- Dance for aerobic exercise was very successful in getting her motivated.
- High cardiovascular risk
After 2 months of PT, she was motivated to work on weight management and diabetes prevention. She enrolled in a partial meal-replacement lifestyle intervention plan, lost 25 lb (11.3 kg) over the subsequent 3 months, and her fasting blood glucose/A1c returned to normal.
Senior Editor's Comment
This patient's story illustrates some of the art of exercise medicine, revealing the importance of working with patients to meet their emotional expectations and needs. Her primary care team was concerned about the diabetes and had been advising her about diet, weight loss, and taking metformin, but this was less important to the patient than the loss of her ability to dance. Dancing was the only type of physical exercise she enjoyed, so she needed to be able to dance as part of her pathway to improving insulin sensitivity. Close liaison with the physical therapist facilitated the process, because the therapist provided her with tips on how to avoid painful movements and begin to dance immediately. By accepting the need to dance as her top priority and then working to help overcome her barriers to dancing, the lifestyle intervention team gained her faith in them and she began to follow their advice on diet and weight. This approach seemed unusual to many who were involved in her care, as it appeared to put the diabetes problem on hold while focusing on a painful shoulder. But from another perspective, the painful shoulder was the most important problem to the patient and thus a significant barrier that needed to be overcome if exercise (in the form of dance) was to become her most important medicine.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
A Closer Look at Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons: There are thousands of chronic conditions and causes of disability.
Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons:
- There are thousands of chronic conditions and causes of disability.
- The vast majority of recommendations seem similar for most chronic conditions.
- Ultimately, exercise is fairly simple and needs to be seen as elegantly powerful.
- The complexities and nuances are matters of clinical judgment for safety's sake.
- The main concern in the chronic conditions in CDD4 is loss of independent living, which is primarily a function of light-intensity physical activities.
For these reasons, the Basic CDD4 Recommendations are consistent with but differ very slightly from the Guidelines and from the various physical activity guidelines discussed in the preceding section, because the CDD4 editors also want to make certain that sufficient attention is paid to light-intensity physical activity, especially the ability to perform instrumental activities of daily living with the goal of having patients remain independent. With these considerations in mind, the Basic CDD4 Recommendations are as follows:
- Every person with a chronic condition should be physically active, accumulating a minimum weekly total of
- 150 min of preferably moderate-intensity physical activity or, if that is too difficult, then
- 150 min of light-intensity physical activity may be substituted.
- At least 2 days per week of flexibility and muscle strengthening activities that should minimally involve
- chair sit-and-reach stretches on left and right,
- at least eight consecutive sit-to-stand exercises,
- at least 10 step-ups (or a flight of steps), leading with each foot, and
- at least eight consecutive arm curls with a minimum of 2 kg held in the hand; 4 kg is recommended.
- Individuals at risk for falls should be evaluated for causes of falls. Not all falls are caused by a condition that can be treated with exercise training. If the diagnosis of the causes suggests that exercise training can reduce the likelihood of a fall, then activities to improve balance should be incorporated into individuals' exercise regimens, under the supervision of an exercise therapist trained in fall prevention.
The higher the aerobic intensity, muscle forces, and required range of motion, the greater the likelihood of an adverse event.
These Basic CDD4 Recommendations are summarized in table 2.4. Readers should always bear in mind the goals behind the Basic CDD4 Recommendations, because these goals are helpful in drafting an individualized program to meet the unique needs of each patient. Everyone should be physically active to an extent sufficient to maintain independent living:

- Let no barrier block someone from doing light-intensity physical activity.
- Independent living requires a minimum ability to perform activities involving (or demanding)
- light-intensity aerobic work (or exertion), combined with
- strength, flexibility, and balance and coordination.
Adverse events from exercise cannot be completely eliminated, but there are two main categories to consider:
- Activity-dependent risks (due to the nature of the activity)
- Disease-dependent risks (those that relate to the pathophysiology)
The best way to minimize activity-dependent risks is to encourage the patient to practice safety precautions. If there is concern that the individual cannot do this independently, then he needs a supervised exercise program, at least to get started.
One major concern is whether or not the advice to do physical activity exposes the patient to the possibility of a disease-dependent risk. Such risks are associated with the intensity of exercise. Accordingly, if the recommendation is to complete vigorous- or high-intensity physical activities, it is prudent to follow the Guidelines on exercise testing and prescription. Most people with a chronic condition can safely participate in moderate-intensity physical activity, and if there is any concern that a particular individual cannot do so, she should either undergo some disease-specific diagnostic exercise testing or be referred to a supervised exercise program (or both).
There are few data beyond anecdotal cases to support the concern that light-intensity physical activities are likely to precipitate a disease-dependent adverse event (especially sudden death or myocardial infarction). Discerning the epidemiological role of light activities in precipitating such events would be exquisitely difficult, because participation in light-intensity activities is so ubiquitous in daily life. If someone is medically unstable to the point that activities of daily living threaten injury or death, then the Basic CDD4 Recommendations do not apply because the individual is not able to maintain independence and belongs in either a hospital or a nursing home. Indeed, it is likely that many people end up in a nursing facility sooner than they need to because no one recommended that they do light-intensity physical activity.
These nuances of safety are a key reason why an exercise professional is a necessary member of the chronic care team, because these staff are trained and have the experience to make good judgments regarding when exercise is safe and when it is not safe. See chapter 3 for a more in-depth discussion on how these judgments are made, which often involves more art than science.
Learn how to prescribe physical activity or exercise in chronic care in ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Permanent Pacemakers and Implantable Cardioverter-Defibrillators
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both.
Permanent Pacemakers
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both. In persons who have light-headedness, syncopal spells, shortness of breath, and more rarely chest pain or other cardiovascular symptoms owing to these problems, a permanent pacemaker
- improves symptoms,
- enhances exercise performance, and
- improves quality of life.
According to guidelines developed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS), class I indications for a permanent pacemaker include the following:
- Sinus node dysfunction
- Third-degree block and advanced second-degree AV block
- Hypersensitive carotid sinus syndrome
- Symptomatic bradycardia
- Sustained pause-dependent ventricular tachycardia
- Left ventricular systolic dysfunction and New York Heart Association (NYHA) functional class III or ambulatory class IV
A typical pacemaker system consists of two basic components: a pulse generator and either one or two pacing wires. In a traditional pacemaker the pacing wires are insulated and are implanted transvenously into the right atrium, right ventricle, or both. With a biventricular pacemaker, a lead is also placed in the left ventricle. The leads are connected to the pulse generator, which is typically implanted subcutaneously just below the clavicle. The two main functions of the leads are sensing and pacing. Sensing involves detecting electrical signals (i.e., P-waves and R-waves) from the heart. When these signals are not sensed at the proper timing, the pacemaker generator fires an impulse that causes the atria or ventricles (or both) to contract. Optimally, the pacing system uses an atrial and ventricular lead to maintain AV synchrony, which serves to optimize cardiac output at rest and during exercise.
Pacemakers are described by a standardized code. The first letter represents the chamber paced; the second is the chamber sensed; and the third denotes the response to a sensed event. The fourth position is used to indicate that the pacemaker has rate-response capabilities. For example, VVIR is the abbreviation used when the ventricle (V) is the chamber being paced and sensed. When the pacemaker senses a normal ventricular contraction, the pacemaker is inhibited (I). The "R" indicates that the pulse generator is rate-responsive during exercise. The response by the pacemaker is to either trigger or inhibit a pacing stimulus, depending on the absence or presence, respectively, of atrial or ventricular conduction, separately or in combination, relative to the range of heart rates that are programmed into the pacer.
A commonly used mode of pacing is the DDDR, which has dual-chamber (i.e., atrium and ventricle) pacing and inhibiting and has rate-response capability. The DDDR pacemaker is widely regarded as the optimal pacing mode in individuals who have normal sinoatrial (SA) node function, because it provides AV synchrony and uses the client's own sinus rhythm to guide ventricular stimulation. This results in a heart rate and cardiac output that, for the rest of the circulatory system, is very nearly normal.
Implantable Cardioverter-Defibrillators
An implantable cardioverter-defibrillator (ICD) is another electronic device that can be permanently implanted in individuals who either have a history of, or are at increased risk for, a life-threatening ventricular dysrhythmia. These devices impressively reduce mortality in persons with cardiomyopathy. Cardioverter-defibrillators can be just an ICD or can be a model that functions as both an ICD and a permanent pacemaker; like pacemakers, they are usually implanted subcutaneously just below the clavicle.
Implantable cardioverter-defibrillators electrically terminate life-threatening ventricular tachyarrhythmias. They consist of two basic parts: the lead system and the ICD itself. Implantable cardioverter-defibrillators have lead systems that are placed transvenously, typically by way of the subclavian vein. The ICD leads pick up the electrical rhythm of the heart and transmit this to the pulse generator, which senses the rhythm. Implantable cardioverter-defibrillators can detect atrial and ventricular arrhythmias, can provide antitachycardia pacing and defibrillation, and can be programmed with multiple protocols and the ability to record an electrocardiogram. Ventricular tachycardia (VT) and ventricular fibrillation (VF) are recognized by their rapid rates. If either VT or VF is sensed, the pulse generator delivers defibrillation or a synchronized cardioversion to terminate the rhythm. Other accelerated rhythms will initiate a pacing therapy intended to restore the rate within the preprogrammed limits.
According to guidelines developed jointly by the ACC, AHA, and HRS, class I indications for an ICD include the following:
- Survivor of cardiac arrest due to ventricular fibrillation (VF) or sustained ventricular tachycardia (VT)
- Structural heart disease with VT
- History of syncope of undetermined origin with clinically relevant VF or sustained VT induced during an electrophysiology study
- Left ventricular dysfunction due to myocardial infarction (post ≥40 days) with an ejection fraction (EF) ≤35% and NYHA class II or III or an EF ≤30% and NYHA class I
- Nonischemic dilated cardiomyopathy with an EF ≤35% and NYHA class II or III
- Nonsustained VT due to myocardial infarction with an EF ≤40% and VF or sustained VT induced during electrophysiology study
Combination Pacemaker - Defibrillator Devices
Some implantable devices are capable of providing both pacing and defibrillation. Recent evolution in terminology of pacemakers and defibrillators is toward calling them cardiac resynchronization therapy (CRT), with subclasses that provide pacing alone (CRT-P) and those that provide both pacing and defibrillation (CRT-D).
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Risk factors for coronary artery disease
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis.
Hypertension and Dyslipidemia
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis. When both conditions are present, the likelihood of having clinically significant CAD is drastically increased because atherosclerosis develops in areas of arteries that experience high blood pressure when high levels of low-density lipoprotein (LDL) are present. Because of this interrelationship and the role of exercise in mitigating these two conditions, hypertension and dyslipidemia are discussed here as linked CAD risk factors.
Basic Pathophysiology
The basic pathophysiology of these conditions is closely interrelated but is discussed separately to highlight key issues.
Hypertension
Hypertension (HTN) is a very common chronic condition, affecting about one in five people; it is defined as either
- systolic blood pressure (BP) over 139 mmHg or
- diastolic BP over 89 mmHg.
Table 6.1 has a more complete description of the classes of hypertension. High BP increases the risk for nonfatal and fatal cardiovascular disease, particularly CAD, kidney disease, and stroke. Even BP that is increased but not meeting the criteria for hypertension causes cardiovascular disease.
While hypertension is a common condition, the cause is not very well understood. In more than 95% of hypertension cases, the etiology is unknown and the condition is referred to as primary or essential or idiopathic hypertension. The remaining 5% of cases are secondary hypertension, so named because there is an identifiable underlying cause such as sleep apnea, drug-induced or drug-related causes (e.g., chronic corticosteroid therapy), chronic kidney disease, renovascular disease, aldosteronism, Cushing's syndrome, pheochromocytoma, coarctation of the aorta, and hyperthyroidism.
Dyslipidemia
Dyslipidemia - a high level of blood lipids - is a complex set of conditions, but the main concern is a high level of cholesterol. Cholesterol is critically important to every cell in the body, as a constituent of cell membranes that helps regulate their stability. Cholesterol is also an intermediary compound in steroid hormones, but the amount of cholesterol needed for hormones is many orders of magnitude lower than that needed for cell membranes. Cholesterol is synthesized and metabolized in the liver and then transported between the liver and the rest of the body. Cholesterol is not soluble in blood plasma and therefore has to be transported in the blood by lipoproteins. There are many different lipoproteins, each functioning to guide the cholesterol it carries to the proper metabolic pathway. This is the basic triad of lipoproteins:
- Very low-density lipoprotein (VLDL)
- Low-density lipoprotein (LDL)
- High-density lipoprotein (HDL)
The VLDL fraction carries about 80% triglycerides and 20% cholesterol, while the LDL and HDL mainly carry cholesterol. The total blood cholesterol is the sum of the cholesterol bound to VLDL, LDL, and HDL, and these cholesterol subcomponents are indicated with a -C suffix (e.g., LDL-C). Several subclassifications also exist, including two notable subclasses of LDL:
- Lipoprotein (a)
- Small dense LDL
Cholesterol metabolism is extremely complex, but the most important issue is that elevated total cholesterol and low-density lipoprotein cholesterol (LDL-C) are associated with an increased risk of CAD. Lipoprotein (a), or Lp(a), increases risk of CAD and of developing a thrombus, and small dense LDL also increases CAD risk. In contrast, high-density lipoprotein cholesterol (HDL-C) decreases CAD risk, through a cardioprotective effect that is partially related to this lipoprotein's role in the reverse cholesterol transport. In reverse transport, the cholesterol in HDL-C is transported to the liver where it is catabolized and excreted as bile.
Terms Often Used to Refer to Blood Lipids
- dyslipidemia - elevated triglycerides and cholesterol
- hypercholesterolemia - only cholesterol is elevated
- hypertriglyceridemia - only triglycerides are elevated
- exaggerated postprandial lipemia - prolonged elevation of triglycerides following consumption of dietary fat
- hyperlipoproteinemia or dyslipoproteinemia - high lipoprotein concentrations from genetic abnormalities or an underlying condition such as diabetes, renal disease, hypothyroidism, biliary obstruction, or dysproteinemia
Management and Medications
Medical management in persons who have the common chronic conditions often involves one or more medications for each condition, such that people with cardiometabolic conditions are often on five to eight prescription medicines. Again, this discussion treats these independently, but readers should expect to see multiple medications in persons in this group.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Case Study: Diabetes and Obesity with Osteoarthrosis
I intend to live into my 90s but I can’t get there unless I’m dancing. A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk.
Type 2 Diabetes and Obesity With Osteoarthrosis
Presenter: Geoffrey E. Moore, MD, FACSM
S
"I intend to live into my 90s but I can't get there unless I'm dancing."
A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk. Her recent A1c values had been 6.5-6.6, and her a.m. fasting glucose was recently 102. She qualified as T2DM by A1c criteria but wasn't working on her diet or weight and had refused to start taking metformin, and her primary care physician was increasingly concerned.
She expressed a desire to be more active through dance, which she had loved since childhood and felt was a part of her culture (having immigrated to the United States as a child). She expressed little concern about her weight and was more worried that the pain in her L shoulder kept her from dancing. She had first experienced the shoulder problem 10 years earlier while swimming backstroke. She had been to physical therapy (PT) twice, which made it worse. She also had received subacromial cortisone injections, but the relief didn't last. Her shoulder is worse at night (rolls over on her left side); the pain was rated 8/10 and was daily and constant except for sharp pain that radiated to the side of the neck when she moved the shoulder too much. She tried not to take pain or anti-inflammatory medications because she said they "wreck her stomach." Acupuncture (cupping) helped.
She also noted a history of her L knee "giving out," causing falls, and of having 2 knee arthroscopic surgeries (4 and 10 years earlier). When she overdoes weight-bearing activity, her left knee swells "like a watermelon." She did PT after the surgeries and gets to her normal daily activities but can't dance.
O
- Height: 5 ft 4¾ in. (1.65 m)
- Weight: 234.4 lb (106.3 kg)
- BMI: 39 kg/m2
- HR: 65 contractions/min
- BP: 188/98 mmHg
Pertinent Exam
- General: normal development, good nutrition, obese body habitus, no deformities
- CV: regular rhythm with normal S1 and S2, without rubs, gallops, or murmurs; distal pulses/circulation normal; no edema
- Musculoskeletal:
- Normal gait and station, muscular build especially of lower extremities
- Valgus alignment of both knees, no tenderness but the L knee has a small effusion
- Normal ROM without pain, substantial crepitus in both knees
- Left shoulder-specific tests:
- + Painful arc
- + Glenohumeral laxity, with crepitus
- + Neer test, +/- Hawkins test, +/- Speed's test
- + Painful with resisted external rotation, - pain with resisted internal rotation
- + AC joint tenderness
X Rays
- Osteoarthrosis in the acromioclavicular joint; severe osteoarthrosis in the glenohumeral joint with advanced sclerosis, subchondral cysts, and spurring; subluxed position of the humeral head at rest
Medications
- Coreg 10 mg once daily
- Diovan HCT 320/12.5 once daily
- Multivitamin once daily
A
- Increased CV risk: HTN, hyperlipidemia, diabetes by A1c criteria, sleep apnea, obesity
- Advanced glenohumeral osteoarthrosis and reduced function due to pain, status post - bilateral partial meniscectomies
Her shoulder markedly diminishes quality of life, impairing her ability to sleep and to recreate. Dance is her preferred form of physical activity, which she wants to do as her approach to improve the blood glucose and reduce her CV risk profile.
P
- L shoulder OA: refer to PT shoulder specialist
- It was explained that her shoulder would take a long time to get better, but she was likely to have some gains in reduced pain and better function after 3-6 months of PT
- Ibuprofen 500 mg every 8-12 hours and prior to bedtime as needed for pain
- Dance for exercise, but any dances that cause pain should be avoided
- Review on the difference between pain and discomfort
- High cardiovascular risk: She was not interested in addressing her cardiometabolic risk at the time of the first visit.
Goals
- Pain-free near-normal physical functioning of L shoulder
- Dance, including tango, for recreation and physical activity
- Physical therapy focused on rotator cuff and scapular stabilizer strengthening, postural control, manual therapy, and education on pain avoidance
- Gentle dancing that avoids painful arm movements started, daily for 30 min
- Dancing and daily activities to be increased as tolerated (i.e., shoulder discomfort)
Exercise Program
- Physical therapy twice weekly
- Home exercises daily, as advised by therapist
- Dancing that does not cause pain allowed as tolerated
Follow-Up
- L shoulder OA
- Pain-avoidance techniques gave rapidly improved physical functioning of L upper extremity.
- Physical therapy made good progress over 3 months to near-normal physical functioning.
- Dance for aerobic exercise was very successful in getting her motivated.
- High cardiovascular risk
After 2 months of PT, she was motivated to work on weight management and diabetes prevention. She enrolled in a partial meal-replacement lifestyle intervention plan, lost 25 lb (11.3 kg) over the subsequent 3 months, and her fasting blood glucose/A1c returned to normal.
Senior Editor's Comment
This patient's story illustrates some of the art of exercise medicine, revealing the importance of working with patients to meet their emotional expectations and needs. Her primary care team was concerned about the diabetes and had been advising her about diet, weight loss, and taking metformin, but this was less important to the patient than the loss of her ability to dance. Dancing was the only type of physical exercise she enjoyed, so she needed to be able to dance as part of her pathway to improving insulin sensitivity. Close liaison with the physical therapist facilitated the process, because the therapist provided her with tips on how to avoid painful movements and begin to dance immediately. By accepting the need to dance as her top priority and then working to help overcome her barriers to dancing, the lifestyle intervention team gained her faith in them and she began to follow their advice on diet and weight. This approach seemed unusual to many who were involved in her care, as it appeared to put the diabetes problem on hold while focusing on a painful shoulder. But from another perspective, the painful shoulder was the most important problem to the patient and thus a significant barrier that needed to be overcome if exercise (in the form of dance) was to become her most important medicine.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
A Closer Look at Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons: There are thousands of chronic conditions and causes of disability.
Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons:
- There are thousands of chronic conditions and causes of disability.
- The vast majority of recommendations seem similar for most chronic conditions.
- Ultimately, exercise is fairly simple and needs to be seen as elegantly powerful.
- The complexities and nuances are matters of clinical judgment for safety's sake.
- The main concern in the chronic conditions in CDD4 is loss of independent living, which is primarily a function of light-intensity physical activities.
For these reasons, the Basic CDD4 Recommendations are consistent with but differ very slightly from the Guidelines and from the various physical activity guidelines discussed in the preceding section, because the CDD4 editors also want to make certain that sufficient attention is paid to light-intensity physical activity, especially the ability to perform instrumental activities of daily living with the goal of having patients remain independent. With these considerations in mind, the Basic CDD4 Recommendations are as follows:
- Every person with a chronic condition should be physically active, accumulating a minimum weekly total of
- 150 min of preferably moderate-intensity physical activity or, if that is too difficult, then
- 150 min of light-intensity physical activity may be substituted.
- At least 2 days per week of flexibility and muscle strengthening activities that should minimally involve
- chair sit-and-reach stretches on left and right,
- at least eight consecutive sit-to-stand exercises,
- at least 10 step-ups (or a flight of steps), leading with each foot, and
- at least eight consecutive arm curls with a minimum of 2 kg held in the hand; 4 kg is recommended.
- Individuals at risk for falls should be evaluated for causes of falls. Not all falls are caused by a condition that can be treated with exercise training. If the diagnosis of the causes suggests that exercise training can reduce the likelihood of a fall, then activities to improve balance should be incorporated into individuals' exercise regimens, under the supervision of an exercise therapist trained in fall prevention.
The higher the aerobic intensity, muscle forces, and required range of motion, the greater the likelihood of an adverse event.
These Basic CDD4 Recommendations are summarized in table 2.4. Readers should always bear in mind the goals behind the Basic CDD4 Recommendations, because these goals are helpful in drafting an individualized program to meet the unique needs of each patient. Everyone should be physically active to an extent sufficient to maintain independent living:

- Let no barrier block someone from doing light-intensity physical activity.
- Independent living requires a minimum ability to perform activities involving (or demanding)
- light-intensity aerobic work (or exertion), combined with
- strength, flexibility, and balance and coordination.
Adverse events from exercise cannot be completely eliminated, but there are two main categories to consider:
- Activity-dependent risks (due to the nature of the activity)
- Disease-dependent risks (those that relate to the pathophysiology)
The best way to minimize activity-dependent risks is to encourage the patient to practice safety precautions. If there is concern that the individual cannot do this independently, then he needs a supervised exercise program, at least to get started.
One major concern is whether or not the advice to do physical activity exposes the patient to the possibility of a disease-dependent risk. Such risks are associated with the intensity of exercise. Accordingly, if the recommendation is to complete vigorous- or high-intensity physical activities, it is prudent to follow the Guidelines on exercise testing and prescription. Most people with a chronic condition can safely participate in moderate-intensity physical activity, and if there is any concern that a particular individual cannot do so, she should either undergo some disease-specific diagnostic exercise testing or be referred to a supervised exercise program (or both).
There are few data beyond anecdotal cases to support the concern that light-intensity physical activities are likely to precipitate a disease-dependent adverse event (especially sudden death or myocardial infarction). Discerning the epidemiological role of light activities in precipitating such events would be exquisitely difficult, because participation in light-intensity activities is so ubiquitous in daily life. If someone is medically unstable to the point that activities of daily living threaten injury or death, then the Basic CDD4 Recommendations do not apply because the individual is not able to maintain independence and belongs in either a hospital or a nursing home. Indeed, it is likely that many people end up in a nursing facility sooner than they need to because no one recommended that they do light-intensity physical activity.
These nuances of safety are a key reason why an exercise professional is a necessary member of the chronic care team, because these staff are trained and have the experience to make good judgments regarding when exercise is safe and when it is not safe. See chapter 3 for a more in-depth discussion on how these judgments are made, which often involves more art than science.
Learn how to prescribe physical activity or exercise in chronic care in ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Permanent Pacemakers and Implantable Cardioverter-Defibrillators
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both.
Permanent Pacemakers
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both. In persons who have light-headedness, syncopal spells, shortness of breath, and more rarely chest pain or other cardiovascular symptoms owing to these problems, a permanent pacemaker
- improves symptoms,
- enhances exercise performance, and
- improves quality of life.
According to guidelines developed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS), class I indications for a permanent pacemaker include the following:
- Sinus node dysfunction
- Third-degree block and advanced second-degree AV block
- Hypersensitive carotid sinus syndrome
- Symptomatic bradycardia
- Sustained pause-dependent ventricular tachycardia
- Left ventricular systolic dysfunction and New York Heart Association (NYHA) functional class III or ambulatory class IV
A typical pacemaker system consists of two basic components: a pulse generator and either one or two pacing wires. In a traditional pacemaker the pacing wires are insulated and are implanted transvenously into the right atrium, right ventricle, or both. With a biventricular pacemaker, a lead is also placed in the left ventricle. The leads are connected to the pulse generator, which is typically implanted subcutaneously just below the clavicle. The two main functions of the leads are sensing and pacing. Sensing involves detecting electrical signals (i.e., P-waves and R-waves) from the heart. When these signals are not sensed at the proper timing, the pacemaker generator fires an impulse that causes the atria or ventricles (or both) to contract. Optimally, the pacing system uses an atrial and ventricular lead to maintain AV synchrony, which serves to optimize cardiac output at rest and during exercise.
Pacemakers are described by a standardized code. The first letter represents the chamber paced; the second is the chamber sensed; and the third denotes the response to a sensed event. The fourth position is used to indicate that the pacemaker has rate-response capabilities. For example, VVIR is the abbreviation used when the ventricle (V) is the chamber being paced and sensed. When the pacemaker senses a normal ventricular contraction, the pacemaker is inhibited (I). The "R" indicates that the pulse generator is rate-responsive during exercise. The response by the pacemaker is to either trigger or inhibit a pacing stimulus, depending on the absence or presence, respectively, of atrial or ventricular conduction, separately or in combination, relative to the range of heart rates that are programmed into the pacer.
A commonly used mode of pacing is the DDDR, which has dual-chamber (i.e., atrium and ventricle) pacing and inhibiting and has rate-response capability. The DDDR pacemaker is widely regarded as the optimal pacing mode in individuals who have normal sinoatrial (SA) node function, because it provides AV synchrony and uses the client's own sinus rhythm to guide ventricular stimulation. This results in a heart rate and cardiac output that, for the rest of the circulatory system, is very nearly normal.
Implantable Cardioverter-Defibrillators
An implantable cardioverter-defibrillator (ICD) is another electronic device that can be permanently implanted in individuals who either have a history of, or are at increased risk for, a life-threatening ventricular dysrhythmia. These devices impressively reduce mortality in persons with cardiomyopathy. Cardioverter-defibrillators can be just an ICD or can be a model that functions as both an ICD and a permanent pacemaker; like pacemakers, they are usually implanted subcutaneously just below the clavicle.
Implantable cardioverter-defibrillators electrically terminate life-threatening ventricular tachyarrhythmias. They consist of two basic parts: the lead system and the ICD itself. Implantable cardioverter-defibrillators have lead systems that are placed transvenously, typically by way of the subclavian vein. The ICD leads pick up the electrical rhythm of the heart and transmit this to the pulse generator, which senses the rhythm. Implantable cardioverter-defibrillators can detect atrial and ventricular arrhythmias, can provide antitachycardia pacing and defibrillation, and can be programmed with multiple protocols and the ability to record an electrocardiogram. Ventricular tachycardia (VT) and ventricular fibrillation (VF) are recognized by their rapid rates. If either VT or VF is sensed, the pulse generator delivers defibrillation or a synchronized cardioversion to terminate the rhythm. Other accelerated rhythms will initiate a pacing therapy intended to restore the rate within the preprogrammed limits.
According to guidelines developed jointly by the ACC, AHA, and HRS, class I indications for an ICD include the following:
- Survivor of cardiac arrest due to ventricular fibrillation (VF) or sustained ventricular tachycardia (VT)
- Structural heart disease with VT
- History of syncope of undetermined origin with clinically relevant VF or sustained VT induced during an electrophysiology study
- Left ventricular dysfunction due to myocardial infarction (post ≥40 days) with an ejection fraction (EF) ≤35% and NYHA class II or III or an EF ≤30% and NYHA class I
- Nonischemic dilated cardiomyopathy with an EF ≤35% and NYHA class II or III
- Nonsustained VT due to myocardial infarction with an EF ≤40% and VF or sustained VT induced during electrophysiology study
Combination Pacemaker - Defibrillator Devices
Some implantable devices are capable of providing both pacing and defibrillation. Recent evolution in terminology of pacemakers and defibrillators is toward calling them cardiac resynchronization therapy (CRT), with subclasses that provide pacing alone (CRT-P) and those that provide both pacing and defibrillation (CRT-D).
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Risk factors for coronary artery disease
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis.
Hypertension and Dyslipidemia
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis. When both conditions are present, the likelihood of having clinically significant CAD is drastically increased because atherosclerosis develops in areas of arteries that experience high blood pressure when high levels of low-density lipoprotein (LDL) are present. Because of this interrelationship and the role of exercise in mitigating these two conditions, hypertension and dyslipidemia are discussed here as linked CAD risk factors.
Basic Pathophysiology
The basic pathophysiology of these conditions is closely interrelated but is discussed separately to highlight key issues.
Hypertension
Hypertension (HTN) is a very common chronic condition, affecting about one in five people; it is defined as either
- systolic blood pressure (BP) over 139 mmHg or
- diastolic BP over 89 mmHg.
Table 6.1 has a more complete description of the classes of hypertension. High BP increases the risk for nonfatal and fatal cardiovascular disease, particularly CAD, kidney disease, and stroke. Even BP that is increased but not meeting the criteria for hypertension causes cardiovascular disease.
While hypertension is a common condition, the cause is not very well understood. In more than 95% of hypertension cases, the etiology is unknown and the condition is referred to as primary or essential or idiopathic hypertension. The remaining 5% of cases are secondary hypertension, so named because there is an identifiable underlying cause such as sleep apnea, drug-induced or drug-related causes (e.g., chronic corticosteroid therapy), chronic kidney disease, renovascular disease, aldosteronism, Cushing's syndrome, pheochromocytoma, coarctation of the aorta, and hyperthyroidism.
Dyslipidemia
Dyslipidemia - a high level of blood lipids - is a complex set of conditions, but the main concern is a high level of cholesterol. Cholesterol is critically important to every cell in the body, as a constituent of cell membranes that helps regulate their stability. Cholesterol is also an intermediary compound in steroid hormones, but the amount of cholesterol needed for hormones is many orders of magnitude lower than that needed for cell membranes. Cholesterol is synthesized and metabolized in the liver and then transported between the liver and the rest of the body. Cholesterol is not soluble in blood plasma and therefore has to be transported in the blood by lipoproteins. There are many different lipoproteins, each functioning to guide the cholesterol it carries to the proper metabolic pathway. This is the basic triad of lipoproteins:
- Very low-density lipoprotein (VLDL)
- Low-density lipoprotein (LDL)
- High-density lipoprotein (HDL)
The VLDL fraction carries about 80% triglycerides and 20% cholesterol, while the LDL and HDL mainly carry cholesterol. The total blood cholesterol is the sum of the cholesterol bound to VLDL, LDL, and HDL, and these cholesterol subcomponents are indicated with a -C suffix (e.g., LDL-C). Several subclassifications also exist, including two notable subclasses of LDL:
- Lipoprotein (a)
- Small dense LDL
Cholesterol metabolism is extremely complex, but the most important issue is that elevated total cholesterol and low-density lipoprotein cholesterol (LDL-C) are associated with an increased risk of CAD. Lipoprotein (a), or Lp(a), increases risk of CAD and of developing a thrombus, and small dense LDL also increases CAD risk. In contrast, high-density lipoprotein cholesterol (HDL-C) decreases CAD risk, through a cardioprotective effect that is partially related to this lipoprotein's role in the reverse cholesterol transport. In reverse transport, the cholesterol in HDL-C is transported to the liver where it is catabolized and excreted as bile.
Terms Often Used to Refer to Blood Lipids
- dyslipidemia - elevated triglycerides and cholesterol
- hypercholesterolemia - only cholesterol is elevated
- hypertriglyceridemia - only triglycerides are elevated
- exaggerated postprandial lipemia - prolonged elevation of triglycerides following consumption of dietary fat
- hyperlipoproteinemia or dyslipoproteinemia - high lipoprotein concentrations from genetic abnormalities or an underlying condition such as diabetes, renal disease, hypothyroidism, biliary obstruction, or dysproteinemia
Management and Medications
Medical management in persons who have the common chronic conditions often involves one or more medications for each condition, such that people with cardiometabolic conditions are often on five to eight prescription medicines. Again, this discussion treats these independently, but readers should expect to see multiple medications in persons in this group.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Case Study: Diabetes and Obesity with Osteoarthrosis
I intend to live into my 90s but I can’t get there unless I’m dancing. A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk.
Type 2 Diabetes and Obesity With Osteoarthrosis
Presenter: Geoffrey E. Moore, MD, FACSM
S
"I intend to live into my 90s but I can't get there unless I'm dancing."
A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk. Her recent A1c values had been 6.5-6.6, and her a.m. fasting glucose was recently 102. She qualified as T2DM by A1c criteria but wasn't working on her diet or weight and had refused to start taking metformin, and her primary care physician was increasingly concerned.
She expressed a desire to be more active through dance, which she had loved since childhood and felt was a part of her culture (having immigrated to the United States as a child). She expressed little concern about her weight and was more worried that the pain in her L shoulder kept her from dancing. She had first experienced the shoulder problem 10 years earlier while swimming backstroke. She had been to physical therapy (PT) twice, which made it worse. She also had received subacromial cortisone injections, but the relief didn't last. Her shoulder is worse at night (rolls over on her left side); the pain was rated 8/10 and was daily and constant except for sharp pain that radiated to the side of the neck when she moved the shoulder too much. She tried not to take pain or anti-inflammatory medications because she said they "wreck her stomach." Acupuncture (cupping) helped.
She also noted a history of her L knee "giving out," causing falls, and of having 2 knee arthroscopic surgeries (4 and 10 years earlier). When she overdoes weight-bearing activity, her left knee swells "like a watermelon." She did PT after the surgeries and gets to her normal daily activities but can't dance.
O
- Height: 5 ft 4¾ in. (1.65 m)
- Weight: 234.4 lb (106.3 kg)
- BMI: 39 kg/m2
- HR: 65 contractions/min
- BP: 188/98 mmHg
Pertinent Exam
- General: normal development, good nutrition, obese body habitus, no deformities
- CV: regular rhythm with normal S1 and S2, without rubs, gallops, or murmurs; distal pulses/circulation normal; no edema
- Musculoskeletal:
- Normal gait and station, muscular build especially of lower extremities
- Valgus alignment of both knees, no tenderness but the L knee has a small effusion
- Normal ROM without pain, substantial crepitus in both knees
- Left shoulder-specific tests:
- + Painful arc
- + Glenohumeral laxity, with crepitus
- + Neer test, +/- Hawkins test, +/- Speed's test
- + Painful with resisted external rotation, - pain with resisted internal rotation
- + AC joint tenderness
X Rays
- Osteoarthrosis in the acromioclavicular joint; severe osteoarthrosis in the glenohumeral joint with advanced sclerosis, subchondral cysts, and spurring; subluxed position of the humeral head at rest
Medications
- Coreg 10 mg once daily
- Diovan HCT 320/12.5 once daily
- Multivitamin once daily
A
- Increased CV risk: HTN, hyperlipidemia, diabetes by A1c criteria, sleep apnea, obesity
- Advanced glenohumeral osteoarthrosis and reduced function due to pain, status post - bilateral partial meniscectomies
Her shoulder markedly diminishes quality of life, impairing her ability to sleep and to recreate. Dance is her preferred form of physical activity, which she wants to do as her approach to improve the blood glucose and reduce her CV risk profile.
P
- L shoulder OA: refer to PT shoulder specialist
- It was explained that her shoulder would take a long time to get better, but she was likely to have some gains in reduced pain and better function after 3-6 months of PT
- Ibuprofen 500 mg every 8-12 hours and prior to bedtime as needed for pain
- Dance for exercise, but any dances that cause pain should be avoided
- Review on the difference between pain and discomfort
- High cardiovascular risk: She was not interested in addressing her cardiometabolic risk at the time of the first visit.
Goals
- Pain-free near-normal physical functioning of L shoulder
- Dance, including tango, for recreation and physical activity
- Physical therapy focused on rotator cuff and scapular stabilizer strengthening, postural control, manual therapy, and education on pain avoidance
- Gentle dancing that avoids painful arm movements started, daily for 30 min
- Dancing and daily activities to be increased as tolerated (i.e., shoulder discomfort)
Exercise Program
- Physical therapy twice weekly
- Home exercises daily, as advised by therapist
- Dancing that does not cause pain allowed as tolerated
Follow-Up
- L shoulder OA
- Pain-avoidance techniques gave rapidly improved physical functioning of L upper extremity.
- Physical therapy made good progress over 3 months to near-normal physical functioning.
- Dance for aerobic exercise was very successful in getting her motivated.
- High cardiovascular risk
After 2 months of PT, she was motivated to work on weight management and diabetes prevention. She enrolled in a partial meal-replacement lifestyle intervention plan, lost 25 lb (11.3 kg) over the subsequent 3 months, and her fasting blood glucose/A1c returned to normal.
Senior Editor's Comment
This patient's story illustrates some of the art of exercise medicine, revealing the importance of working with patients to meet their emotional expectations and needs. Her primary care team was concerned about the diabetes and had been advising her about diet, weight loss, and taking metformin, but this was less important to the patient than the loss of her ability to dance. Dancing was the only type of physical exercise she enjoyed, so she needed to be able to dance as part of her pathway to improving insulin sensitivity. Close liaison with the physical therapist facilitated the process, because the therapist provided her with tips on how to avoid painful movements and begin to dance immediately. By accepting the need to dance as her top priority and then working to help overcome her barriers to dancing, the lifestyle intervention team gained her faith in them and she began to follow their advice on diet and weight. This approach seemed unusual to many who were involved in her care, as it appeared to put the diabetes problem on hold while focusing on a painful shoulder. But from another perspective, the painful shoulder was the most important problem to the patient and thus a significant barrier that needed to be overcome if exercise (in the form of dance) was to become her most important medicine.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
A Closer Look at Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons: There are thousands of chronic conditions and causes of disability.
Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons:
- There are thousands of chronic conditions and causes of disability.
- The vast majority of recommendations seem similar for most chronic conditions.
- Ultimately, exercise is fairly simple and needs to be seen as elegantly powerful.
- The complexities and nuances are matters of clinical judgment for safety's sake.
- The main concern in the chronic conditions in CDD4 is loss of independent living, which is primarily a function of light-intensity physical activities.
For these reasons, the Basic CDD4 Recommendations are consistent with but differ very slightly from the Guidelines and from the various physical activity guidelines discussed in the preceding section, because the CDD4 editors also want to make certain that sufficient attention is paid to light-intensity physical activity, especially the ability to perform instrumental activities of daily living with the goal of having patients remain independent. With these considerations in mind, the Basic CDD4 Recommendations are as follows:
- Every person with a chronic condition should be physically active, accumulating a minimum weekly total of
- 150 min of preferably moderate-intensity physical activity or, if that is too difficult, then
- 150 min of light-intensity physical activity may be substituted.
- At least 2 days per week of flexibility and muscle strengthening activities that should minimally involve
- chair sit-and-reach stretches on left and right,
- at least eight consecutive sit-to-stand exercises,
- at least 10 step-ups (or a flight of steps), leading with each foot, and
- at least eight consecutive arm curls with a minimum of 2 kg held in the hand; 4 kg is recommended.
- Individuals at risk for falls should be evaluated for causes of falls. Not all falls are caused by a condition that can be treated with exercise training. If the diagnosis of the causes suggests that exercise training can reduce the likelihood of a fall, then activities to improve balance should be incorporated into individuals' exercise regimens, under the supervision of an exercise therapist trained in fall prevention.
The higher the aerobic intensity, muscle forces, and required range of motion, the greater the likelihood of an adverse event.
These Basic CDD4 Recommendations are summarized in table 2.4. Readers should always bear in mind the goals behind the Basic CDD4 Recommendations, because these goals are helpful in drafting an individualized program to meet the unique needs of each patient. Everyone should be physically active to an extent sufficient to maintain independent living:

- Let no barrier block someone from doing light-intensity physical activity.
- Independent living requires a minimum ability to perform activities involving (or demanding)
- light-intensity aerobic work (or exertion), combined with
- strength, flexibility, and balance and coordination.
Adverse events from exercise cannot be completely eliminated, but there are two main categories to consider:
- Activity-dependent risks (due to the nature of the activity)
- Disease-dependent risks (those that relate to the pathophysiology)
The best way to minimize activity-dependent risks is to encourage the patient to practice safety precautions. If there is concern that the individual cannot do this independently, then he needs a supervised exercise program, at least to get started.
One major concern is whether or not the advice to do physical activity exposes the patient to the possibility of a disease-dependent risk. Such risks are associated with the intensity of exercise. Accordingly, if the recommendation is to complete vigorous- or high-intensity physical activities, it is prudent to follow the Guidelines on exercise testing and prescription. Most people with a chronic condition can safely participate in moderate-intensity physical activity, and if there is any concern that a particular individual cannot do so, she should either undergo some disease-specific diagnostic exercise testing or be referred to a supervised exercise program (or both).
There are few data beyond anecdotal cases to support the concern that light-intensity physical activities are likely to precipitate a disease-dependent adverse event (especially sudden death or myocardial infarction). Discerning the epidemiological role of light activities in precipitating such events would be exquisitely difficult, because participation in light-intensity activities is so ubiquitous in daily life. If someone is medically unstable to the point that activities of daily living threaten injury or death, then the Basic CDD4 Recommendations do not apply because the individual is not able to maintain independence and belongs in either a hospital or a nursing home. Indeed, it is likely that many people end up in a nursing facility sooner than they need to because no one recommended that they do light-intensity physical activity.
These nuances of safety are a key reason why an exercise professional is a necessary member of the chronic care team, because these staff are trained and have the experience to make good judgments regarding when exercise is safe and when it is not safe. See chapter 3 for a more in-depth discussion on how these judgments are made, which often involves more art than science.
Learn how to prescribe physical activity or exercise in chronic care in ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Permanent Pacemakers and Implantable Cardioverter-Defibrillators
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both.
Permanent Pacemakers
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both. In persons who have light-headedness, syncopal spells, shortness of breath, and more rarely chest pain or other cardiovascular symptoms owing to these problems, a permanent pacemaker
- improves symptoms,
- enhances exercise performance, and
- improves quality of life.
According to guidelines developed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS), class I indications for a permanent pacemaker include the following:
- Sinus node dysfunction
- Third-degree block and advanced second-degree AV block
- Hypersensitive carotid sinus syndrome
- Symptomatic bradycardia
- Sustained pause-dependent ventricular tachycardia
- Left ventricular systolic dysfunction and New York Heart Association (NYHA) functional class III or ambulatory class IV
A typical pacemaker system consists of two basic components: a pulse generator and either one or two pacing wires. In a traditional pacemaker the pacing wires are insulated and are implanted transvenously into the right atrium, right ventricle, or both. With a biventricular pacemaker, a lead is also placed in the left ventricle. The leads are connected to the pulse generator, which is typically implanted subcutaneously just below the clavicle. The two main functions of the leads are sensing and pacing. Sensing involves detecting electrical signals (i.e., P-waves and R-waves) from the heart. When these signals are not sensed at the proper timing, the pacemaker generator fires an impulse that causes the atria or ventricles (or both) to contract. Optimally, the pacing system uses an atrial and ventricular lead to maintain AV synchrony, which serves to optimize cardiac output at rest and during exercise.
Pacemakers are described by a standardized code. The first letter represents the chamber paced; the second is the chamber sensed; and the third denotes the response to a sensed event. The fourth position is used to indicate that the pacemaker has rate-response capabilities. For example, VVIR is the abbreviation used when the ventricle (V) is the chamber being paced and sensed. When the pacemaker senses a normal ventricular contraction, the pacemaker is inhibited (I). The "R" indicates that the pulse generator is rate-responsive during exercise. The response by the pacemaker is to either trigger or inhibit a pacing stimulus, depending on the absence or presence, respectively, of atrial or ventricular conduction, separately or in combination, relative to the range of heart rates that are programmed into the pacer.
A commonly used mode of pacing is the DDDR, which has dual-chamber (i.e., atrium and ventricle) pacing and inhibiting and has rate-response capability. The DDDR pacemaker is widely regarded as the optimal pacing mode in individuals who have normal sinoatrial (SA) node function, because it provides AV synchrony and uses the client's own sinus rhythm to guide ventricular stimulation. This results in a heart rate and cardiac output that, for the rest of the circulatory system, is very nearly normal.
Implantable Cardioverter-Defibrillators
An implantable cardioverter-defibrillator (ICD) is another electronic device that can be permanently implanted in individuals who either have a history of, or are at increased risk for, a life-threatening ventricular dysrhythmia. These devices impressively reduce mortality in persons with cardiomyopathy. Cardioverter-defibrillators can be just an ICD or can be a model that functions as both an ICD and a permanent pacemaker; like pacemakers, they are usually implanted subcutaneously just below the clavicle.
Implantable cardioverter-defibrillators electrically terminate life-threatening ventricular tachyarrhythmias. They consist of two basic parts: the lead system and the ICD itself. Implantable cardioverter-defibrillators have lead systems that are placed transvenously, typically by way of the subclavian vein. The ICD leads pick up the electrical rhythm of the heart and transmit this to the pulse generator, which senses the rhythm. Implantable cardioverter-defibrillators can detect atrial and ventricular arrhythmias, can provide antitachycardia pacing and defibrillation, and can be programmed with multiple protocols and the ability to record an electrocardiogram. Ventricular tachycardia (VT) and ventricular fibrillation (VF) are recognized by their rapid rates. If either VT or VF is sensed, the pulse generator delivers defibrillation or a synchronized cardioversion to terminate the rhythm. Other accelerated rhythms will initiate a pacing therapy intended to restore the rate within the preprogrammed limits.
According to guidelines developed jointly by the ACC, AHA, and HRS, class I indications for an ICD include the following:
- Survivor of cardiac arrest due to ventricular fibrillation (VF) or sustained ventricular tachycardia (VT)
- Structural heart disease with VT
- History of syncope of undetermined origin with clinically relevant VF or sustained VT induced during an electrophysiology study
- Left ventricular dysfunction due to myocardial infarction (post ≥40 days) with an ejection fraction (EF) ≤35% and NYHA class II or III or an EF ≤30% and NYHA class I
- Nonischemic dilated cardiomyopathy with an EF ≤35% and NYHA class II or III
- Nonsustained VT due to myocardial infarction with an EF ≤40% and VF or sustained VT induced during electrophysiology study
Combination Pacemaker - Defibrillator Devices
Some implantable devices are capable of providing both pacing and defibrillation. Recent evolution in terminology of pacemakers and defibrillators is toward calling them cardiac resynchronization therapy (CRT), with subclasses that provide pacing alone (CRT-P) and those that provide both pacing and defibrillation (CRT-D).
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Risk factors for coronary artery disease
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis.
Hypertension and Dyslipidemia
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis. When both conditions are present, the likelihood of having clinically significant CAD is drastically increased because atherosclerosis develops in areas of arteries that experience high blood pressure when high levels of low-density lipoprotein (LDL) are present. Because of this interrelationship and the role of exercise in mitigating these two conditions, hypertension and dyslipidemia are discussed here as linked CAD risk factors.
Basic Pathophysiology
The basic pathophysiology of these conditions is closely interrelated but is discussed separately to highlight key issues.
Hypertension
Hypertension (HTN) is a very common chronic condition, affecting about one in five people; it is defined as either
- systolic blood pressure (BP) over 139 mmHg or
- diastolic BP over 89 mmHg.
Table 6.1 has a more complete description of the classes of hypertension. High BP increases the risk for nonfatal and fatal cardiovascular disease, particularly CAD, kidney disease, and stroke. Even BP that is increased but not meeting the criteria for hypertension causes cardiovascular disease.
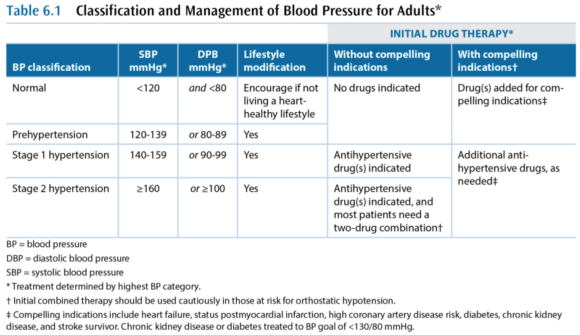
While hypertension is a common condition, the cause is not very well understood. In more than 95% of hypertension cases, the etiology is unknown and the condition is referred to as primary or essential or idiopathic hypertension. The remaining 5% of cases are secondary hypertension, so named because there is an identifiable underlying cause such as sleep apnea, drug-induced or drug-related causes (e.g., chronic corticosteroid therapy), chronic kidney disease, renovascular disease, aldosteronism, Cushing's syndrome, pheochromocytoma, coarctation of the aorta, and hyperthyroidism.
Dyslipidemia
Dyslipidemia - a high level of blood lipids - is a complex set of conditions, but the main concern is a high level of cholesterol. Cholesterol is critically important to every cell in the body, as a constituent of cell membranes that helps regulate their stability. Cholesterol is also an intermediary compound in steroid hormones, but the amount of cholesterol needed for hormones is many orders of magnitude lower than that needed for cell membranes. Cholesterol is synthesized and metabolized in the liver and then transported between the liver and the rest of the body. Cholesterol is not soluble in blood plasma and therefore has to be transported in the blood by lipoproteins. There are many different lipoproteins, each functioning to guide the cholesterol it carries to the proper metabolic pathway. This is the basic triad of lipoproteins:
- Very low-density lipoprotein (VLDL)
- Low-density lipoprotein (LDL)
- High-density lipoprotein (HDL)
The VLDL fraction carries about 80% triglycerides and 20% cholesterol, while the LDL and HDL mainly carry cholesterol. The total blood cholesterol is the sum of the cholesterol bound to VLDL, LDL, and HDL, and these cholesterol subcomponents are indicated with a -C suffix (e.g., LDL-C). Several subclassifications also exist, including two notable subclasses of LDL:
- Lipoprotein (a)
- Small dense LDL
Cholesterol metabolism is extremely complex, but the most important issue is that elevated total cholesterol and low-density lipoprotein cholesterol (LDL-C) are associated with an increased risk of CAD. Lipoprotein (a), or Lp(a), increases risk of CAD and of developing a thrombus, and small dense LDL also increases CAD risk. In contrast, high-density lipoprotein cholesterol (HDL-C) decreases CAD risk, through a cardioprotective effect that is partially related to this lipoprotein's role in the reverse cholesterol transport. In reverse transport, the cholesterol in HDL-C is transported to the liver where it is catabolized and excreted as bile.
Terms Often Used to Refer to Blood Lipids
- dyslipidemia - elevated triglycerides and cholesterol
- hypercholesterolemia - only cholesterol is elevated
- hypertriglyceridemia - only triglycerides are elevated
- exaggerated postprandial lipemia - prolonged elevation of triglycerides following consumption of dietary fat
- hyperlipoproteinemia or dyslipoproteinemia - high lipoprotein concentrations from genetic abnormalities or an underlying condition such as diabetes, renal disease, hypothyroidism, biliary obstruction, or dysproteinemia
Management and Medications
Medical management in persons who have the common chronic conditions often involves one or more medications for each condition, such that people with cardiometabolic conditions are often on five to eight prescription medicines. Again, this discussion treats these independently, but readers should expect to see multiple medications in persons in this group.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Case Study: Diabetes and Obesity with Osteoarthrosis
I intend to live into my 90s but I can’t get there unless I’m dancing. A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk.
Type 2 Diabetes and Obesity With Osteoarthrosis
Presenter: Geoffrey E. Moore, MD, FACSM
S
"I intend to live into my 90s but I can't get there unless I'm dancing."
A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk. Her recent A1c values had been 6.5-6.6, and her a.m. fasting glucose was recently 102. She qualified as T2DM by A1c criteria but wasn't working on her diet or weight and had refused to start taking metformin, and her primary care physician was increasingly concerned.
She expressed a desire to be more active through dance, which she had loved since childhood and felt was a part of her culture (having immigrated to the United States as a child). She expressed little concern about her weight and was more worried that the pain in her L shoulder kept her from dancing. She had first experienced the shoulder problem 10 years earlier while swimming backstroke. She had been to physical therapy (PT) twice, which made it worse. She also had received subacromial cortisone injections, but the relief didn't last. Her shoulder is worse at night (rolls over on her left side); the pain was rated 8/10 and was daily and constant except for sharp pain that radiated to the side of the neck when she moved the shoulder too much. She tried not to take pain or anti-inflammatory medications because she said they "wreck her stomach." Acupuncture (cupping) helped.
She also noted a history of her L knee "giving out," causing falls, and of having 2 knee arthroscopic surgeries (4 and 10 years earlier). When she overdoes weight-bearing activity, her left knee swells "like a watermelon." She did PT after the surgeries and gets to her normal daily activities but can't dance.
O
- Height: 5 ft 4¾ in. (1.65 m)
- Weight: 234.4 lb (106.3 kg)
- BMI: 39 kg/m2
- HR: 65 contractions/min
- BP: 188/98 mmHg
Pertinent Exam
- General: normal development, good nutrition, obese body habitus, no deformities
- CV: regular rhythm with normal S1 and S2, without rubs, gallops, or murmurs; distal pulses/circulation normal; no edema
- Musculoskeletal:
- Normal gait and station, muscular build especially of lower extremities
- Valgus alignment of both knees, no tenderness but the L knee has a small effusion
- Normal ROM without pain, substantial crepitus in both knees
- Left shoulder-specific tests:
- + Painful arc
- + Glenohumeral laxity, with crepitus
- + Neer test, +/- Hawkins test, +/- Speed's test
- + Painful with resisted external rotation, - pain with resisted internal rotation
- + AC joint tenderness
X Rays
- Osteoarthrosis in the acromioclavicular joint; severe osteoarthrosis in the glenohumeral joint with advanced sclerosis, subchondral cysts, and spurring; subluxed position of the humeral head at rest
Medications
- Coreg 10 mg once daily
- Diovan HCT 320/12.5 once daily
- Multivitamin once daily
A
- Increased CV risk: HTN, hyperlipidemia, diabetes by A1c criteria, sleep apnea, obesity
- Advanced glenohumeral osteoarthrosis and reduced function due to pain, status post - bilateral partial meniscectomies
Her shoulder markedly diminishes quality of life, impairing her ability to sleep and to recreate. Dance is her preferred form of physical activity, which she wants to do as her approach to improve the blood glucose and reduce her CV risk profile.
P
- L shoulder OA: refer to PT shoulder specialist
- It was explained that her shoulder would take a long time to get better, but she was likely to have some gains in reduced pain and better function after 3-6 months of PT
- Ibuprofen 500 mg every 8-12 hours and prior to bedtime as needed for pain
- Dance for exercise, but any dances that cause pain should be avoided
- Review on the difference between pain and discomfort
- High cardiovascular risk: She was not interested in addressing her cardiometabolic risk at the time of the first visit.
Goals
- Pain-free near-normal physical functioning of L shoulder
- Dance, including tango, for recreation and physical activity
- Physical therapy focused on rotator cuff and scapular stabilizer strengthening, postural control, manual therapy, and education on pain avoidance
- Gentle dancing that avoids painful arm movements started, daily for 30 min
- Dancing and daily activities to be increased as tolerated (i.e., shoulder discomfort)
Exercise Program
- Physical therapy twice weekly
- Home exercises daily, as advised by therapist
- Dancing that does not cause pain allowed as tolerated
Follow-Up
- L shoulder OA
- Pain-avoidance techniques gave rapidly improved physical functioning of L upper extremity.
- Physical therapy made good progress over 3 months to near-normal physical functioning.
- Dance for aerobic exercise was very successful in getting her motivated.
- High cardiovascular risk
After 2 months of PT, she was motivated to work on weight management and diabetes prevention. She enrolled in a partial meal-replacement lifestyle intervention plan, lost 25 lb (11.3 kg) over the subsequent 3 months, and her fasting blood glucose/A1c returned to normal.
Senior Editor's Comment
This patient's story illustrates some of the art of exercise medicine, revealing the importance of working with patients to meet their emotional expectations and needs. Her primary care team was concerned about the diabetes and had been advising her about diet, weight loss, and taking metformin, but this was less important to the patient than the loss of her ability to dance. Dancing was the only type of physical exercise she enjoyed, so she needed to be able to dance as part of her pathway to improving insulin sensitivity. Close liaison with the physical therapist facilitated the process, because the therapist provided her with tips on how to avoid painful movements and begin to dance immediately. By accepting the need to dance as her top priority and then working to help overcome her barriers to dancing, the lifestyle intervention team gained her faith in them and she began to follow their advice on diet and weight. This approach seemed unusual to many who were involved in her care, as it appeared to put the diabetes problem on hold while focusing on a painful shoulder. But from another perspective, the painful shoulder was the most important problem to the patient and thus a significant barrier that needed to be overcome if exercise (in the form of dance) was to become her most important medicine.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
A Closer Look at Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons: There are thousands of chronic conditions and causes of disability.
Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons:
- There are thousands of chronic conditions and causes of disability.
- The vast majority of recommendations seem similar for most chronic conditions.
- Ultimately, exercise is fairly simple and needs to be seen as elegantly powerful.
- The complexities and nuances are matters of clinical judgment for safety's sake.
- The main concern in the chronic conditions in CDD4 is loss of independent living, which is primarily a function of light-intensity physical activities.
For these reasons, the Basic CDD4 Recommendations are consistent with but differ very slightly from the Guidelines and from the various physical activity guidelines discussed in the preceding section, because the CDD4 editors also want to make certain that sufficient attention is paid to light-intensity physical activity, especially the ability to perform instrumental activities of daily living with the goal of having patients remain independent. With these considerations in mind, the Basic CDD4 Recommendations are as follows:
- Every person with a chronic condition should be physically active, accumulating a minimum weekly total of
- 150 min of preferably moderate-intensity physical activity or, if that is too difficult, then
- 150 min of light-intensity physical activity may be substituted.
- At least 2 days per week of flexibility and muscle strengthening activities that should minimally involve
- chair sit-and-reach stretches on left and right,
- at least eight consecutive sit-to-stand exercises,
- at least 10 step-ups (or a flight of steps), leading with each foot, and
- at least eight consecutive arm curls with a minimum of 2 kg held in the hand; 4 kg is recommended.
- Individuals at risk for falls should be evaluated for causes of falls. Not all falls are caused by a condition that can be treated with exercise training. If the diagnosis of the causes suggests that exercise training can reduce the likelihood of a fall, then activities to improve balance should be incorporated into individuals' exercise regimens, under the supervision of an exercise therapist trained in fall prevention.
The higher the aerobic intensity, muscle forces, and required range of motion, the greater the likelihood of an adverse event.
These Basic CDD4 Recommendations are summarized in table 2.4. Readers should always bear in mind the goals behind the Basic CDD4 Recommendations, because these goals are helpful in drafting an individualized program to meet the unique needs of each patient. Everyone should be physically active to an extent sufficient to maintain independent living:

- Let no barrier block someone from doing light-intensity physical activity.
- Independent living requires a minimum ability to perform activities involving (or demanding)
- light-intensity aerobic work (or exertion), combined with
- strength, flexibility, and balance and coordination.
Adverse events from exercise cannot be completely eliminated, but there are two main categories to consider:
- Activity-dependent risks (due to the nature of the activity)
- Disease-dependent risks (those that relate to the pathophysiology)
The best way to minimize activity-dependent risks is to encourage the patient to practice safety precautions. If there is concern that the individual cannot do this independently, then he needs a supervised exercise program, at least to get started.
One major concern is whether or not the advice to do physical activity exposes the patient to the possibility of a disease-dependent risk. Such risks are associated with the intensity of exercise. Accordingly, if the recommendation is to complete vigorous- or high-intensity physical activities, it is prudent to follow the Guidelines on exercise testing and prescription. Most people with a chronic condition can safely participate in moderate-intensity physical activity, and if there is any concern that a particular individual cannot do so, she should either undergo some disease-specific diagnostic exercise testing or be referred to a supervised exercise program (or both).
There are few data beyond anecdotal cases to support the concern that light-intensity physical activities are likely to precipitate a disease-dependent adverse event (especially sudden death or myocardial infarction). Discerning the epidemiological role of light activities in precipitating such events would be exquisitely difficult, because participation in light-intensity activities is so ubiquitous in daily life. If someone is medically unstable to the point that activities of daily living threaten injury or death, then the Basic CDD4 Recommendations do not apply because the individual is not able to maintain independence and belongs in either a hospital or a nursing home. Indeed, it is likely that many people end up in a nursing facility sooner than they need to because no one recommended that they do light-intensity physical activity.
These nuances of safety are a key reason why an exercise professional is a necessary member of the chronic care team, because these staff are trained and have the experience to make good judgments regarding when exercise is safe and when it is not safe. See chapter 3 for a more in-depth discussion on how these judgments are made, which often involves more art than science.
Learn how to prescribe physical activity or exercise in chronic care in ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Permanent Pacemakers and Implantable Cardioverter-Defibrillators
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both.
Permanent Pacemakers
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both. In persons who have light-headedness, syncopal spells, shortness of breath, and more rarely chest pain or other cardiovascular symptoms owing to these problems, a permanent pacemaker
- improves symptoms,
- enhances exercise performance, and
- improves quality of life.
According to guidelines developed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS), class I indications for a permanent pacemaker include the following:
- Sinus node dysfunction
- Third-degree block and advanced second-degree AV block
- Hypersensitive carotid sinus syndrome
- Symptomatic bradycardia
- Sustained pause-dependent ventricular tachycardia
- Left ventricular systolic dysfunction and New York Heart Association (NYHA) functional class III or ambulatory class IV
A typical pacemaker system consists of two basic components: a pulse generator and either one or two pacing wires. In a traditional pacemaker the pacing wires are insulated and are implanted transvenously into the right atrium, right ventricle, or both. With a biventricular pacemaker, a lead is also placed in the left ventricle. The leads are connected to the pulse generator, which is typically implanted subcutaneously just below the clavicle. The two main functions of the leads are sensing and pacing. Sensing involves detecting electrical signals (i.e., P-waves and R-waves) from the heart. When these signals are not sensed at the proper timing, the pacemaker generator fires an impulse that causes the atria or ventricles (or both) to contract. Optimally, the pacing system uses an atrial and ventricular lead to maintain AV synchrony, which serves to optimize cardiac output at rest and during exercise.
Pacemakers are described by a standardized code. The first letter represents the chamber paced; the second is the chamber sensed; and the third denotes the response to a sensed event. The fourth position is used to indicate that the pacemaker has rate-response capabilities. For example, VVIR is the abbreviation used when the ventricle (V) is the chamber being paced and sensed. When the pacemaker senses a normal ventricular contraction, the pacemaker is inhibited (I). The "R" indicates that the pulse generator is rate-responsive during exercise. The response by the pacemaker is to either trigger or inhibit a pacing stimulus, depending on the absence or presence, respectively, of atrial or ventricular conduction, separately or in combination, relative to the range of heart rates that are programmed into the pacer.
A commonly used mode of pacing is the DDDR, which has dual-chamber (i.e., atrium and ventricle) pacing and inhibiting and has rate-response capability. The DDDR pacemaker is widely regarded as the optimal pacing mode in individuals who have normal sinoatrial (SA) node function, because it provides AV synchrony and uses the client's own sinus rhythm to guide ventricular stimulation. This results in a heart rate and cardiac output that, for the rest of the circulatory system, is very nearly normal.
Implantable Cardioverter-Defibrillators
An implantable cardioverter-defibrillator (ICD) is another electronic device that can be permanently implanted in individuals who either have a history of, or are at increased risk for, a life-threatening ventricular dysrhythmia. These devices impressively reduce mortality in persons with cardiomyopathy. Cardioverter-defibrillators can be just an ICD or can be a model that functions as both an ICD and a permanent pacemaker; like pacemakers, they are usually implanted subcutaneously just below the clavicle.
Implantable cardioverter-defibrillators electrically terminate life-threatening ventricular tachyarrhythmias. They consist of two basic parts: the lead system and the ICD itself. Implantable cardioverter-defibrillators have lead systems that are placed transvenously, typically by way of the subclavian vein. The ICD leads pick up the electrical rhythm of the heart and transmit this to the pulse generator, which senses the rhythm. Implantable cardioverter-defibrillators can detect atrial and ventricular arrhythmias, can provide antitachycardia pacing and defibrillation, and can be programmed with multiple protocols and the ability to record an electrocardiogram. Ventricular tachycardia (VT) and ventricular fibrillation (VF) are recognized by their rapid rates. If either VT or VF is sensed, the pulse generator delivers defibrillation or a synchronized cardioversion to terminate the rhythm. Other accelerated rhythms will initiate a pacing therapy intended to restore the rate within the preprogrammed limits.
According to guidelines developed jointly by the ACC, AHA, and HRS, class I indications for an ICD include the following:
- Survivor of cardiac arrest due to ventricular fibrillation (VF) or sustained ventricular tachycardia (VT)
- Structural heart disease with VT
- History of syncope of undetermined origin with clinically relevant VF or sustained VT induced during an electrophysiology study
- Left ventricular dysfunction due to myocardial infarction (post ≥40 days) with an ejection fraction (EF) ≤35% and NYHA class II or III or an EF ≤30% and NYHA class I
- Nonischemic dilated cardiomyopathy with an EF ≤35% and NYHA class II or III
- Nonsustained VT due to myocardial infarction with an EF ≤40% and VF or sustained VT induced during electrophysiology study
Combination Pacemaker - Defibrillator Devices
Some implantable devices are capable of providing both pacing and defibrillation. Recent evolution in terminology of pacemakers and defibrillators is toward calling them cardiac resynchronization therapy (CRT), with subclasses that provide pacing alone (CRT-P) and those that provide both pacing and defibrillation (CRT-D).
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Risk factors for coronary artery disease
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis.
Hypertension and Dyslipidemia
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis. When both conditions are present, the likelihood of having clinically significant CAD is drastically increased because atherosclerosis develops in areas of arteries that experience high blood pressure when high levels of low-density lipoprotein (LDL) are present. Because of this interrelationship and the role of exercise in mitigating these two conditions, hypertension and dyslipidemia are discussed here as linked CAD risk factors.
Basic Pathophysiology
The basic pathophysiology of these conditions is closely interrelated but is discussed separately to highlight key issues.
Hypertension
Hypertension (HTN) is a very common chronic condition, affecting about one in five people; it is defined as either
- systolic blood pressure (BP) over 139 mmHg or
- diastolic BP over 89 mmHg.
Table 6.1 has a more complete description of the classes of hypertension. High BP increases the risk for nonfatal and fatal cardiovascular disease, particularly CAD, kidney disease, and stroke. Even BP that is increased but not meeting the criteria for hypertension causes cardiovascular disease.
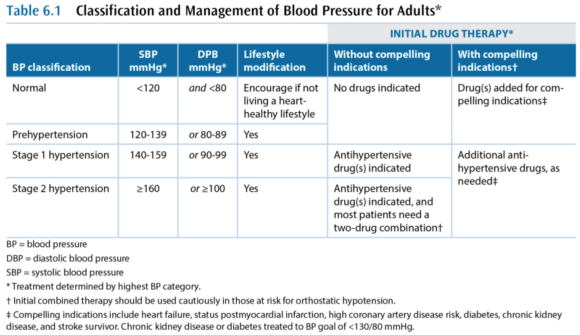
While hypertension is a common condition, the cause is not very well understood. In more than 95% of hypertension cases, the etiology is unknown and the condition is referred to as primary or essential or idiopathic hypertension. The remaining 5% of cases are secondary hypertension, so named because there is an identifiable underlying cause such as sleep apnea, drug-induced or drug-related causes (e.g., chronic corticosteroid therapy), chronic kidney disease, renovascular disease, aldosteronism, Cushing's syndrome, pheochromocytoma, coarctation of the aorta, and hyperthyroidism.
Dyslipidemia
Dyslipidemia - a high level of blood lipids - is a complex set of conditions, but the main concern is a high level of cholesterol. Cholesterol is critically important to every cell in the body, as a constituent of cell membranes that helps regulate their stability. Cholesterol is also an intermediary compound in steroid hormones, but the amount of cholesterol needed for hormones is many orders of magnitude lower than that needed for cell membranes. Cholesterol is synthesized and metabolized in the liver and then transported between the liver and the rest of the body. Cholesterol is not soluble in blood plasma and therefore has to be transported in the blood by lipoproteins. There are many different lipoproteins, each functioning to guide the cholesterol it carries to the proper metabolic pathway. This is the basic triad of lipoproteins:
- Very low-density lipoprotein (VLDL)
- Low-density lipoprotein (LDL)
- High-density lipoprotein (HDL)
The VLDL fraction carries about 80% triglycerides and 20% cholesterol, while the LDL and HDL mainly carry cholesterol. The total blood cholesterol is the sum of the cholesterol bound to VLDL, LDL, and HDL, and these cholesterol subcomponents are indicated with a -C suffix (e.g., LDL-C). Several subclassifications also exist, including two notable subclasses of LDL:
- Lipoprotein (a)
- Small dense LDL
Cholesterol metabolism is extremely complex, but the most important issue is that elevated total cholesterol and low-density lipoprotein cholesterol (LDL-C) are associated with an increased risk of CAD. Lipoprotein (a), or Lp(a), increases risk of CAD and of developing a thrombus, and small dense LDL also increases CAD risk. In contrast, high-density lipoprotein cholesterol (HDL-C) decreases CAD risk, through a cardioprotective effect that is partially related to this lipoprotein's role in the reverse cholesterol transport. In reverse transport, the cholesterol in HDL-C is transported to the liver where it is catabolized and excreted as bile.
Terms Often Used to Refer to Blood Lipids
- dyslipidemia - elevated triglycerides and cholesterol
- hypercholesterolemia - only cholesterol is elevated
- hypertriglyceridemia - only triglycerides are elevated
- exaggerated postprandial lipemia - prolonged elevation of triglycerides following consumption of dietary fat
- hyperlipoproteinemia or dyslipoproteinemia - high lipoprotein concentrations from genetic abnormalities or an underlying condition such as diabetes, renal disease, hypothyroidism, biliary obstruction, or dysproteinemia
Management and Medications
Medical management in persons who have the common chronic conditions often involves one or more medications for each condition, such that people with cardiometabolic conditions are often on five to eight prescription medicines. Again, this discussion treats these independently, but readers should expect to see multiple medications in persons in this group.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Case Study: Diabetes and Obesity with Osteoarthrosis
I intend to live into my 90s but I can’t get there unless I’m dancing. A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk.
Type 2 Diabetes and Obesity With Osteoarthrosis
Presenter: Geoffrey E. Moore, MD, FACSM
S
"I intend to live into my 90s but I can't get there unless I'm dancing."
A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk. Her recent A1c values had been 6.5-6.6, and her a.m. fasting glucose was recently 102. She qualified as T2DM by A1c criteria but wasn't working on her diet or weight and had refused to start taking metformin, and her primary care physician was increasingly concerned.
She expressed a desire to be more active through dance, which she had loved since childhood and felt was a part of her culture (having immigrated to the United States as a child). She expressed little concern about her weight and was more worried that the pain in her L shoulder kept her from dancing. She had first experienced the shoulder problem 10 years earlier while swimming backstroke. She had been to physical therapy (PT) twice, which made it worse. She also had received subacromial cortisone injections, but the relief didn't last. Her shoulder is worse at night (rolls over on her left side); the pain was rated 8/10 and was daily and constant except for sharp pain that radiated to the side of the neck when she moved the shoulder too much. She tried not to take pain or anti-inflammatory medications because she said they "wreck her stomach." Acupuncture (cupping) helped.
She also noted a history of her L knee "giving out," causing falls, and of having 2 knee arthroscopic surgeries (4 and 10 years earlier). When she overdoes weight-bearing activity, her left knee swells "like a watermelon." She did PT after the surgeries and gets to her normal daily activities but can't dance.
O
- Height: 5 ft 4¾ in. (1.65 m)
- Weight: 234.4 lb (106.3 kg)
- BMI: 39 kg/m2
- HR: 65 contractions/min
- BP: 188/98 mmHg
Pertinent Exam
- General: normal development, good nutrition, obese body habitus, no deformities
- CV: regular rhythm with normal S1 and S2, without rubs, gallops, or murmurs; distal pulses/circulation normal; no edema
- Musculoskeletal:
- Normal gait and station, muscular build especially of lower extremities
- Valgus alignment of both knees, no tenderness but the L knee has a small effusion
- Normal ROM without pain, substantial crepitus in both knees
- Left shoulder-specific tests:
- + Painful arc
- + Glenohumeral laxity, with crepitus
- + Neer test, +/- Hawkins test, +/- Speed's test
- + Painful with resisted external rotation, - pain with resisted internal rotation
- + AC joint tenderness
X Rays
- Osteoarthrosis in the acromioclavicular joint; severe osteoarthrosis in the glenohumeral joint with advanced sclerosis, subchondral cysts, and spurring; subluxed position of the humeral head at rest
Medications
- Coreg 10 mg once daily
- Diovan HCT 320/12.5 once daily
- Multivitamin once daily
A
- Increased CV risk: HTN, hyperlipidemia, diabetes by A1c criteria, sleep apnea, obesity
- Advanced glenohumeral osteoarthrosis and reduced function due to pain, status post - bilateral partial meniscectomies
Her shoulder markedly diminishes quality of life, impairing her ability to sleep and to recreate. Dance is her preferred form of physical activity, which she wants to do as her approach to improve the blood glucose and reduce her CV risk profile.
P
- L shoulder OA: refer to PT shoulder specialist
- It was explained that her shoulder would take a long time to get better, but she was likely to have some gains in reduced pain and better function after 3-6 months of PT
- Ibuprofen 500 mg every 8-12 hours and prior to bedtime as needed for pain
- Dance for exercise, but any dances that cause pain should be avoided
- Review on the difference between pain and discomfort
- High cardiovascular risk: She was not interested in addressing her cardiometabolic risk at the time of the first visit.
Goals
- Pain-free near-normal physical functioning of L shoulder
- Dance, including tango, for recreation and physical activity
- Physical therapy focused on rotator cuff and scapular stabilizer strengthening, postural control, manual therapy, and education on pain avoidance
- Gentle dancing that avoids painful arm movements started, daily for 30 min
- Dancing and daily activities to be increased as tolerated (i.e., shoulder discomfort)
Exercise Program
- Physical therapy twice weekly
- Home exercises daily, as advised by therapist
- Dancing that does not cause pain allowed as tolerated
Follow-Up
- L shoulder OA
- Pain-avoidance techniques gave rapidly improved physical functioning of L upper extremity.
- Physical therapy made good progress over 3 months to near-normal physical functioning.
- Dance for aerobic exercise was very successful in getting her motivated.
- High cardiovascular risk
After 2 months of PT, she was motivated to work on weight management and diabetes prevention. She enrolled in a partial meal-replacement lifestyle intervention plan, lost 25 lb (11.3 kg) over the subsequent 3 months, and her fasting blood glucose/A1c returned to normal.
Senior Editor's Comment
This patient's story illustrates some of the art of exercise medicine, revealing the importance of working with patients to meet their emotional expectations and needs. Her primary care team was concerned about the diabetes and had been advising her about diet, weight loss, and taking metformin, but this was less important to the patient than the loss of her ability to dance. Dancing was the only type of physical exercise she enjoyed, so she needed to be able to dance as part of her pathway to improving insulin sensitivity. Close liaison with the physical therapist facilitated the process, because the therapist provided her with tips on how to avoid painful movements and begin to dance immediately. By accepting the need to dance as her top priority and then working to help overcome her barriers to dancing, the lifestyle intervention team gained her faith in them and she began to follow their advice on diet and weight. This approach seemed unusual to many who were involved in her care, as it appeared to put the diabetes problem on hold while focusing on a painful shoulder. But from another perspective, the painful shoulder was the most important problem to the patient and thus a significant barrier that needed to be overcome if exercise (in the form of dance) was to become her most important medicine.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
A Closer Look at Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons: There are thousands of chronic conditions and causes of disability.
Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons:
- There are thousands of chronic conditions and causes of disability.
- The vast majority of recommendations seem similar for most chronic conditions.
- Ultimately, exercise is fairly simple and needs to be seen as elegantly powerful.
- The complexities and nuances are matters of clinical judgment for safety's sake.
- The main concern in the chronic conditions in CDD4 is loss of independent living, which is primarily a function of light-intensity physical activities.
For these reasons, the Basic CDD4 Recommendations are consistent with but differ very slightly from the Guidelines and from the various physical activity guidelines discussed in the preceding section, because the CDD4 editors also want to make certain that sufficient attention is paid to light-intensity physical activity, especially the ability to perform instrumental activities of daily living with the goal of having patients remain independent. With these considerations in mind, the Basic CDD4 Recommendations are as follows:
- Every person with a chronic condition should be physically active, accumulating a minimum weekly total of
- 150 min of preferably moderate-intensity physical activity or, if that is too difficult, then
- 150 min of light-intensity physical activity may be substituted.
- At least 2 days per week of flexibility and muscle strengthening activities that should minimally involve
- chair sit-and-reach stretches on left and right,
- at least eight consecutive sit-to-stand exercises,
- at least 10 step-ups (or a flight of steps), leading with each foot, and
- at least eight consecutive arm curls with a minimum of 2 kg held in the hand; 4 kg is recommended.
- Individuals at risk for falls should be evaluated for causes of falls. Not all falls are caused by a condition that can be treated with exercise training. If the diagnosis of the causes suggests that exercise training can reduce the likelihood of a fall, then activities to improve balance should be incorporated into individuals' exercise regimens, under the supervision of an exercise therapist trained in fall prevention.
The higher the aerobic intensity, muscle forces, and required range of motion, the greater the likelihood of an adverse event.
These Basic CDD4 Recommendations are summarized in table 2.4. Readers should always bear in mind the goals behind the Basic CDD4 Recommendations, because these goals are helpful in drafting an individualized program to meet the unique needs of each patient. Everyone should be physically active to an extent sufficient to maintain independent living:

- Let no barrier block someone from doing light-intensity physical activity.
- Independent living requires a minimum ability to perform activities involving (or demanding)
- light-intensity aerobic work (or exertion), combined with
- strength, flexibility, and balance and coordination.
Adverse events from exercise cannot be completely eliminated, but there are two main categories to consider:
- Activity-dependent risks (due to the nature of the activity)
- Disease-dependent risks (those that relate to the pathophysiology)
The best way to minimize activity-dependent risks is to encourage the patient to practice safety precautions. If there is concern that the individual cannot do this independently, then he needs a supervised exercise program, at least to get started.
One major concern is whether or not the advice to do physical activity exposes the patient to the possibility of a disease-dependent risk. Such risks are associated with the intensity of exercise. Accordingly, if the recommendation is to complete vigorous- or high-intensity physical activities, it is prudent to follow the Guidelines on exercise testing and prescription. Most people with a chronic condition can safely participate in moderate-intensity physical activity, and if there is any concern that a particular individual cannot do so, she should either undergo some disease-specific diagnostic exercise testing or be referred to a supervised exercise program (or both).
There are few data beyond anecdotal cases to support the concern that light-intensity physical activities are likely to precipitate a disease-dependent adverse event (especially sudden death or myocardial infarction). Discerning the epidemiological role of light activities in precipitating such events would be exquisitely difficult, because participation in light-intensity activities is so ubiquitous in daily life. If someone is medically unstable to the point that activities of daily living threaten injury or death, then the Basic CDD4 Recommendations do not apply because the individual is not able to maintain independence and belongs in either a hospital or a nursing home. Indeed, it is likely that many people end up in a nursing facility sooner than they need to because no one recommended that they do light-intensity physical activity.
These nuances of safety are a key reason why an exercise professional is a necessary member of the chronic care team, because these staff are trained and have the experience to make good judgments regarding when exercise is safe and when it is not safe. See chapter 3 for a more in-depth discussion on how these judgments are made, which often involves more art than science.
Learn how to prescribe physical activity or exercise in chronic care in ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Permanent Pacemakers and Implantable Cardioverter-Defibrillators
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both.
Permanent Pacemakers
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both. In persons who have light-headedness, syncopal spells, shortness of breath, and more rarely chest pain or other cardiovascular symptoms owing to these problems, a permanent pacemaker
- improves symptoms,
- enhances exercise performance, and
- improves quality of life.
According to guidelines developed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS), class I indications for a permanent pacemaker include the following:
- Sinus node dysfunction
- Third-degree block and advanced second-degree AV block
- Hypersensitive carotid sinus syndrome
- Symptomatic bradycardia
- Sustained pause-dependent ventricular tachycardia
- Left ventricular systolic dysfunction and New York Heart Association (NYHA) functional class III or ambulatory class IV
A typical pacemaker system consists of two basic components: a pulse generator and either one or two pacing wires. In a traditional pacemaker the pacing wires are insulated and are implanted transvenously into the right atrium, right ventricle, or both. With a biventricular pacemaker, a lead is also placed in the left ventricle. The leads are connected to the pulse generator, which is typically implanted subcutaneously just below the clavicle. The two main functions of the leads are sensing and pacing. Sensing involves detecting electrical signals (i.e., P-waves and R-waves) from the heart. When these signals are not sensed at the proper timing, the pacemaker generator fires an impulse that causes the atria or ventricles (or both) to contract. Optimally, the pacing system uses an atrial and ventricular lead to maintain AV synchrony, which serves to optimize cardiac output at rest and during exercise.
Pacemakers are described by a standardized code. The first letter represents the chamber paced; the second is the chamber sensed; and the third denotes the response to a sensed event. The fourth position is used to indicate that the pacemaker has rate-response capabilities. For example, VVIR is the abbreviation used when the ventricle (V) is the chamber being paced and sensed. When the pacemaker senses a normal ventricular contraction, the pacemaker is inhibited (I). The "R" indicates that the pulse generator is rate-responsive during exercise. The response by the pacemaker is to either trigger or inhibit a pacing stimulus, depending on the absence or presence, respectively, of atrial or ventricular conduction, separately or in combination, relative to the range of heart rates that are programmed into the pacer.
A commonly used mode of pacing is the DDDR, which has dual-chamber (i.e., atrium and ventricle) pacing and inhibiting and has rate-response capability. The DDDR pacemaker is widely regarded as the optimal pacing mode in individuals who have normal sinoatrial (SA) node function, because it provides AV synchrony and uses the client's own sinus rhythm to guide ventricular stimulation. This results in a heart rate and cardiac output that, for the rest of the circulatory system, is very nearly normal.
Implantable Cardioverter-Defibrillators
An implantable cardioverter-defibrillator (ICD) is another electronic device that can be permanently implanted in individuals who either have a history of, or are at increased risk for, a life-threatening ventricular dysrhythmia. These devices impressively reduce mortality in persons with cardiomyopathy. Cardioverter-defibrillators can be just an ICD or can be a model that functions as both an ICD and a permanent pacemaker; like pacemakers, they are usually implanted subcutaneously just below the clavicle.
Implantable cardioverter-defibrillators electrically terminate life-threatening ventricular tachyarrhythmias. They consist of two basic parts: the lead system and the ICD itself. Implantable cardioverter-defibrillators have lead systems that are placed transvenously, typically by way of the subclavian vein. The ICD leads pick up the electrical rhythm of the heart and transmit this to the pulse generator, which senses the rhythm. Implantable cardioverter-defibrillators can detect atrial and ventricular arrhythmias, can provide antitachycardia pacing and defibrillation, and can be programmed with multiple protocols and the ability to record an electrocardiogram. Ventricular tachycardia (VT) and ventricular fibrillation (VF) are recognized by their rapid rates. If either VT or VF is sensed, the pulse generator delivers defibrillation or a synchronized cardioversion to terminate the rhythm. Other accelerated rhythms will initiate a pacing therapy intended to restore the rate within the preprogrammed limits.
According to guidelines developed jointly by the ACC, AHA, and HRS, class I indications for an ICD include the following:
- Survivor of cardiac arrest due to ventricular fibrillation (VF) or sustained ventricular tachycardia (VT)
- Structural heart disease with VT
- History of syncope of undetermined origin with clinically relevant VF or sustained VT induced during an electrophysiology study
- Left ventricular dysfunction due to myocardial infarction (post ≥40 days) with an ejection fraction (EF) ≤35% and NYHA class II or III or an EF ≤30% and NYHA class I
- Nonischemic dilated cardiomyopathy with an EF ≤35% and NYHA class II or III
- Nonsustained VT due to myocardial infarction with an EF ≤40% and VF or sustained VT induced during electrophysiology study
Combination Pacemaker - Defibrillator Devices
Some implantable devices are capable of providing both pacing and defibrillation. Recent evolution in terminology of pacemakers and defibrillators is toward calling them cardiac resynchronization therapy (CRT), with subclasses that provide pacing alone (CRT-P) and those that provide both pacing and defibrillation (CRT-D).
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Risk factors for coronary artery disease
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis.
Hypertension and Dyslipidemia
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis. When both conditions are present, the likelihood of having clinically significant CAD is drastically increased because atherosclerosis develops in areas of arteries that experience high blood pressure when high levels of low-density lipoprotein (LDL) are present. Because of this interrelationship and the role of exercise in mitigating these two conditions, hypertension and dyslipidemia are discussed here as linked CAD risk factors.
Basic Pathophysiology
The basic pathophysiology of these conditions is closely interrelated but is discussed separately to highlight key issues.
Hypertension
Hypertension (HTN) is a very common chronic condition, affecting about one in five people; it is defined as either
- systolic blood pressure (BP) over 139 mmHg or
- diastolic BP over 89 mmHg.
Table 6.1 has a more complete description of the classes of hypertension. High BP increases the risk for nonfatal and fatal cardiovascular disease, particularly CAD, kidney disease, and stroke. Even BP that is increased but not meeting the criteria for hypertension causes cardiovascular disease.
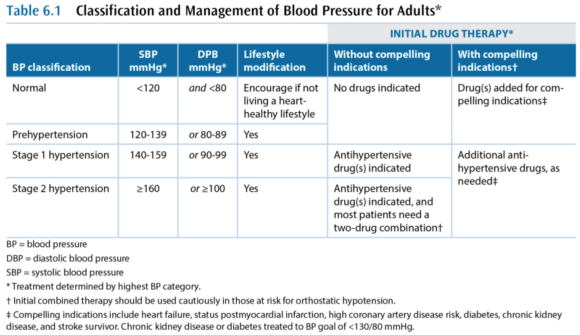
While hypertension is a common condition, the cause is not very well understood. In more than 95% of hypertension cases, the etiology is unknown and the condition is referred to as primary or essential or idiopathic hypertension. The remaining 5% of cases are secondary hypertension, so named because there is an identifiable underlying cause such as sleep apnea, drug-induced or drug-related causes (e.g., chronic corticosteroid therapy), chronic kidney disease, renovascular disease, aldosteronism, Cushing's syndrome, pheochromocytoma, coarctation of the aorta, and hyperthyroidism.
Dyslipidemia
Dyslipidemia - a high level of blood lipids - is a complex set of conditions, but the main concern is a high level of cholesterol. Cholesterol is critically important to every cell in the body, as a constituent of cell membranes that helps regulate their stability. Cholesterol is also an intermediary compound in steroid hormones, but the amount of cholesterol needed for hormones is many orders of magnitude lower than that needed for cell membranes. Cholesterol is synthesized and metabolized in the liver and then transported between the liver and the rest of the body. Cholesterol is not soluble in blood plasma and therefore has to be transported in the blood by lipoproteins. There are many different lipoproteins, each functioning to guide the cholesterol it carries to the proper metabolic pathway. This is the basic triad of lipoproteins:
- Very low-density lipoprotein (VLDL)
- Low-density lipoprotein (LDL)
- High-density lipoprotein (HDL)
The VLDL fraction carries about 80% triglycerides and 20% cholesterol, while the LDL and HDL mainly carry cholesterol. The total blood cholesterol is the sum of the cholesterol bound to VLDL, LDL, and HDL, and these cholesterol subcomponents are indicated with a -C suffix (e.g., LDL-C). Several subclassifications also exist, including two notable subclasses of LDL:
- Lipoprotein (a)
- Small dense LDL
Cholesterol metabolism is extremely complex, but the most important issue is that elevated total cholesterol and low-density lipoprotein cholesterol (LDL-C) are associated with an increased risk of CAD. Lipoprotein (a), or Lp(a), increases risk of CAD and of developing a thrombus, and small dense LDL also increases CAD risk. In contrast, high-density lipoprotein cholesterol (HDL-C) decreases CAD risk, through a cardioprotective effect that is partially related to this lipoprotein's role in the reverse cholesterol transport. In reverse transport, the cholesterol in HDL-C is transported to the liver where it is catabolized and excreted as bile.
Terms Often Used to Refer to Blood Lipids
- dyslipidemia - elevated triglycerides and cholesterol
- hypercholesterolemia - only cholesterol is elevated
- hypertriglyceridemia - only triglycerides are elevated
- exaggerated postprandial lipemia - prolonged elevation of triglycerides following consumption of dietary fat
- hyperlipoproteinemia or dyslipoproteinemia - high lipoprotein concentrations from genetic abnormalities or an underlying condition such as diabetes, renal disease, hypothyroidism, biliary obstruction, or dysproteinemia
Management and Medications
Medical management in persons who have the common chronic conditions often involves one or more medications for each condition, such that people with cardiometabolic conditions are often on five to eight prescription medicines. Again, this discussion treats these independently, but readers should expect to see multiple medications in persons in this group.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Case Study: Diabetes and Obesity with Osteoarthrosis
I intend to live into my 90s but I can’t get there unless I’m dancing. A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk.
Type 2 Diabetes and Obesity With Osteoarthrosis
Presenter: Geoffrey E. Moore, MD, FACSM
S
"I intend to live into my 90s but I can't get there unless I'm dancing."
A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk. Her recent A1c values had been 6.5-6.6, and her a.m. fasting glucose was recently 102. She qualified as T2DM by A1c criteria but wasn't working on her diet or weight and had refused to start taking metformin, and her primary care physician was increasingly concerned.
She expressed a desire to be more active through dance, which she had loved since childhood and felt was a part of her culture (having immigrated to the United States as a child). She expressed little concern about her weight and was more worried that the pain in her L shoulder kept her from dancing. She had first experienced the shoulder problem 10 years earlier while swimming backstroke. She had been to physical therapy (PT) twice, which made it worse. She also had received subacromial cortisone injections, but the relief didn't last. Her shoulder is worse at night (rolls over on her left side); the pain was rated 8/10 and was daily and constant except for sharp pain that radiated to the side of the neck when she moved the shoulder too much. She tried not to take pain or anti-inflammatory medications because she said they "wreck her stomach." Acupuncture (cupping) helped.
She also noted a history of her L knee "giving out," causing falls, and of having 2 knee arthroscopic surgeries (4 and 10 years earlier). When she overdoes weight-bearing activity, her left knee swells "like a watermelon." She did PT after the surgeries and gets to her normal daily activities but can't dance.
O
- Height: 5 ft 4¾ in. (1.65 m)
- Weight: 234.4 lb (106.3 kg)
- BMI: 39 kg/m2
- HR: 65 contractions/min
- BP: 188/98 mmHg
Pertinent Exam
- General: normal development, good nutrition, obese body habitus, no deformities
- CV: regular rhythm with normal S1 and S2, without rubs, gallops, or murmurs; distal pulses/circulation normal; no edema
- Musculoskeletal:
- Normal gait and station, muscular build especially of lower extremities
- Valgus alignment of both knees, no tenderness but the L knee has a small effusion
- Normal ROM without pain, substantial crepitus in both knees
- Left shoulder-specific tests:
- + Painful arc
- + Glenohumeral laxity, with crepitus
- + Neer test, +/- Hawkins test, +/- Speed's test
- + Painful with resisted external rotation, - pain with resisted internal rotation
- + AC joint tenderness
X Rays
- Osteoarthrosis in the acromioclavicular joint; severe osteoarthrosis in the glenohumeral joint with advanced sclerosis, subchondral cysts, and spurring; subluxed position of the humeral head at rest
Medications
- Coreg 10 mg once daily
- Diovan HCT 320/12.5 once daily
- Multivitamin once daily
A
- Increased CV risk: HTN, hyperlipidemia, diabetes by A1c criteria, sleep apnea, obesity
- Advanced glenohumeral osteoarthrosis and reduced function due to pain, status post - bilateral partial meniscectomies
Her shoulder markedly diminishes quality of life, impairing her ability to sleep and to recreate. Dance is her preferred form of physical activity, which she wants to do as her approach to improve the blood glucose and reduce her CV risk profile.
P
- L shoulder OA: refer to PT shoulder specialist
- It was explained that her shoulder would take a long time to get better, but she was likely to have some gains in reduced pain and better function after 3-6 months of PT
- Ibuprofen 500 mg every 8-12 hours and prior to bedtime as needed for pain
- Dance for exercise, but any dances that cause pain should be avoided
- Review on the difference between pain and discomfort
- High cardiovascular risk: She was not interested in addressing her cardiometabolic risk at the time of the first visit.
Goals
- Pain-free near-normal physical functioning of L shoulder
- Dance, including tango, for recreation and physical activity
- Physical therapy focused on rotator cuff and scapular stabilizer strengthening, postural control, manual therapy, and education on pain avoidance
- Gentle dancing that avoids painful arm movements started, daily for 30 min
- Dancing and daily activities to be increased as tolerated (i.e., shoulder discomfort)
Exercise Program
- Physical therapy twice weekly
- Home exercises daily, as advised by therapist
- Dancing that does not cause pain allowed as tolerated
Follow-Up
- L shoulder OA
- Pain-avoidance techniques gave rapidly improved physical functioning of L upper extremity.
- Physical therapy made good progress over 3 months to near-normal physical functioning.
- Dance for aerobic exercise was very successful in getting her motivated.
- High cardiovascular risk
After 2 months of PT, she was motivated to work on weight management and diabetes prevention. She enrolled in a partial meal-replacement lifestyle intervention plan, lost 25 lb (11.3 kg) over the subsequent 3 months, and her fasting blood glucose/A1c returned to normal.
Senior Editor's Comment
This patient's story illustrates some of the art of exercise medicine, revealing the importance of working with patients to meet their emotional expectations and needs. Her primary care team was concerned about the diabetes and had been advising her about diet, weight loss, and taking metformin, but this was less important to the patient than the loss of her ability to dance. Dancing was the only type of physical exercise she enjoyed, so she needed to be able to dance as part of her pathway to improving insulin sensitivity. Close liaison with the physical therapist facilitated the process, because the therapist provided her with tips on how to avoid painful movements and begin to dance immediately. By accepting the need to dance as her top priority and then working to help overcome her barriers to dancing, the lifestyle intervention team gained her faith in them and she began to follow their advice on diet and weight. This approach seemed unusual to many who were involved in her care, as it appeared to put the diabetes problem on hold while focusing on a painful shoulder. But from another perspective, the painful shoulder was the most important problem to the patient and thus a significant barrier that needed to be overcome if exercise (in the form of dance) was to become her most important medicine.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
A Closer Look at Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons: There are thousands of chronic conditions and causes of disability.
Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons:
- There are thousands of chronic conditions and causes of disability.
- The vast majority of recommendations seem similar for most chronic conditions.
- Ultimately, exercise is fairly simple and needs to be seen as elegantly powerful.
- The complexities and nuances are matters of clinical judgment for safety's sake.
- The main concern in the chronic conditions in CDD4 is loss of independent living, which is primarily a function of light-intensity physical activities.
For these reasons, the Basic CDD4 Recommendations are consistent with but differ very slightly from the Guidelines and from the various physical activity guidelines discussed in the preceding section, because the CDD4 editors also want to make certain that sufficient attention is paid to light-intensity physical activity, especially the ability to perform instrumental activities of daily living with the goal of having patients remain independent. With these considerations in mind, the Basic CDD4 Recommendations are as follows:
- Every person with a chronic condition should be physically active, accumulating a minimum weekly total of
- 150 min of preferably moderate-intensity physical activity or, if that is too difficult, then
- 150 min of light-intensity physical activity may be substituted.
- At least 2 days per week of flexibility and muscle strengthening activities that should minimally involve
- chair sit-and-reach stretches on left and right,
- at least eight consecutive sit-to-stand exercises,
- at least 10 step-ups (or a flight of steps), leading with each foot, and
- at least eight consecutive arm curls with a minimum of 2 kg held in the hand; 4 kg is recommended.
- Individuals at risk for falls should be evaluated for causes of falls. Not all falls are caused by a condition that can be treated with exercise training. If the diagnosis of the causes suggests that exercise training can reduce the likelihood of a fall, then activities to improve balance should be incorporated into individuals' exercise regimens, under the supervision of an exercise therapist trained in fall prevention.
The higher the aerobic intensity, muscle forces, and required range of motion, the greater the likelihood of an adverse event.
These Basic CDD4 Recommendations are summarized in table 2.4. Readers should always bear in mind the goals behind the Basic CDD4 Recommendations, because these goals are helpful in drafting an individualized program to meet the unique needs of each patient. Everyone should be physically active to an extent sufficient to maintain independent living:

- Let no barrier block someone from doing light-intensity physical activity.
- Independent living requires a minimum ability to perform activities involving (or demanding)
- light-intensity aerobic work (or exertion), combined with
- strength, flexibility, and balance and coordination.
Adverse events from exercise cannot be completely eliminated, but there are two main categories to consider:
- Activity-dependent risks (due to the nature of the activity)
- Disease-dependent risks (those that relate to the pathophysiology)
The best way to minimize activity-dependent risks is to encourage the patient to practice safety precautions. If there is concern that the individual cannot do this independently, then he needs a supervised exercise program, at least to get started.
One major concern is whether or not the advice to do physical activity exposes the patient to the possibility of a disease-dependent risk. Such risks are associated with the intensity of exercise. Accordingly, if the recommendation is to complete vigorous- or high-intensity physical activities, it is prudent to follow the Guidelines on exercise testing and prescription. Most people with a chronic condition can safely participate in moderate-intensity physical activity, and if there is any concern that a particular individual cannot do so, she should either undergo some disease-specific diagnostic exercise testing or be referred to a supervised exercise program (or both).
There are few data beyond anecdotal cases to support the concern that light-intensity physical activities are likely to precipitate a disease-dependent adverse event (especially sudden death or myocardial infarction). Discerning the epidemiological role of light activities in precipitating such events would be exquisitely difficult, because participation in light-intensity activities is so ubiquitous in daily life. If someone is medically unstable to the point that activities of daily living threaten injury or death, then the Basic CDD4 Recommendations do not apply because the individual is not able to maintain independence and belongs in either a hospital or a nursing home. Indeed, it is likely that many people end up in a nursing facility sooner than they need to because no one recommended that they do light-intensity physical activity.
These nuances of safety are a key reason why an exercise professional is a necessary member of the chronic care team, because these staff are trained and have the experience to make good judgments regarding when exercise is safe and when it is not safe. See chapter 3 for a more in-depth discussion on how these judgments are made, which often involves more art than science.
Learn how to prescribe physical activity or exercise in chronic care in ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Permanent Pacemakers and Implantable Cardioverter-Defibrillators
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both.
Permanent Pacemakers
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both. In persons who have light-headedness, syncopal spells, shortness of breath, and more rarely chest pain or other cardiovascular symptoms owing to these problems, a permanent pacemaker
- improves symptoms,
- enhances exercise performance, and
- improves quality of life.
According to guidelines developed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS), class I indications for a permanent pacemaker include the following:
- Sinus node dysfunction
- Third-degree block and advanced second-degree AV block
- Hypersensitive carotid sinus syndrome
- Symptomatic bradycardia
- Sustained pause-dependent ventricular tachycardia
- Left ventricular systolic dysfunction and New York Heart Association (NYHA) functional class III or ambulatory class IV
A typical pacemaker system consists of two basic components: a pulse generator and either one or two pacing wires. In a traditional pacemaker the pacing wires are insulated and are implanted transvenously into the right atrium, right ventricle, or both. With a biventricular pacemaker, a lead is also placed in the left ventricle. The leads are connected to the pulse generator, which is typically implanted subcutaneously just below the clavicle. The two main functions of the leads are sensing and pacing. Sensing involves detecting electrical signals (i.e., P-waves and R-waves) from the heart. When these signals are not sensed at the proper timing, the pacemaker generator fires an impulse that causes the atria or ventricles (or both) to contract. Optimally, the pacing system uses an atrial and ventricular lead to maintain AV synchrony, which serves to optimize cardiac output at rest and during exercise.
Pacemakers are described by a standardized code. The first letter represents the chamber paced; the second is the chamber sensed; and the third denotes the response to a sensed event. The fourth position is used to indicate that the pacemaker has rate-response capabilities. For example, VVIR is the abbreviation used when the ventricle (V) is the chamber being paced and sensed. When the pacemaker senses a normal ventricular contraction, the pacemaker is inhibited (I). The "R" indicates that the pulse generator is rate-responsive during exercise. The response by the pacemaker is to either trigger or inhibit a pacing stimulus, depending on the absence or presence, respectively, of atrial or ventricular conduction, separately or in combination, relative to the range of heart rates that are programmed into the pacer.
A commonly used mode of pacing is the DDDR, which has dual-chamber (i.e., atrium and ventricle) pacing and inhibiting and has rate-response capability. The DDDR pacemaker is widely regarded as the optimal pacing mode in individuals who have normal sinoatrial (SA) node function, because it provides AV synchrony and uses the client's own sinus rhythm to guide ventricular stimulation. This results in a heart rate and cardiac output that, for the rest of the circulatory system, is very nearly normal.
Implantable Cardioverter-Defibrillators
An implantable cardioverter-defibrillator (ICD) is another electronic device that can be permanently implanted in individuals who either have a history of, or are at increased risk for, a life-threatening ventricular dysrhythmia. These devices impressively reduce mortality in persons with cardiomyopathy. Cardioverter-defibrillators can be just an ICD or can be a model that functions as both an ICD and a permanent pacemaker; like pacemakers, they are usually implanted subcutaneously just below the clavicle.
Implantable cardioverter-defibrillators electrically terminate life-threatening ventricular tachyarrhythmias. They consist of two basic parts: the lead system and the ICD itself. Implantable cardioverter-defibrillators have lead systems that are placed transvenously, typically by way of the subclavian vein. The ICD leads pick up the electrical rhythm of the heart and transmit this to the pulse generator, which senses the rhythm. Implantable cardioverter-defibrillators can detect atrial and ventricular arrhythmias, can provide antitachycardia pacing and defibrillation, and can be programmed with multiple protocols and the ability to record an electrocardiogram. Ventricular tachycardia (VT) and ventricular fibrillation (VF) are recognized by their rapid rates. If either VT or VF is sensed, the pulse generator delivers defibrillation or a synchronized cardioversion to terminate the rhythm. Other accelerated rhythms will initiate a pacing therapy intended to restore the rate within the preprogrammed limits.
According to guidelines developed jointly by the ACC, AHA, and HRS, class I indications for an ICD include the following:
- Survivor of cardiac arrest due to ventricular fibrillation (VF) or sustained ventricular tachycardia (VT)
- Structural heart disease with VT
- History of syncope of undetermined origin with clinically relevant VF or sustained VT induced during an electrophysiology study
- Left ventricular dysfunction due to myocardial infarction (post ≥40 days) with an ejection fraction (EF) ≤35% and NYHA class II or III or an EF ≤30% and NYHA class I
- Nonischemic dilated cardiomyopathy with an EF ≤35% and NYHA class II or III
- Nonsustained VT due to myocardial infarction with an EF ≤40% and VF or sustained VT induced during electrophysiology study
Combination Pacemaker - Defibrillator Devices
Some implantable devices are capable of providing both pacing and defibrillation. Recent evolution in terminology of pacemakers and defibrillators is toward calling them cardiac resynchronization therapy (CRT), with subclasses that provide pacing alone (CRT-P) and those that provide both pacing and defibrillation (CRT-D).
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Risk factors for coronary artery disease
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis.
Hypertension and Dyslipidemia
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis. When both conditions are present, the likelihood of having clinically significant CAD is drastically increased because atherosclerosis develops in areas of arteries that experience high blood pressure when high levels of low-density lipoprotein (LDL) are present. Because of this interrelationship and the role of exercise in mitigating these two conditions, hypertension and dyslipidemia are discussed here as linked CAD risk factors.
Basic Pathophysiology
The basic pathophysiology of these conditions is closely interrelated but is discussed separately to highlight key issues.
Hypertension
Hypertension (HTN) is a very common chronic condition, affecting about one in five people; it is defined as either
- systolic blood pressure (BP) over 139 mmHg or
- diastolic BP over 89 mmHg.
Table 6.1 has a more complete description of the classes of hypertension. High BP increases the risk for nonfatal and fatal cardiovascular disease, particularly CAD, kidney disease, and stroke. Even BP that is increased but not meeting the criteria for hypertension causes cardiovascular disease.
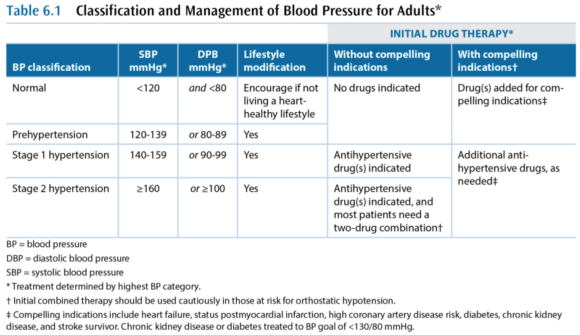
While hypertension is a common condition, the cause is not very well understood. In more than 95% of hypertension cases, the etiology is unknown and the condition is referred to as primary or essential or idiopathic hypertension. The remaining 5% of cases are secondary hypertension, so named because there is an identifiable underlying cause such as sleep apnea, drug-induced or drug-related causes (e.g., chronic corticosteroid therapy), chronic kidney disease, renovascular disease, aldosteronism, Cushing's syndrome, pheochromocytoma, coarctation of the aorta, and hyperthyroidism.
Dyslipidemia
Dyslipidemia - a high level of blood lipids - is a complex set of conditions, but the main concern is a high level of cholesterol. Cholesterol is critically important to every cell in the body, as a constituent of cell membranes that helps regulate their stability. Cholesterol is also an intermediary compound in steroid hormones, but the amount of cholesterol needed for hormones is many orders of magnitude lower than that needed for cell membranes. Cholesterol is synthesized and metabolized in the liver and then transported between the liver and the rest of the body. Cholesterol is not soluble in blood plasma and therefore has to be transported in the blood by lipoproteins. There are many different lipoproteins, each functioning to guide the cholesterol it carries to the proper metabolic pathway. This is the basic triad of lipoproteins:
- Very low-density lipoprotein (VLDL)
- Low-density lipoprotein (LDL)
- High-density lipoprotein (HDL)
The VLDL fraction carries about 80% triglycerides and 20% cholesterol, while the LDL and HDL mainly carry cholesterol. The total blood cholesterol is the sum of the cholesterol bound to VLDL, LDL, and HDL, and these cholesterol subcomponents are indicated with a -C suffix (e.g., LDL-C). Several subclassifications also exist, including two notable subclasses of LDL:
- Lipoprotein (a)
- Small dense LDL
Cholesterol metabolism is extremely complex, but the most important issue is that elevated total cholesterol and low-density lipoprotein cholesterol (LDL-C) are associated with an increased risk of CAD. Lipoprotein (a), or Lp(a), increases risk of CAD and of developing a thrombus, and small dense LDL also increases CAD risk. In contrast, high-density lipoprotein cholesterol (HDL-C) decreases CAD risk, through a cardioprotective effect that is partially related to this lipoprotein's role in the reverse cholesterol transport. In reverse transport, the cholesterol in HDL-C is transported to the liver where it is catabolized and excreted as bile.
Terms Often Used to Refer to Blood Lipids
- dyslipidemia - elevated triglycerides and cholesterol
- hypercholesterolemia - only cholesterol is elevated
- hypertriglyceridemia - only triglycerides are elevated
- exaggerated postprandial lipemia - prolonged elevation of triglycerides following consumption of dietary fat
- hyperlipoproteinemia or dyslipoproteinemia - high lipoprotein concentrations from genetic abnormalities or an underlying condition such as diabetes, renal disease, hypothyroidism, biliary obstruction, or dysproteinemia
Management and Medications
Medical management in persons who have the common chronic conditions often involves one or more medications for each condition, such that people with cardiometabolic conditions are often on five to eight prescription medicines. Again, this discussion treats these independently, but readers should expect to see multiple medications in persons in this group.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Case Study: Diabetes and Obesity with Osteoarthrosis
I intend to live into my 90s but I can’t get there unless I’m dancing. A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk.
Type 2 Diabetes and Obesity With Osteoarthrosis
Presenter: Geoffrey E. Moore, MD, FACSM
S
"I intend to live into my 90s but I can't get there unless I'm dancing."
A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk. Her recent A1c values had been 6.5-6.6, and her a.m. fasting glucose was recently 102. She qualified as T2DM by A1c criteria but wasn't working on her diet or weight and had refused to start taking metformin, and her primary care physician was increasingly concerned.
She expressed a desire to be more active through dance, which she had loved since childhood and felt was a part of her culture (having immigrated to the United States as a child). She expressed little concern about her weight and was more worried that the pain in her L shoulder kept her from dancing. She had first experienced the shoulder problem 10 years earlier while swimming backstroke. She had been to physical therapy (PT) twice, which made it worse. She also had received subacromial cortisone injections, but the relief didn't last. Her shoulder is worse at night (rolls over on her left side); the pain was rated 8/10 and was daily and constant except for sharp pain that radiated to the side of the neck when she moved the shoulder too much. She tried not to take pain or anti-inflammatory medications because she said they "wreck her stomach." Acupuncture (cupping) helped.
She also noted a history of her L knee "giving out," causing falls, and of having 2 knee arthroscopic surgeries (4 and 10 years earlier). When she overdoes weight-bearing activity, her left knee swells "like a watermelon." She did PT after the surgeries and gets to her normal daily activities but can't dance.
O
- Height: 5 ft 4¾ in. (1.65 m)
- Weight: 234.4 lb (106.3 kg)
- BMI: 39 kg/m2
- HR: 65 contractions/min
- BP: 188/98 mmHg
Pertinent Exam
- General: normal development, good nutrition, obese body habitus, no deformities
- CV: regular rhythm with normal S1 and S2, without rubs, gallops, or murmurs; distal pulses/circulation normal; no edema
- Musculoskeletal:
- Normal gait and station, muscular build especially of lower extremities
- Valgus alignment of both knees, no tenderness but the L knee has a small effusion
- Normal ROM without pain, substantial crepitus in both knees
- Left shoulder-specific tests:
- + Painful arc
- + Glenohumeral laxity, with crepitus
- + Neer test, +/- Hawkins test, +/- Speed's test
- + Painful with resisted external rotation, - pain with resisted internal rotation
- + AC joint tenderness
X Rays
- Osteoarthrosis in the acromioclavicular joint; severe osteoarthrosis in the glenohumeral joint with advanced sclerosis, subchondral cysts, and spurring; subluxed position of the humeral head at rest
Medications
- Coreg 10 mg once daily
- Diovan HCT 320/12.5 once daily
- Multivitamin once daily
A
- Increased CV risk: HTN, hyperlipidemia, diabetes by A1c criteria, sleep apnea, obesity
- Advanced glenohumeral osteoarthrosis and reduced function due to pain, status post - bilateral partial meniscectomies
Her shoulder markedly diminishes quality of life, impairing her ability to sleep and to recreate. Dance is her preferred form of physical activity, which she wants to do as her approach to improve the blood glucose and reduce her CV risk profile.
P
- L shoulder OA: refer to PT shoulder specialist
- It was explained that her shoulder would take a long time to get better, but she was likely to have some gains in reduced pain and better function after 3-6 months of PT
- Ibuprofen 500 mg every 8-12 hours and prior to bedtime as needed for pain
- Dance for exercise, but any dances that cause pain should be avoided
- Review on the difference between pain and discomfort
- High cardiovascular risk: She was not interested in addressing her cardiometabolic risk at the time of the first visit.
Goals
- Pain-free near-normal physical functioning of L shoulder
- Dance, including tango, for recreation and physical activity
- Physical therapy focused on rotator cuff and scapular stabilizer strengthening, postural control, manual therapy, and education on pain avoidance
- Gentle dancing that avoids painful arm movements started, daily for 30 min
- Dancing and daily activities to be increased as tolerated (i.e., shoulder discomfort)
Exercise Program
- Physical therapy twice weekly
- Home exercises daily, as advised by therapist
- Dancing that does not cause pain allowed as tolerated
Follow-Up
- L shoulder OA
- Pain-avoidance techniques gave rapidly improved physical functioning of L upper extremity.
- Physical therapy made good progress over 3 months to near-normal physical functioning.
- Dance for aerobic exercise was very successful in getting her motivated.
- High cardiovascular risk
After 2 months of PT, she was motivated to work on weight management and diabetes prevention. She enrolled in a partial meal-replacement lifestyle intervention plan, lost 25 lb (11.3 kg) over the subsequent 3 months, and her fasting blood glucose/A1c returned to normal.
Senior Editor's Comment
This patient's story illustrates some of the art of exercise medicine, revealing the importance of working with patients to meet their emotional expectations and needs. Her primary care team was concerned about the diabetes and had been advising her about diet, weight loss, and taking metformin, but this was less important to the patient than the loss of her ability to dance. Dancing was the only type of physical exercise she enjoyed, so she needed to be able to dance as part of her pathway to improving insulin sensitivity. Close liaison with the physical therapist facilitated the process, because the therapist provided her with tips on how to avoid painful movements and begin to dance immediately. By accepting the need to dance as her top priority and then working to help overcome her barriers to dancing, the lifestyle intervention team gained her faith in them and she began to follow their advice on diet and weight. This approach seemed unusual to many who were involved in her care, as it appeared to put the diabetes problem on hold while focusing on a painful shoulder. But from another perspective, the painful shoulder was the most important problem to the patient and thus a significant barrier that needed to be overcome if exercise (in the form of dance) was to become her most important medicine.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
A Closer Look at Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons: There are thousands of chronic conditions and causes of disability.
Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons:
- There are thousands of chronic conditions and causes of disability.
- The vast majority of recommendations seem similar for most chronic conditions.
- Ultimately, exercise is fairly simple and needs to be seen as elegantly powerful.
- The complexities and nuances are matters of clinical judgment for safety's sake.
- The main concern in the chronic conditions in CDD4 is loss of independent living, which is primarily a function of light-intensity physical activities.
For these reasons, the Basic CDD4 Recommendations are consistent with but differ very slightly from the Guidelines and from the various physical activity guidelines discussed in the preceding section, because the CDD4 editors also want to make certain that sufficient attention is paid to light-intensity physical activity, especially the ability to perform instrumental activities of daily living with the goal of having patients remain independent. With these considerations in mind, the Basic CDD4 Recommendations are as follows:
- Every person with a chronic condition should be physically active, accumulating a minimum weekly total of
- 150 min of preferably moderate-intensity physical activity or, if that is too difficult, then
- 150 min of light-intensity physical activity may be substituted.
- At least 2 days per week of flexibility and muscle strengthening activities that should minimally involve
- chair sit-and-reach stretches on left and right,
- at least eight consecutive sit-to-stand exercises,
- at least 10 step-ups (or a flight of steps), leading with each foot, and
- at least eight consecutive arm curls with a minimum of 2 kg held in the hand; 4 kg is recommended.
- Individuals at risk for falls should be evaluated for causes of falls. Not all falls are caused by a condition that can be treated with exercise training. If the diagnosis of the causes suggests that exercise training can reduce the likelihood of a fall, then activities to improve balance should be incorporated into individuals' exercise regimens, under the supervision of an exercise therapist trained in fall prevention.
The higher the aerobic intensity, muscle forces, and required range of motion, the greater the likelihood of an adverse event.
These Basic CDD4 Recommendations are summarized in table 2.4. Readers should always bear in mind the goals behind the Basic CDD4 Recommendations, because these goals are helpful in drafting an individualized program to meet the unique needs of each patient. Everyone should be physically active to an extent sufficient to maintain independent living:

- Let no barrier block someone from doing light-intensity physical activity.
- Independent living requires a minimum ability to perform activities involving (or demanding)
- light-intensity aerobic work (or exertion), combined with
- strength, flexibility, and balance and coordination.
Adverse events from exercise cannot be completely eliminated, but there are two main categories to consider:
- Activity-dependent risks (due to the nature of the activity)
- Disease-dependent risks (those that relate to the pathophysiology)
The best way to minimize activity-dependent risks is to encourage the patient to practice safety precautions. If there is concern that the individual cannot do this independently, then he needs a supervised exercise program, at least to get started.
One major concern is whether or not the advice to do physical activity exposes the patient to the possibility of a disease-dependent risk. Such risks are associated with the intensity of exercise. Accordingly, if the recommendation is to complete vigorous- or high-intensity physical activities, it is prudent to follow the Guidelines on exercise testing and prescription. Most people with a chronic condition can safely participate in moderate-intensity physical activity, and if there is any concern that a particular individual cannot do so, she should either undergo some disease-specific diagnostic exercise testing or be referred to a supervised exercise program (or both).
There are few data beyond anecdotal cases to support the concern that light-intensity physical activities are likely to precipitate a disease-dependent adverse event (especially sudden death or myocardial infarction). Discerning the epidemiological role of light activities in precipitating such events would be exquisitely difficult, because participation in light-intensity activities is so ubiquitous in daily life. If someone is medically unstable to the point that activities of daily living threaten injury or death, then the Basic CDD4 Recommendations do not apply because the individual is not able to maintain independence and belongs in either a hospital or a nursing home. Indeed, it is likely that many people end up in a nursing facility sooner than they need to because no one recommended that they do light-intensity physical activity.
These nuances of safety are a key reason why an exercise professional is a necessary member of the chronic care team, because these staff are trained and have the experience to make good judgments regarding when exercise is safe and when it is not safe. See chapter 3 for a more in-depth discussion on how these judgments are made, which often involves more art than science.
Learn how to prescribe physical activity or exercise in chronic care in ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Permanent Pacemakers and Implantable Cardioverter-Defibrillators
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both.
Permanent Pacemakers
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both. In persons who have light-headedness, syncopal spells, shortness of breath, and more rarely chest pain or other cardiovascular symptoms owing to these problems, a permanent pacemaker
- improves symptoms,
- enhances exercise performance, and
- improves quality of life.
According to guidelines developed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS), class I indications for a permanent pacemaker include the following:
- Sinus node dysfunction
- Third-degree block and advanced second-degree AV block
- Hypersensitive carotid sinus syndrome
- Symptomatic bradycardia
- Sustained pause-dependent ventricular tachycardia
- Left ventricular systolic dysfunction and New York Heart Association (NYHA) functional class III or ambulatory class IV
A typical pacemaker system consists of two basic components: a pulse generator and either one or two pacing wires. In a traditional pacemaker the pacing wires are insulated and are implanted transvenously into the right atrium, right ventricle, or both. With a biventricular pacemaker, a lead is also placed in the left ventricle. The leads are connected to the pulse generator, which is typically implanted subcutaneously just below the clavicle. The two main functions of the leads are sensing and pacing. Sensing involves detecting electrical signals (i.e., P-waves and R-waves) from the heart. When these signals are not sensed at the proper timing, the pacemaker generator fires an impulse that causes the atria or ventricles (or both) to contract. Optimally, the pacing system uses an atrial and ventricular lead to maintain AV synchrony, which serves to optimize cardiac output at rest and during exercise.
Pacemakers are described by a standardized code. The first letter represents the chamber paced; the second is the chamber sensed; and the third denotes the response to a sensed event. The fourth position is used to indicate that the pacemaker has rate-response capabilities. For example, VVIR is the abbreviation used when the ventricle (V) is the chamber being paced and sensed. When the pacemaker senses a normal ventricular contraction, the pacemaker is inhibited (I). The "R" indicates that the pulse generator is rate-responsive during exercise. The response by the pacemaker is to either trigger or inhibit a pacing stimulus, depending on the absence or presence, respectively, of atrial or ventricular conduction, separately or in combination, relative to the range of heart rates that are programmed into the pacer.
A commonly used mode of pacing is the DDDR, which has dual-chamber (i.e., atrium and ventricle) pacing and inhibiting and has rate-response capability. The DDDR pacemaker is widely regarded as the optimal pacing mode in individuals who have normal sinoatrial (SA) node function, because it provides AV synchrony and uses the client's own sinus rhythm to guide ventricular stimulation. This results in a heart rate and cardiac output that, for the rest of the circulatory system, is very nearly normal.
Implantable Cardioverter-Defibrillators
An implantable cardioverter-defibrillator (ICD) is another electronic device that can be permanently implanted in individuals who either have a history of, or are at increased risk for, a life-threatening ventricular dysrhythmia. These devices impressively reduce mortality in persons with cardiomyopathy. Cardioverter-defibrillators can be just an ICD or can be a model that functions as both an ICD and a permanent pacemaker; like pacemakers, they are usually implanted subcutaneously just below the clavicle.
Implantable cardioverter-defibrillators electrically terminate life-threatening ventricular tachyarrhythmias. They consist of two basic parts: the lead system and the ICD itself. Implantable cardioverter-defibrillators have lead systems that are placed transvenously, typically by way of the subclavian vein. The ICD leads pick up the electrical rhythm of the heart and transmit this to the pulse generator, which senses the rhythm. Implantable cardioverter-defibrillators can detect atrial and ventricular arrhythmias, can provide antitachycardia pacing and defibrillation, and can be programmed with multiple protocols and the ability to record an electrocardiogram. Ventricular tachycardia (VT) and ventricular fibrillation (VF) are recognized by their rapid rates. If either VT or VF is sensed, the pulse generator delivers defibrillation or a synchronized cardioversion to terminate the rhythm. Other accelerated rhythms will initiate a pacing therapy intended to restore the rate within the preprogrammed limits.
According to guidelines developed jointly by the ACC, AHA, and HRS, class I indications for an ICD include the following:
- Survivor of cardiac arrest due to ventricular fibrillation (VF) or sustained ventricular tachycardia (VT)
- Structural heart disease with VT
- History of syncope of undetermined origin with clinically relevant VF or sustained VT induced during an electrophysiology study
- Left ventricular dysfunction due to myocardial infarction (post ≥40 days) with an ejection fraction (EF) ≤35% and NYHA class II or III or an EF ≤30% and NYHA class I
- Nonischemic dilated cardiomyopathy with an EF ≤35% and NYHA class II or III
- Nonsustained VT due to myocardial infarction with an EF ≤40% and VF or sustained VT induced during electrophysiology study
Combination Pacemaker - Defibrillator Devices
Some implantable devices are capable of providing both pacing and defibrillation. Recent evolution in terminology of pacemakers and defibrillators is toward calling them cardiac resynchronization therapy (CRT), with subclasses that provide pacing alone (CRT-P) and those that provide both pacing and defibrillation (CRT-D).
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Risk factors for coronary artery disease
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis.
Hypertension and Dyslipidemia
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis. When both conditions are present, the likelihood of having clinically significant CAD is drastically increased because atherosclerosis develops in areas of arteries that experience high blood pressure when high levels of low-density lipoprotein (LDL) are present. Because of this interrelationship and the role of exercise in mitigating these two conditions, hypertension and dyslipidemia are discussed here as linked CAD risk factors.
Basic Pathophysiology
The basic pathophysiology of these conditions is closely interrelated but is discussed separately to highlight key issues.
Hypertension
Hypertension (HTN) is a very common chronic condition, affecting about one in five people; it is defined as either
- systolic blood pressure (BP) over 139 mmHg or
- diastolic BP over 89 mmHg.
Table 6.1 has a more complete description of the classes of hypertension. High BP increases the risk for nonfatal and fatal cardiovascular disease, particularly CAD, kidney disease, and stroke. Even BP that is increased but not meeting the criteria for hypertension causes cardiovascular disease.
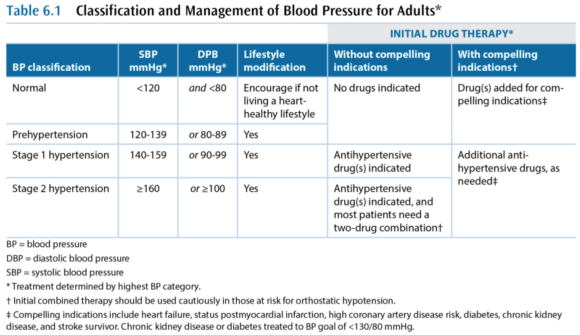
While hypertension is a common condition, the cause is not very well understood. In more than 95% of hypertension cases, the etiology is unknown and the condition is referred to as primary or essential or idiopathic hypertension. The remaining 5% of cases are secondary hypertension, so named because there is an identifiable underlying cause such as sleep apnea, drug-induced or drug-related causes (e.g., chronic corticosteroid therapy), chronic kidney disease, renovascular disease, aldosteronism, Cushing's syndrome, pheochromocytoma, coarctation of the aorta, and hyperthyroidism.
Dyslipidemia
Dyslipidemia - a high level of blood lipids - is a complex set of conditions, but the main concern is a high level of cholesterol. Cholesterol is critically important to every cell in the body, as a constituent of cell membranes that helps regulate their stability. Cholesterol is also an intermediary compound in steroid hormones, but the amount of cholesterol needed for hormones is many orders of magnitude lower than that needed for cell membranes. Cholesterol is synthesized and metabolized in the liver and then transported between the liver and the rest of the body. Cholesterol is not soluble in blood plasma and therefore has to be transported in the blood by lipoproteins. There are many different lipoproteins, each functioning to guide the cholesterol it carries to the proper metabolic pathway. This is the basic triad of lipoproteins:
- Very low-density lipoprotein (VLDL)
- Low-density lipoprotein (LDL)
- High-density lipoprotein (HDL)
The VLDL fraction carries about 80% triglycerides and 20% cholesterol, while the LDL and HDL mainly carry cholesterol. The total blood cholesterol is the sum of the cholesterol bound to VLDL, LDL, and HDL, and these cholesterol subcomponents are indicated with a -C suffix (e.g., LDL-C). Several subclassifications also exist, including two notable subclasses of LDL:
- Lipoprotein (a)
- Small dense LDL
Cholesterol metabolism is extremely complex, but the most important issue is that elevated total cholesterol and low-density lipoprotein cholesterol (LDL-C) are associated with an increased risk of CAD. Lipoprotein (a), or Lp(a), increases risk of CAD and of developing a thrombus, and small dense LDL also increases CAD risk. In contrast, high-density lipoprotein cholesterol (HDL-C) decreases CAD risk, through a cardioprotective effect that is partially related to this lipoprotein's role in the reverse cholesterol transport. In reverse transport, the cholesterol in HDL-C is transported to the liver where it is catabolized and excreted as bile.
Terms Often Used to Refer to Blood Lipids
- dyslipidemia - elevated triglycerides and cholesterol
- hypercholesterolemia - only cholesterol is elevated
- hypertriglyceridemia - only triglycerides are elevated
- exaggerated postprandial lipemia - prolonged elevation of triglycerides following consumption of dietary fat
- hyperlipoproteinemia or dyslipoproteinemia - high lipoprotein concentrations from genetic abnormalities or an underlying condition such as diabetes, renal disease, hypothyroidism, biliary obstruction, or dysproteinemia
Management and Medications
Medical management in persons who have the common chronic conditions often involves one or more medications for each condition, such that people with cardiometabolic conditions are often on five to eight prescription medicines. Again, this discussion treats these independently, but readers should expect to see multiple medications in persons in this group.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Case Study: Diabetes and Obesity with Osteoarthrosis
I intend to live into my 90s but I can’t get there unless I’m dancing. A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk.
Type 2 Diabetes and Obesity With Osteoarthrosis
Presenter: Geoffrey E. Moore, MD, FACSM
S
"I intend to live into my 90s but I can't get there unless I'm dancing."
A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk. Her recent A1c values had been 6.5-6.6, and her a.m. fasting glucose was recently 102. She qualified as T2DM by A1c criteria but wasn't working on her diet or weight and had refused to start taking metformin, and her primary care physician was increasingly concerned.
She expressed a desire to be more active through dance, which she had loved since childhood and felt was a part of her culture (having immigrated to the United States as a child). She expressed little concern about her weight and was more worried that the pain in her L shoulder kept her from dancing. She had first experienced the shoulder problem 10 years earlier while swimming backstroke. She had been to physical therapy (PT) twice, which made it worse. She also had received subacromial cortisone injections, but the relief didn't last. Her shoulder is worse at night (rolls over on her left side); the pain was rated 8/10 and was daily and constant except for sharp pain that radiated to the side of the neck when she moved the shoulder too much. She tried not to take pain or anti-inflammatory medications because she said they "wreck her stomach." Acupuncture (cupping) helped.
She also noted a history of her L knee "giving out," causing falls, and of having 2 knee arthroscopic surgeries (4 and 10 years earlier). When she overdoes weight-bearing activity, her left knee swells "like a watermelon." She did PT after the surgeries and gets to her normal daily activities but can't dance.
O
- Height: 5 ft 4¾ in. (1.65 m)
- Weight: 234.4 lb (106.3 kg)
- BMI: 39 kg/m2
- HR: 65 contractions/min
- BP: 188/98 mmHg
Pertinent Exam
- General: normal development, good nutrition, obese body habitus, no deformities
- CV: regular rhythm with normal S1 and S2, without rubs, gallops, or murmurs; distal pulses/circulation normal; no edema
- Musculoskeletal:
- Normal gait and station, muscular build especially of lower extremities
- Valgus alignment of both knees, no tenderness but the L knee has a small effusion
- Normal ROM without pain, substantial crepitus in both knees
- Left shoulder-specific tests:
- + Painful arc
- + Glenohumeral laxity, with crepitus
- + Neer test, +/- Hawkins test, +/- Speed's test
- + Painful with resisted external rotation, - pain with resisted internal rotation
- + AC joint tenderness
X Rays
- Osteoarthrosis in the acromioclavicular joint; severe osteoarthrosis in the glenohumeral joint with advanced sclerosis, subchondral cysts, and spurring; subluxed position of the humeral head at rest
Medications
- Coreg 10 mg once daily
- Diovan HCT 320/12.5 once daily
- Multivitamin once daily
A
- Increased CV risk: HTN, hyperlipidemia, diabetes by A1c criteria, sleep apnea, obesity
- Advanced glenohumeral osteoarthrosis and reduced function due to pain, status post - bilateral partial meniscectomies
Her shoulder markedly diminishes quality of life, impairing her ability to sleep and to recreate. Dance is her preferred form of physical activity, which she wants to do as her approach to improve the blood glucose and reduce her CV risk profile.
P
- L shoulder OA: refer to PT shoulder specialist
- It was explained that her shoulder would take a long time to get better, but she was likely to have some gains in reduced pain and better function after 3-6 months of PT
- Ibuprofen 500 mg every 8-12 hours and prior to bedtime as needed for pain
- Dance for exercise, but any dances that cause pain should be avoided
- Review on the difference between pain and discomfort
- High cardiovascular risk: She was not interested in addressing her cardiometabolic risk at the time of the first visit.
Goals
- Pain-free near-normal physical functioning of L shoulder
- Dance, including tango, for recreation and physical activity
- Physical therapy focused on rotator cuff and scapular stabilizer strengthening, postural control, manual therapy, and education on pain avoidance
- Gentle dancing that avoids painful arm movements started, daily for 30 min
- Dancing and daily activities to be increased as tolerated (i.e., shoulder discomfort)
Exercise Program
- Physical therapy twice weekly
- Home exercises daily, as advised by therapist
- Dancing that does not cause pain allowed as tolerated
Follow-Up
- L shoulder OA
- Pain-avoidance techniques gave rapidly improved physical functioning of L upper extremity.
- Physical therapy made good progress over 3 months to near-normal physical functioning.
- Dance for aerobic exercise was very successful in getting her motivated.
- High cardiovascular risk
After 2 months of PT, she was motivated to work on weight management and diabetes prevention. She enrolled in a partial meal-replacement lifestyle intervention plan, lost 25 lb (11.3 kg) over the subsequent 3 months, and her fasting blood glucose/A1c returned to normal.
Senior Editor's Comment
This patient's story illustrates some of the art of exercise medicine, revealing the importance of working with patients to meet their emotional expectations and needs. Her primary care team was concerned about the diabetes and had been advising her about diet, weight loss, and taking metformin, but this was less important to the patient than the loss of her ability to dance. Dancing was the only type of physical exercise she enjoyed, so she needed to be able to dance as part of her pathway to improving insulin sensitivity. Close liaison with the physical therapist facilitated the process, because the therapist provided her with tips on how to avoid painful movements and begin to dance immediately. By accepting the need to dance as her top priority and then working to help overcome her barriers to dancing, the lifestyle intervention team gained her faith in them and she began to follow their advice on diet and weight. This approach seemed unusual to many who were involved in her care, as it appeared to put the diabetes problem on hold while focusing on a painful shoulder. But from another perspective, the painful shoulder was the most important problem to the patient and thus a significant barrier that needed to be overcome if exercise (in the form of dance) was to become her most important medicine.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
A Closer Look at Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons: There are thousands of chronic conditions and causes of disability.
Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons:
- There are thousands of chronic conditions and causes of disability.
- The vast majority of recommendations seem similar for most chronic conditions.
- Ultimately, exercise is fairly simple and needs to be seen as elegantly powerful.
- The complexities and nuances are matters of clinical judgment for safety's sake.
- The main concern in the chronic conditions in CDD4 is loss of independent living, which is primarily a function of light-intensity physical activities.
For these reasons, the Basic CDD4 Recommendations are consistent with but differ very slightly from the Guidelines and from the various physical activity guidelines discussed in the preceding section, because the CDD4 editors also want to make certain that sufficient attention is paid to light-intensity physical activity, especially the ability to perform instrumental activities of daily living with the goal of having patients remain independent. With these considerations in mind, the Basic CDD4 Recommendations are as follows:
- Every person with a chronic condition should be physically active, accumulating a minimum weekly total of
- 150 min of preferably moderate-intensity physical activity or, if that is too difficult, then
- 150 min of light-intensity physical activity may be substituted.
- At least 2 days per week of flexibility and muscle strengthening activities that should minimally involve
- chair sit-and-reach stretches on left and right,
- at least eight consecutive sit-to-stand exercises,
- at least 10 step-ups (or a flight of steps), leading with each foot, and
- at least eight consecutive arm curls with a minimum of 2 kg held in the hand; 4 kg is recommended.
- Individuals at risk for falls should be evaluated for causes of falls. Not all falls are caused by a condition that can be treated with exercise training. If the diagnosis of the causes suggests that exercise training can reduce the likelihood of a fall, then activities to improve balance should be incorporated into individuals' exercise regimens, under the supervision of an exercise therapist trained in fall prevention.
The higher the aerobic intensity, muscle forces, and required range of motion, the greater the likelihood of an adverse event.
These Basic CDD4 Recommendations are summarized in table 2.4. Readers should always bear in mind the goals behind the Basic CDD4 Recommendations, because these goals are helpful in drafting an individualized program to meet the unique needs of each patient. Everyone should be physically active to an extent sufficient to maintain independent living:

- Let no barrier block someone from doing light-intensity physical activity.
- Independent living requires a minimum ability to perform activities involving (or demanding)
- light-intensity aerobic work (or exertion), combined with
- strength, flexibility, and balance and coordination.
Adverse events from exercise cannot be completely eliminated, but there are two main categories to consider:
- Activity-dependent risks (due to the nature of the activity)
- Disease-dependent risks (those that relate to the pathophysiology)
The best way to minimize activity-dependent risks is to encourage the patient to practice safety precautions. If there is concern that the individual cannot do this independently, then he needs a supervised exercise program, at least to get started.
One major concern is whether or not the advice to do physical activity exposes the patient to the possibility of a disease-dependent risk. Such risks are associated with the intensity of exercise. Accordingly, if the recommendation is to complete vigorous- or high-intensity physical activities, it is prudent to follow the Guidelines on exercise testing and prescription. Most people with a chronic condition can safely participate in moderate-intensity physical activity, and if there is any concern that a particular individual cannot do so, she should either undergo some disease-specific diagnostic exercise testing or be referred to a supervised exercise program (or both).
There are few data beyond anecdotal cases to support the concern that light-intensity physical activities are likely to precipitate a disease-dependent adverse event (especially sudden death or myocardial infarction). Discerning the epidemiological role of light activities in precipitating such events would be exquisitely difficult, because participation in light-intensity activities is so ubiquitous in daily life. If someone is medically unstable to the point that activities of daily living threaten injury or death, then the Basic CDD4 Recommendations do not apply because the individual is not able to maintain independence and belongs in either a hospital or a nursing home. Indeed, it is likely that many people end up in a nursing facility sooner than they need to because no one recommended that they do light-intensity physical activity.
These nuances of safety are a key reason why an exercise professional is a necessary member of the chronic care team, because these staff are trained and have the experience to make good judgments regarding when exercise is safe and when it is not safe. See chapter 3 for a more in-depth discussion on how these judgments are made, which often involves more art than science.
Learn how to prescribe physical activity or exercise in chronic care in ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Permanent Pacemakers and Implantable Cardioverter-Defibrillators
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both.
Permanent Pacemakers
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both. In persons who have light-headedness, syncopal spells, shortness of breath, and more rarely chest pain or other cardiovascular symptoms owing to these problems, a permanent pacemaker
- improves symptoms,
- enhances exercise performance, and
- improves quality of life.
According to guidelines developed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS), class I indications for a permanent pacemaker include the following:
- Sinus node dysfunction
- Third-degree block and advanced second-degree AV block
- Hypersensitive carotid sinus syndrome
- Symptomatic bradycardia
- Sustained pause-dependent ventricular tachycardia
- Left ventricular systolic dysfunction and New York Heart Association (NYHA) functional class III or ambulatory class IV
A typical pacemaker system consists of two basic components: a pulse generator and either one or two pacing wires. In a traditional pacemaker the pacing wires are insulated and are implanted transvenously into the right atrium, right ventricle, or both. With a biventricular pacemaker, a lead is also placed in the left ventricle. The leads are connected to the pulse generator, which is typically implanted subcutaneously just below the clavicle. The two main functions of the leads are sensing and pacing. Sensing involves detecting electrical signals (i.e., P-waves and R-waves) from the heart. When these signals are not sensed at the proper timing, the pacemaker generator fires an impulse that causes the atria or ventricles (or both) to contract. Optimally, the pacing system uses an atrial and ventricular lead to maintain AV synchrony, which serves to optimize cardiac output at rest and during exercise.
Pacemakers are described by a standardized code. The first letter represents the chamber paced; the second is the chamber sensed; and the third denotes the response to a sensed event. The fourth position is used to indicate that the pacemaker has rate-response capabilities. For example, VVIR is the abbreviation used when the ventricle (V) is the chamber being paced and sensed. When the pacemaker senses a normal ventricular contraction, the pacemaker is inhibited (I). The "R" indicates that the pulse generator is rate-responsive during exercise. The response by the pacemaker is to either trigger or inhibit a pacing stimulus, depending on the absence or presence, respectively, of atrial or ventricular conduction, separately or in combination, relative to the range of heart rates that are programmed into the pacer.
A commonly used mode of pacing is the DDDR, which has dual-chamber (i.e., atrium and ventricle) pacing and inhibiting and has rate-response capability. The DDDR pacemaker is widely regarded as the optimal pacing mode in individuals who have normal sinoatrial (SA) node function, because it provides AV synchrony and uses the client's own sinus rhythm to guide ventricular stimulation. This results in a heart rate and cardiac output that, for the rest of the circulatory system, is very nearly normal.
Implantable Cardioverter-Defibrillators
An implantable cardioverter-defibrillator (ICD) is another electronic device that can be permanently implanted in individuals who either have a history of, or are at increased risk for, a life-threatening ventricular dysrhythmia. These devices impressively reduce mortality in persons with cardiomyopathy. Cardioverter-defibrillators can be just an ICD or can be a model that functions as both an ICD and a permanent pacemaker; like pacemakers, they are usually implanted subcutaneously just below the clavicle.
Implantable cardioverter-defibrillators electrically terminate life-threatening ventricular tachyarrhythmias. They consist of two basic parts: the lead system and the ICD itself. Implantable cardioverter-defibrillators have lead systems that are placed transvenously, typically by way of the subclavian vein. The ICD leads pick up the electrical rhythm of the heart and transmit this to the pulse generator, which senses the rhythm. Implantable cardioverter-defibrillators can detect atrial and ventricular arrhythmias, can provide antitachycardia pacing and defibrillation, and can be programmed with multiple protocols and the ability to record an electrocardiogram. Ventricular tachycardia (VT) and ventricular fibrillation (VF) are recognized by their rapid rates. If either VT or VF is sensed, the pulse generator delivers defibrillation or a synchronized cardioversion to terminate the rhythm. Other accelerated rhythms will initiate a pacing therapy intended to restore the rate within the preprogrammed limits.
According to guidelines developed jointly by the ACC, AHA, and HRS, class I indications for an ICD include the following:
- Survivor of cardiac arrest due to ventricular fibrillation (VF) or sustained ventricular tachycardia (VT)
- Structural heart disease with VT
- History of syncope of undetermined origin with clinically relevant VF or sustained VT induced during an electrophysiology study
- Left ventricular dysfunction due to myocardial infarction (post ≥40 days) with an ejection fraction (EF) ≤35% and NYHA class II or III or an EF ≤30% and NYHA class I
- Nonischemic dilated cardiomyopathy with an EF ≤35% and NYHA class II or III
- Nonsustained VT due to myocardial infarction with an EF ≤40% and VF or sustained VT induced during electrophysiology study
Combination Pacemaker - Defibrillator Devices
Some implantable devices are capable of providing both pacing and defibrillation. Recent evolution in terminology of pacemakers and defibrillators is toward calling them cardiac resynchronization therapy (CRT), with subclasses that provide pacing alone (CRT-P) and those that provide both pacing and defibrillation (CRT-D).
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Risk factors for coronary artery disease
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis.
Hypertension and Dyslipidemia
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis. When both conditions are present, the likelihood of having clinically significant CAD is drastically increased because atherosclerosis develops in areas of arteries that experience high blood pressure when high levels of low-density lipoprotein (LDL) are present. Because of this interrelationship and the role of exercise in mitigating these two conditions, hypertension and dyslipidemia are discussed here as linked CAD risk factors.
Basic Pathophysiology
The basic pathophysiology of these conditions is closely interrelated but is discussed separately to highlight key issues.
Hypertension
Hypertension (HTN) is a very common chronic condition, affecting about one in five people; it is defined as either
- systolic blood pressure (BP) over 139 mmHg or
- diastolic BP over 89 mmHg.
Table 6.1 has a more complete description of the classes of hypertension. High BP increases the risk for nonfatal and fatal cardiovascular disease, particularly CAD, kidney disease, and stroke. Even BP that is increased but not meeting the criteria for hypertension causes cardiovascular disease.
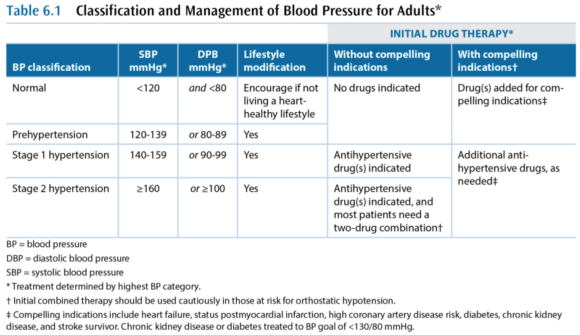
While hypertension is a common condition, the cause is not very well understood. In more than 95% of hypertension cases, the etiology is unknown and the condition is referred to as primary or essential or idiopathic hypertension. The remaining 5% of cases are secondary hypertension, so named because there is an identifiable underlying cause such as sleep apnea, drug-induced or drug-related causes (e.g., chronic corticosteroid therapy), chronic kidney disease, renovascular disease, aldosteronism, Cushing's syndrome, pheochromocytoma, coarctation of the aorta, and hyperthyroidism.
Dyslipidemia
Dyslipidemia - a high level of blood lipids - is a complex set of conditions, but the main concern is a high level of cholesterol. Cholesterol is critically important to every cell in the body, as a constituent of cell membranes that helps regulate their stability. Cholesterol is also an intermediary compound in steroid hormones, but the amount of cholesterol needed for hormones is many orders of magnitude lower than that needed for cell membranes. Cholesterol is synthesized and metabolized in the liver and then transported between the liver and the rest of the body. Cholesterol is not soluble in blood plasma and therefore has to be transported in the blood by lipoproteins. There are many different lipoproteins, each functioning to guide the cholesterol it carries to the proper metabolic pathway. This is the basic triad of lipoproteins:
- Very low-density lipoprotein (VLDL)
- Low-density lipoprotein (LDL)
- High-density lipoprotein (HDL)
The VLDL fraction carries about 80% triglycerides and 20% cholesterol, while the LDL and HDL mainly carry cholesterol. The total blood cholesterol is the sum of the cholesterol bound to VLDL, LDL, and HDL, and these cholesterol subcomponents are indicated with a -C suffix (e.g., LDL-C). Several subclassifications also exist, including two notable subclasses of LDL:
- Lipoprotein (a)
- Small dense LDL
Cholesterol metabolism is extremely complex, but the most important issue is that elevated total cholesterol and low-density lipoprotein cholesterol (LDL-C) are associated with an increased risk of CAD. Lipoprotein (a), or Lp(a), increases risk of CAD and of developing a thrombus, and small dense LDL also increases CAD risk. In contrast, high-density lipoprotein cholesterol (HDL-C) decreases CAD risk, through a cardioprotective effect that is partially related to this lipoprotein's role in the reverse cholesterol transport. In reverse transport, the cholesterol in HDL-C is transported to the liver where it is catabolized and excreted as bile.
Terms Often Used to Refer to Blood Lipids
- dyslipidemia - elevated triglycerides and cholesterol
- hypercholesterolemia - only cholesterol is elevated
- hypertriglyceridemia - only triglycerides are elevated
- exaggerated postprandial lipemia - prolonged elevation of triglycerides following consumption of dietary fat
- hyperlipoproteinemia or dyslipoproteinemia - high lipoprotein concentrations from genetic abnormalities or an underlying condition such as diabetes, renal disease, hypothyroidism, biliary obstruction, or dysproteinemia
Management and Medications
Medical management in persons who have the common chronic conditions often involves one or more medications for each condition, such that people with cardiometabolic conditions are often on five to eight prescription medicines. Again, this discussion treats these independently, but readers should expect to see multiple medications in persons in this group.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Case Study: Diabetes and Obesity with Osteoarthrosis
I intend to live into my 90s but I can’t get there unless I’m dancing. A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk.
Type 2 Diabetes and Obesity With Osteoarthrosis
Presenter: Geoffrey E. Moore, MD, FACSM
S
"I intend to live into my 90s but I can't get there unless I'm dancing."
A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk. Her recent A1c values had been 6.5-6.6, and her a.m. fasting glucose was recently 102. She qualified as T2DM by A1c criteria but wasn't working on her diet or weight and had refused to start taking metformin, and her primary care physician was increasingly concerned.
She expressed a desire to be more active through dance, which she had loved since childhood and felt was a part of her culture (having immigrated to the United States as a child). She expressed little concern about her weight and was more worried that the pain in her L shoulder kept her from dancing. She had first experienced the shoulder problem 10 years earlier while swimming backstroke. She had been to physical therapy (PT) twice, which made it worse. She also had received subacromial cortisone injections, but the relief didn't last. Her shoulder is worse at night (rolls over on her left side); the pain was rated 8/10 and was daily and constant except for sharp pain that radiated to the side of the neck when she moved the shoulder too much. She tried not to take pain or anti-inflammatory medications because she said they "wreck her stomach." Acupuncture (cupping) helped.
She also noted a history of her L knee "giving out," causing falls, and of having 2 knee arthroscopic surgeries (4 and 10 years earlier). When she overdoes weight-bearing activity, her left knee swells "like a watermelon." She did PT after the surgeries and gets to her normal daily activities but can't dance.
O
- Height: 5 ft 4¾ in. (1.65 m)
- Weight: 234.4 lb (106.3 kg)
- BMI: 39 kg/m2
- HR: 65 contractions/min
- BP: 188/98 mmHg
Pertinent Exam
- General: normal development, good nutrition, obese body habitus, no deformities
- CV: regular rhythm with normal S1 and S2, without rubs, gallops, or murmurs; distal pulses/circulation normal; no edema
- Musculoskeletal:
- Normal gait and station, muscular build especially of lower extremities
- Valgus alignment of both knees, no tenderness but the L knee has a small effusion
- Normal ROM without pain, substantial crepitus in both knees
- Left shoulder-specific tests:
- + Painful arc
- + Glenohumeral laxity, with crepitus
- + Neer test, +/- Hawkins test, +/- Speed's test
- + Painful with resisted external rotation, - pain with resisted internal rotation
- + AC joint tenderness
X Rays
- Osteoarthrosis in the acromioclavicular joint; severe osteoarthrosis in the glenohumeral joint with advanced sclerosis, subchondral cysts, and spurring; subluxed position of the humeral head at rest
Medications
- Coreg 10 mg once daily
- Diovan HCT 320/12.5 once daily
- Multivitamin once daily
A
- Increased CV risk: HTN, hyperlipidemia, diabetes by A1c criteria, sleep apnea, obesity
- Advanced glenohumeral osteoarthrosis and reduced function due to pain, status post - bilateral partial meniscectomies
Her shoulder markedly diminishes quality of life, impairing her ability to sleep and to recreate. Dance is her preferred form of physical activity, which she wants to do as her approach to improve the blood glucose and reduce her CV risk profile.
P
- L shoulder OA: refer to PT shoulder specialist
- It was explained that her shoulder would take a long time to get better, but she was likely to have some gains in reduced pain and better function after 3-6 months of PT
- Ibuprofen 500 mg every 8-12 hours and prior to bedtime as needed for pain
- Dance for exercise, but any dances that cause pain should be avoided
- Review on the difference between pain and discomfort
- High cardiovascular risk: She was not interested in addressing her cardiometabolic risk at the time of the first visit.
Goals
- Pain-free near-normal physical functioning of L shoulder
- Dance, including tango, for recreation and physical activity
- Physical therapy focused on rotator cuff and scapular stabilizer strengthening, postural control, manual therapy, and education on pain avoidance
- Gentle dancing that avoids painful arm movements started, daily for 30 min
- Dancing and daily activities to be increased as tolerated (i.e., shoulder discomfort)
Exercise Program
- Physical therapy twice weekly
- Home exercises daily, as advised by therapist
- Dancing that does not cause pain allowed as tolerated
Follow-Up
- L shoulder OA
- Pain-avoidance techniques gave rapidly improved physical functioning of L upper extremity.
- Physical therapy made good progress over 3 months to near-normal physical functioning.
- Dance for aerobic exercise was very successful in getting her motivated.
- High cardiovascular risk
After 2 months of PT, she was motivated to work on weight management and diabetes prevention. She enrolled in a partial meal-replacement lifestyle intervention plan, lost 25 lb (11.3 kg) over the subsequent 3 months, and her fasting blood glucose/A1c returned to normal.
Senior Editor's Comment
This patient's story illustrates some of the art of exercise medicine, revealing the importance of working with patients to meet their emotional expectations and needs. Her primary care team was concerned about the diabetes and had been advising her about diet, weight loss, and taking metformin, but this was less important to the patient than the loss of her ability to dance. Dancing was the only type of physical exercise she enjoyed, so she needed to be able to dance as part of her pathway to improving insulin sensitivity. Close liaison with the physical therapist facilitated the process, because the therapist provided her with tips on how to avoid painful movements and begin to dance immediately. By accepting the need to dance as her top priority and then working to help overcome her barriers to dancing, the lifestyle intervention team gained her faith in them and she began to follow their advice on diet and weight. This approach seemed unusual to many who were involved in her care, as it appeared to put the diabetes problem on hold while focusing on a painful shoulder. But from another perspective, the painful shoulder was the most important problem to the patient and thus a significant barrier that needed to be overcome if exercise (in the form of dance) was to become her most important medicine.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
A Closer Look at Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons: There are thousands of chronic conditions and causes of disability.
Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons:
- There are thousands of chronic conditions and causes of disability.
- The vast majority of recommendations seem similar for most chronic conditions.
- Ultimately, exercise is fairly simple and needs to be seen as elegantly powerful.
- The complexities and nuances are matters of clinical judgment for safety's sake.
- The main concern in the chronic conditions in CDD4 is loss of independent living, which is primarily a function of light-intensity physical activities.
For these reasons, the Basic CDD4 Recommendations are consistent with but differ very slightly from the Guidelines and from the various physical activity guidelines discussed in the preceding section, because the CDD4 editors also want to make certain that sufficient attention is paid to light-intensity physical activity, especially the ability to perform instrumental activities of daily living with the goal of having patients remain independent. With these considerations in mind, the Basic CDD4 Recommendations are as follows:
- Every person with a chronic condition should be physically active, accumulating a minimum weekly total of
- 150 min of preferably moderate-intensity physical activity or, if that is too difficult, then
- 150 min of light-intensity physical activity may be substituted.
- At least 2 days per week of flexibility and muscle strengthening activities that should minimally involve
- chair sit-and-reach stretches on left and right,
- at least eight consecutive sit-to-stand exercises,
- at least 10 step-ups (or a flight of steps), leading with each foot, and
- at least eight consecutive arm curls with a minimum of 2 kg held in the hand; 4 kg is recommended.
- Individuals at risk for falls should be evaluated for causes of falls. Not all falls are caused by a condition that can be treated with exercise training. If the diagnosis of the causes suggests that exercise training can reduce the likelihood of a fall, then activities to improve balance should be incorporated into individuals' exercise regimens, under the supervision of an exercise therapist trained in fall prevention.
The higher the aerobic intensity, muscle forces, and required range of motion, the greater the likelihood of an adverse event.
These Basic CDD4 Recommendations are summarized in table 2.4. Readers should always bear in mind the goals behind the Basic CDD4 Recommendations, because these goals are helpful in drafting an individualized program to meet the unique needs of each patient. Everyone should be physically active to an extent sufficient to maintain independent living:

- Let no barrier block someone from doing light-intensity physical activity.
- Independent living requires a minimum ability to perform activities involving (or demanding)
- light-intensity aerobic work (or exertion), combined with
- strength, flexibility, and balance and coordination.
Adverse events from exercise cannot be completely eliminated, but there are two main categories to consider:
- Activity-dependent risks (due to the nature of the activity)
- Disease-dependent risks (those that relate to the pathophysiology)
The best way to minimize activity-dependent risks is to encourage the patient to practice safety precautions. If there is concern that the individual cannot do this independently, then he needs a supervised exercise program, at least to get started.
One major concern is whether or not the advice to do physical activity exposes the patient to the possibility of a disease-dependent risk. Such risks are associated with the intensity of exercise. Accordingly, if the recommendation is to complete vigorous- or high-intensity physical activities, it is prudent to follow the Guidelines on exercise testing and prescription. Most people with a chronic condition can safely participate in moderate-intensity physical activity, and if there is any concern that a particular individual cannot do so, she should either undergo some disease-specific diagnostic exercise testing or be referred to a supervised exercise program (or both).
There are few data beyond anecdotal cases to support the concern that light-intensity physical activities are likely to precipitate a disease-dependent adverse event (especially sudden death or myocardial infarction). Discerning the epidemiological role of light activities in precipitating such events would be exquisitely difficult, because participation in light-intensity activities is so ubiquitous in daily life. If someone is medically unstable to the point that activities of daily living threaten injury or death, then the Basic CDD4 Recommendations do not apply because the individual is not able to maintain independence and belongs in either a hospital or a nursing home. Indeed, it is likely that many people end up in a nursing facility sooner than they need to because no one recommended that they do light-intensity physical activity.
These nuances of safety are a key reason why an exercise professional is a necessary member of the chronic care team, because these staff are trained and have the experience to make good judgments regarding when exercise is safe and when it is not safe. See chapter 3 for a more in-depth discussion on how these judgments are made, which often involves more art than science.
Learn how to prescribe physical activity or exercise in chronic care in ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Permanent Pacemakers and Implantable Cardioverter-Defibrillators
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both.
Permanent Pacemakers
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both. In persons who have light-headedness, syncopal spells, shortness of breath, and more rarely chest pain or other cardiovascular symptoms owing to these problems, a permanent pacemaker
- improves symptoms,
- enhances exercise performance, and
- improves quality of life.
According to guidelines developed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS), class I indications for a permanent pacemaker include the following:
- Sinus node dysfunction
- Third-degree block and advanced second-degree AV block
- Hypersensitive carotid sinus syndrome
- Symptomatic bradycardia
- Sustained pause-dependent ventricular tachycardia
- Left ventricular systolic dysfunction and New York Heart Association (NYHA) functional class III or ambulatory class IV
A typical pacemaker system consists of two basic components: a pulse generator and either one or two pacing wires. In a traditional pacemaker the pacing wires are insulated and are implanted transvenously into the right atrium, right ventricle, or both. With a biventricular pacemaker, a lead is also placed in the left ventricle. The leads are connected to the pulse generator, which is typically implanted subcutaneously just below the clavicle. The two main functions of the leads are sensing and pacing. Sensing involves detecting electrical signals (i.e., P-waves and R-waves) from the heart. When these signals are not sensed at the proper timing, the pacemaker generator fires an impulse that causes the atria or ventricles (or both) to contract. Optimally, the pacing system uses an atrial and ventricular lead to maintain AV synchrony, which serves to optimize cardiac output at rest and during exercise.
Pacemakers are described by a standardized code. The first letter represents the chamber paced; the second is the chamber sensed; and the third denotes the response to a sensed event. The fourth position is used to indicate that the pacemaker has rate-response capabilities. For example, VVIR is the abbreviation used when the ventricle (V) is the chamber being paced and sensed. When the pacemaker senses a normal ventricular contraction, the pacemaker is inhibited (I). The "R" indicates that the pulse generator is rate-responsive during exercise. The response by the pacemaker is to either trigger or inhibit a pacing stimulus, depending on the absence or presence, respectively, of atrial or ventricular conduction, separately or in combination, relative to the range of heart rates that are programmed into the pacer.
A commonly used mode of pacing is the DDDR, which has dual-chamber (i.e., atrium and ventricle) pacing and inhibiting and has rate-response capability. The DDDR pacemaker is widely regarded as the optimal pacing mode in individuals who have normal sinoatrial (SA) node function, because it provides AV synchrony and uses the client's own sinus rhythm to guide ventricular stimulation. This results in a heart rate and cardiac output that, for the rest of the circulatory system, is very nearly normal.
Implantable Cardioverter-Defibrillators
An implantable cardioverter-defibrillator (ICD) is another electronic device that can be permanently implanted in individuals who either have a history of, or are at increased risk for, a life-threatening ventricular dysrhythmia. These devices impressively reduce mortality in persons with cardiomyopathy. Cardioverter-defibrillators can be just an ICD or can be a model that functions as both an ICD and a permanent pacemaker; like pacemakers, they are usually implanted subcutaneously just below the clavicle.
Implantable cardioverter-defibrillators electrically terminate life-threatening ventricular tachyarrhythmias. They consist of two basic parts: the lead system and the ICD itself. Implantable cardioverter-defibrillators have lead systems that are placed transvenously, typically by way of the subclavian vein. The ICD leads pick up the electrical rhythm of the heart and transmit this to the pulse generator, which senses the rhythm. Implantable cardioverter-defibrillators can detect atrial and ventricular arrhythmias, can provide antitachycardia pacing and defibrillation, and can be programmed with multiple protocols and the ability to record an electrocardiogram. Ventricular tachycardia (VT) and ventricular fibrillation (VF) are recognized by their rapid rates. If either VT or VF is sensed, the pulse generator delivers defibrillation or a synchronized cardioversion to terminate the rhythm. Other accelerated rhythms will initiate a pacing therapy intended to restore the rate within the preprogrammed limits.
According to guidelines developed jointly by the ACC, AHA, and HRS, class I indications for an ICD include the following:
- Survivor of cardiac arrest due to ventricular fibrillation (VF) or sustained ventricular tachycardia (VT)
- Structural heart disease with VT
- History of syncope of undetermined origin with clinically relevant VF or sustained VT induced during an electrophysiology study
- Left ventricular dysfunction due to myocardial infarction (post ≥40 days) with an ejection fraction (EF) ≤35% and NYHA class II or III or an EF ≤30% and NYHA class I
- Nonischemic dilated cardiomyopathy with an EF ≤35% and NYHA class II or III
- Nonsustained VT due to myocardial infarction with an EF ≤40% and VF or sustained VT induced during electrophysiology study
Combination Pacemaker - Defibrillator Devices
Some implantable devices are capable of providing both pacing and defibrillation. Recent evolution in terminology of pacemakers and defibrillators is toward calling them cardiac resynchronization therapy (CRT), with subclasses that provide pacing alone (CRT-P) and those that provide both pacing and defibrillation (CRT-D).
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Risk factors for coronary artery disease
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis.
Hypertension and Dyslipidemia
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis. When both conditions are present, the likelihood of having clinically significant CAD is drastically increased because atherosclerosis develops in areas of arteries that experience high blood pressure when high levels of low-density lipoprotein (LDL) are present. Because of this interrelationship and the role of exercise in mitigating these two conditions, hypertension and dyslipidemia are discussed here as linked CAD risk factors.
Basic Pathophysiology
The basic pathophysiology of these conditions is closely interrelated but is discussed separately to highlight key issues.
Hypertension
Hypertension (HTN) is a very common chronic condition, affecting about one in five people; it is defined as either
- systolic blood pressure (BP) over 139 mmHg or
- diastolic BP over 89 mmHg.
Table 6.1 has a more complete description of the classes of hypertension. High BP increases the risk for nonfatal and fatal cardiovascular disease, particularly CAD, kidney disease, and stroke. Even BP that is increased but not meeting the criteria for hypertension causes cardiovascular disease.
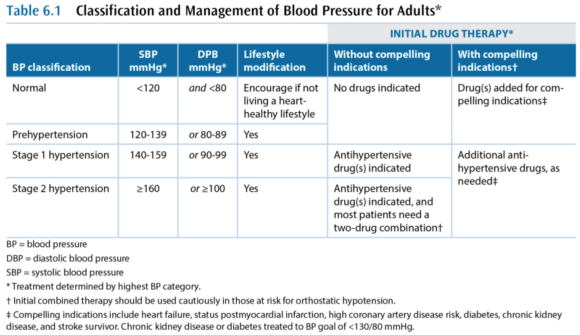
While hypertension is a common condition, the cause is not very well understood. In more than 95% of hypertension cases, the etiology is unknown and the condition is referred to as primary or essential or idiopathic hypertension. The remaining 5% of cases are secondary hypertension, so named because there is an identifiable underlying cause such as sleep apnea, drug-induced or drug-related causes (e.g., chronic corticosteroid therapy), chronic kidney disease, renovascular disease, aldosteronism, Cushing's syndrome, pheochromocytoma, coarctation of the aorta, and hyperthyroidism.
Dyslipidemia
Dyslipidemia - a high level of blood lipids - is a complex set of conditions, but the main concern is a high level of cholesterol. Cholesterol is critically important to every cell in the body, as a constituent of cell membranes that helps regulate their stability. Cholesterol is also an intermediary compound in steroid hormones, but the amount of cholesterol needed for hormones is many orders of magnitude lower than that needed for cell membranes. Cholesterol is synthesized and metabolized in the liver and then transported between the liver and the rest of the body. Cholesterol is not soluble in blood plasma and therefore has to be transported in the blood by lipoproteins. There are many different lipoproteins, each functioning to guide the cholesterol it carries to the proper metabolic pathway. This is the basic triad of lipoproteins:
- Very low-density lipoprotein (VLDL)
- Low-density lipoprotein (LDL)
- High-density lipoprotein (HDL)
The VLDL fraction carries about 80% triglycerides and 20% cholesterol, while the LDL and HDL mainly carry cholesterol. The total blood cholesterol is the sum of the cholesterol bound to VLDL, LDL, and HDL, and these cholesterol subcomponents are indicated with a -C suffix (e.g., LDL-C). Several subclassifications also exist, including two notable subclasses of LDL:
- Lipoprotein (a)
- Small dense LDL
Cholesterol metabolism is extremely complex, but the most important issue is that elevated total cholesterol and low-density lipoprotein cholesterol (LDL-C) are associated with an increased risk of CAD. Lipoprotein (a), or Lp(a), increases risk of CAD and of developing a thrombus, and small dense LDL also increases CAD risk. In contrast, high-density lipoprotein cholesterol (HDL-C) decreases CAD risk, through a cardioprotective effect that is partially related to this lipoprotein's role in the reverse cholesterol transport. In reverse transport, the cholesterol in HDL-C is transported to the liver where it is catabolized and excreted as bile.
Terms Often Used to Refer to Blood Lipids
- dyslipidemia - elevated triglycerides and cholesterol
- hypercholesterolemia - only cholesterol is elevated
- hypertriglyceridemia - only triglycerides are elevated
- exaggerated postprandial lipemia - prolonged elevation of triglycerides following consumption of dietary fat
- hyperlipoproteinemia or dyslipoproteinemia - high lipoprotein concentrations from genetic abnormalities or an underlying condition such as diabetes, renal disease, hypothyroidism, biliary obstruction, or dysproteinemia
Management and Medications
Medical management in persons who have the common chronic conditions often involves one or more medications for each condition, such that people with cardiometabolic conditions are often on five to eight prescription medicines. Again, this discussion treats these independently, but readers should expect to see multiple medications in persons in this group.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Case Study: Diabetes and Obesity with Osteoarthrosis
I intend to live into my 90s but I can’t get there unless I’m dancing. A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk.
Type 2 Diabetes and Obesity With Osteoarthrosis
Presenter: Geoffrey E. Moore, MD, FACSM
S
"I intend to live into my 90s but I can't get there unless I'm dancing."
A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk. Her recent A1c values had been 6.5-6.6, and her a.m. fasting glucose was recently 102. She qualified as T2DM by A1c criteria but wasn't working on her diet or weight and had refused to start taking metformin, and her primary care physician was increasingly concerned.
She expressed a desire to be more active through dance, which she had loved since childhood and felt was a part of her culture (having immigrated to the United States as a child). She expressed little concern about her weight and was more worried that the pain in her L shoulder kept her from dancing. She had first experienced the shoulder problem 10 years earlier while swimming backstroke. She had been to physical therapy (PT) twice, which made it worse. She also had received subacromial cortisone injections, but the relief didn't last. Her shoulder is worse at night (rolls over on her left side); the pain was rated 8/10 and was daily and constant except for sharp pain that radiated to the side of the neck when she moved the shoulder too much. She tried not to take pain or anti-inflammatory medications because she said they "wreck her stomach." Acupuncture (cupping) helped.
She also noted a history of her L knee "giving out," causing falls, and of having 2 knee arthroscopic surgeries (4 and 10 years earlier). When she overdoes weight-bearing activity, her left knee swells "like a watermelon." She did PT after the surgeries and gets to her normal daily activities but can't dance.
O
- Height: 5 ft 4¾ in. (1.65 m)
- Weight: 234.4 lb (106.3 kg)
- BMI: 39 kg/m2
- HR: 65 contractions/min
- BP: 188/98 mmHg
Pertinent Exam
- General: normal development, good nutrition, obese body habitus, no deformities
- CV: regular rhythm with normal S1 and S2, without rubs, gallops, or murmurs; distal pulses/circulation normal; no edema
- Musculoskeletal:
- Normal gait and station, muscular build especially of lower extremities
- Valgus alignment of both knees, no tenderness but the L knee has a small effusion
- Normal ROM without pain, substantial crepitus in both knees
- Left shoulder-specific tests:
- + Painful arc
- + Glenohumeral laxity, with crepitus
- + Neer test, +/- Hawkins test, +/- Speed's test
- + Painful with resisted external rotation, - pain with resisted internal rotation
- + AC joint tenderness
X Rays
- Osteoarthrosis in the acromioclavicular joint; severe osteoarthrosis in the glenohumeral joint with advanced sclerosis, subchondral cysts, and spurring; subluxed position of the humeral head at rest
Medications
- Coreg 10 mg once daily
- Diovan HCT 320/12.5 once daily
- Multivitamin once daily
A
- Increased CV risk: HTN, hyperlipidemia, diabetes by A1c criteria, sleep apnea, obesity
- Advanced glenohumeral osteoarthrosis and reduced function due to pain, status post - bilateral partial meniscectomies
Her shoulder markedly diminishes quality of life, impairing her ability to sleep and to recreate. Dance is her preferred form of physical activity, which she wants to do as her approach to improve the blood glucose and reduce her CV risk profile.
P
- L shoulder OA: refer to PT shoulder specialist
- It was explained that her shoulder would take a long time to get better, but she was likely to have some gains in reduced pain and better function after 3-6 months of PT
- Ibuprofen 500 mg every 8-12 hours and prior to bedtime as needed for pain
- Dance for exercise, but any dances that cause pain should be avoided
- Review on the difference between pain and discomfort
- High cardiovascular risk: She was not interested in addressing her cardiometabolic risk at the time of the first visit.
Goals
- Pain-free near-normal physical functioning of L shoulder
- Dance, including tango, for recreation and physical activity
- Physical therapy focused on rotator cuff and scapular stabilizer strengthening, postural control, manual therapy, and education on pain avoidance
- Gentle dancing that avoids painful arm movements started, daily for 30 min
- Dancing and daily activities to be increased as tolerated (i.e., shoulder discomfort)
Exercise Program
- Physical therapy twice weekly
- Home exercises daily, as advised by therapist
- Dancing that does not cause pain allowed as tolerated
Follow-Up
- L shoulder OA
- Pain-avoidance techniques gave rapidly improved physical functioning of L upper extremity.
- Physical therapy made good progress over 3 months to near-normal physical functioning.
- Dance for aerobic exercise was very successful in getting her motivated.
- High cardiovascular risk
After 2 months of PT, she was motivated to work on weight management and diabetes prevention. She enrolled in a partial meal-replacement lifestyle intervention plan, lost 25 lb (11.3 kg) over the subsequent 3 months, and her fasting blood glucose/A1c returned to normal.
Senior Editor's Comment
This patient's story illustrates some of the art of exercise medicine, revealing the importance of working with patients to meet their emotional expectations and needs. Her primary care team was concerned about the diabetes and had been advising her about diet, weight loss, and taking metformin, but this was less important to the patient than the loss of her ability to dance. Dancing was the only type of physical exercise she enjoyed, so she needed to be able to dance as part of her pathway to improving insulin sensitivity. Close liaison with the physical therapist facilitated the process, because the therapist provided her with tips on how to avoid painful movements and begin to dance immediately. By accepting the need to dance as her top priority and then working to help overcome her barriers to dancing, the lifestyle intervention team gained her faith in them and she began to follow their advice on diet and weight. This approach seemed unusual to many who were involved in her care, as it appeared to put the diabetes problem on hold while focusing on a painful shoulder. But from another perspective, the painful shoulder was the most important problem to the patient and thus a significant barrier that needed to be overcome if exercise (in the form of dance) was to become her most important medicine.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
A Closer Look at Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons: There are thousands of chronic conditions and causes of disability.
Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons:
- There are thousands of chronic conditions and causes of disability.
- The vast majority of recommendations seem similar for most chronic conditions.
- Ultimately, exercise is fairly simple and needs to be seen as elegantly powerful.
- The complexities and nuances are matters of clinical judgment for safety's sake.
- The main concern in the chronic conditions in CDD4 is loss of independent living, which is primarily a function of light-intensity physical activities.
For these reasons, the Basic CDD4 Recommendations are consistent with but differ very slightly from the Guidelines and from the various physical activity guidelines discussed in the preceding section, because the CDD4 editors also want to make certain that sufficient attention is paid to light-intensity physical activity, especially the ability to perform instrumental activities of daily living with the goal of having patients remain independent. With these considerations in mind, the Basic CDD4 Recommendations are as follows:
- Every person with a chronic condition should be physically active, accumulating a minimum weekly total of
- 150 min of preferably moderate-intensity physical activity or, if that is too difficult, then
- 150 min of light-intensity physical activity may be substituted.
- At least 2 days per week of flexibility and muscle strengthening activities that should minimally involve
- chair sit-and-reach stretches on left and right,
- at least eight consecutive sit-to-stand exercises,
- at least 10 step-ups (or a flight of steps), leading with each foot, and
- at least eight consecutive arm curls with a minimum of 2 kg held in the hand; 4 kg is recommended.
- Individuals at risk for falls should be evaluated for causes of falls. Not all falls are caused by a condition that can be treated with exercise training. If the diagnosis of the causes suggests that exercise training can reduce the likelihood of a fall, then activities to improve balance should be incorporated into individuals' exercise regimens, under the supervision of an exercise therapist trained in fall prevention.
The higher the aerobic intensity, muscle forces, and required range of motion, the greater the likelihood of an adverse event.
These Basic CDD4 Recommendations are summarized in table 2.4. Readers should always bear in mind the goals behind the Basic CDD4 Recommendations, because these goals are helpful in drafting an individualized program to meet the unique needs of each patient. Everyone should be physically active to an extent sufficient to maintain independent living:

- Let no barrier block someone from doing light-intensity physical activity.
- Independent living requires a minimum ability to perform activities involving (or demanding)
- light-intensity aerobic work (or exertion), combined with
- strength, flexibility, and balance and coordination.
Adverse events from exercise cannot be completely eliminated, but there are two main categories to consider:
- Activity-dependent risks (due to the nature of the activity)
- Disease-dependent risks (those that relate to the pathophysiology)
The best way to minimize activity-dependent risks is to encourage the patient to practice safety precautions. If there is concern that the individual cannot do this independently, then he needs a supervised exercise program, at least to get started.
One major concern is whether or not the advice to do physical activity exposes the patient to the possibility of a disease-dependent risk. Such risks are associated with the intensity of exercise. Accordingly, if the recommendation is to complete vigorous- or high-intensity physical activities, it is prudent to follow the Guidelines on exercise testing and prescription. Most people with a chronic condition can safely participate in moderate-intensity physical activity, and if there is any concern that a particular individual cannot do so, she should either undergo some disease-specific diagnostic exercise testing or be referred to a supervised exercise program (or both).
There are few data beyond anecdotal cases to support the concern that light-intensity physical activities are likely to precipitate a disease-dependent adverse event (especially sudden death or myocardial infarction). Discerning the epidemiological role of light activities in precipitating such events would be exquisitely difficult, because participation in light-intensity activities is so ubiquitous in daily life. If someone is medically unstable to the point that activities of daily living threaten injury or death, then the Basic CDD4 Recommendations do not apply because the individual is not able to maintain independence and belongs in either a hospital or a nursing home. Indeed, it is likely that many people end up in a nursing facility sooner than they need to because no one recommended that they do light-intensity physical activity.
These nuances of safety are a key reason why an exercise professional is a necessary member of the chronic care team, because these staff are trained and have the experience to make good judgments regarding when exercise is safe and when it is not safe. See chapter 3 for a more in-depth discussion on how these judgments are made, which often involves more art than science.
Learn how to prescribe physical activity or exercise in chronic care in ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Permanent Pacemakers and Implantable Cardioverter-Defibrillators
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both.
Permanent Pacemakers
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both. In persons who have light-headedness, syncopal spells, shortness of breath, and more rarely chest pain or other cardiovascular symptoms owing to these problems, a permanent pacemaker
- improves symptoms,
- enhances exercise performance, and
- improves quality of life.
According to guidelines developed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS), class I indications for a permanent pacemaker include the following:
- Sinus node dysfunction
- Third-degree block and advanced second-degree AV block
- Hypersensitive carotid sinus syndrome
- Symptomatic bradycardia
- Sustained pause-dependent ventricular tachycardia
- Left ventricular systolic dysfunction and New York Heart Association (NYHA) functional class III or ambulatory class IV
A typical pacemaker system consists of two basic components: a pulse generator and either one or two pacing wires. In a traditional pacemaker the pacing wires are insulated and are implanted transvenously into the right atrium, right ventricle, or both. With a biventricular pacemaker, a lead is also placed in the left ventricle. The leads are connected to the pulse generator, which is typically implanted subcutaneously just below the clavicle. The two main functions of the leads are sensing and pacing. Sensing involves detecting electrical signals (i.e., P-waves and R-waves) from the heart. When these signals are not sensed at the proper timing, the pacemaker generator fires an impulse that causes the atria or ventricles (or both) to contract. Optimally, the pacing system uses an atrial and ventricular lead to maintain AV synchrony, which serves to optimize cardiac output at rest and during exercise.
Pacemakers are described by a standardized code. The first letter represents the chamber paced; the second is the chamber sensed; and the third denotes the response to a sensed event. The fourth position is used to indicate that the pacemaker has rate-response capabilities. For example, VVIR is the abbreviation used when the ventricle (V) is the chamber being paced and sensed. When the pacemaker senses a normal ventricular contraction, the pacemaker is inhibited (I). The "R" indicates that the pulse generator is rate-responsive during exercise. The response by the pacemaker is to either trigger or inhibit a pacing stimulus, depending on the absence or presence, respectively, of atrial or ventricular conduction, separately or in combination, relative to the range of heart rates that are programmed into the pacer.
A commonly used mode of pacing is the DDDR, which has dual-chamber (i.e., atrium and ventricle) pacing and inhibiting and has rate-response capability. The DDDR pacemaker is widely regarded as the optimal pacing mode in individuals who have normal sinoatrial (SA) node function, because it provides AV synchrony and uses the client's own sinus rhythm to guide ventricular stimulation. This results in a heart rate and cardiac output that, for the rest of the circulatory system, is very nearly normal.
Implantable Cardioverter-Defibrillators
An implantable cardioverter-defibrillator (ICD) is another electronic device that can be permanently implanted in individuals who either have a history of, or are at increased risk for, a life-threatening ventricular dysrhythmia. These devices impressively reduce mortality in persons with cardiomyopathy. Cardioverter-defibrillators can be just an ICD or can be a model that functions as both an ICD and a permanent pacemaker; like pacemakers, they are usually implanted subcutaneously just below the clavicle.
Implantable cardioverter-defibrillators electrically terminate life-threatening ventricular tachyarrhythmias. They consist of two basic parts: the lead system and the ICD itself. Implantable cardioverter-defibrillators have lead systems that are placed transvenously, typically by way of the subclavian vein. The ICD leads pick up the electrical rhythm of the heart and transmit this to the pulse generator, which senses the rhythm. Implantable cardioverter-defibrillators can detect atrial and ventricular arrhythmias, can provide antitachycardia pacing and defibrillation, and can be programmed with multiple protocols and the ability to record an electrocardiogram. Ventricular tachycardia (VT) and ventricular fibrillation (VF) are recognized by their rapid rates. If either VT or VF is sensed, the pulse generator delivers defibrillation or a synchronized cardioversion to terminate the rhythm. Other accelerated rhythms will initiate a pacing therapy intended to restore the rate within the preprogrammed limits.
According to guidelines developed jointly by the ACC, AHA, and HRS, class I indications for an ICD include the following:
- Survivor of cardiac arrest due to ventricular fibrillation (VF) or sustained ventricular tachycardia (VT)
- Structural heart disease with VT
- History of syncope of undetermined origin with clinically relevant VF or sustained VT induced during an electrophysiology study
- Left ventricular dysfunction due to myocardial infarction (post ≥40 days) with an ejection fraction (EF) ≤35% and NYHA class II or III or an EF ≤30% and NYHA class I
- Nonischemic dilated cardiomyopathy with an EF ≤35% and NYHA class II or III
- Nonsustained VT due to myocardial infarction with an EF ≤40% and VF or sustained VT induced during electrophysiology study
Combination Pacemaker - Defibrillator Devices
Some implantable devices are capable of providing both pacing and defibrillation. Recent evolution in terminology of pacemakers and defibrillators is toward calling them cardiac resynchronization therapy (CRT), with subclasses that provide pacing alone (CRT-P) and those that provide both pacing and defibrillation (CRT-D).
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Risk factors for coronary artery disease
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis.
Hypertension and Dyslipidemia
Hypertension and dyslipidemia are separate independent risk factors for coronary artery disease (CAD), and in the United States, 33% of Americans have dyslipidemia and 29% have hypertension. These diseases frequently occur together, however, and the combination speeds the process of atherosclerosis. When both conditions are present, the likelihood of having clinically significant CAD is drastically increased because atherosclerosis develops in areas of arteries that experience high blood pressure when high levels of low-density lipoprotein (LDL) are present. Because of this interrelationship and the role of exercise in mitigating these two conditions, hypertension and dyslipidemia are discussed here as linked CAD risk factors.
Basic Pathophysiology
The basic pathophysiology of these conditions is closely interrelated but is discussed separately to highlight key issues.
Hypertension
Hypertension (HTN) is a very common chronic condition, affecting about one in five people; it is defined as either
- systolic blood pressure (BP) over 139 mmHg or
- diastolic BP over 89 mmHg.
Table 6.1 has a more complete description of the classes of hypertension. High BP increases the risk for nonfatal and fatal cardiovascular disease, particularly CAD, kidney disease, and stroke. Even BP that is increased but not meeting the criteria for hypertension causes cardiovascular disease.
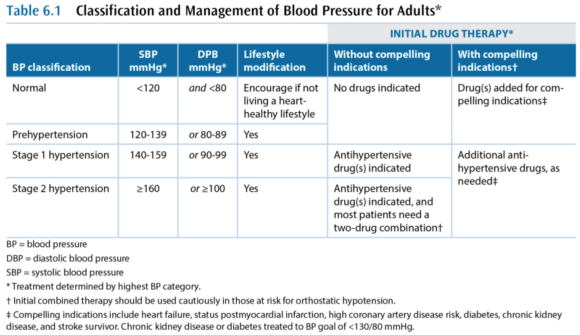
While hypertension is a common condition, the cause is not very well understood. In more than 95% of hypertension cases, the etiology is unknown and the condition is referred to as primary or essential or idiopathic hypertension. The remaining 5% of cases are secondary hypertension, so named because there is an identifiable underlying cause such as sleep apnea, drug-induced or drug-related causes (e.g., chronic corticosteroid therapy), chronic kidney disease, renovascular disease, aldosteronism, Cushing's syndrome, pheochromocytoma, coarctation of the aorta, and hyperthyroidism.
Dyslipidemia
Dyslipidemia - a high level of blood lipids - is a complex set of conditions, but the main concern is a high level of cholesterol. Cholesterol is critically important to every cell in the body, as a constituent of cell membranes that helps regulate their stability. Cholesterol is also an intermediary compound in steroid hormones, but the amount of cholesterol needed for hormones is many orders of magnitude lower than that needed for cell membranes. Cholesterol is synthesized and metabolized in the liver and then transported between the liver and the rest of the body. Cholesterol is not soluble in blood plasma and therefore has to be transported in the blood by lipoproteins. There are many different lipoproteins, each functioning to guide the cholesterol it carries to the proper metabolic pathway. This is the basic triad of lipoproteins:
- Very low-density lipoprotein (VLDL)
- Low-density lipoprotein (LDL)
- High-density lipoprotein (HDL)
The VLDL fraction carries about 80% triglycerides and 20% cholesterol, while the LDL and HDL mainly carry cholesterol. The total blood cholesterol is the sum of the cholesterol bound to VLDL, LDL, and HDL, and these cholesterol subcomponents are indicated with a -C suffix (e.g., LDL-C). Several subclassifications also exist, including two notable subclasses of LDL:
- Lipoprotein (a)
- Small dense LDL
Cholesterol metabolism is extremely complex, but the most important issue is that elevated total cholesterol and low-density lipoprotein cholesterol (LDL-C) are associated with an increased risk of CAD. Lipoprotein (a), or Lp(a), increases risk of CAD and of developing a thrombus, and small dense LDL also increases CAD risk. In contrast, high-density lipoprotein cholesterol (HDL-C) decreases CAD risk, through a cardioprotective effect that is partially related to this lipoprotein's role in the reverse cholesterol transport. In reverse transport, the cholesterol in HDL-C is transported to the liver where it is catabolized and excreted as bile.
Terms Often Used to Refer to Blood Lipids
- dyslipidemia - elevated triglycerides and cholesterol
- hypercholesterolemia - only cholesterol is elevated
- hypertriglyceridemia - only triglycerides are elevated
- exaggerated postprandial lipemia - prolonged elevation of triglycerides following consumption of dietary fat
- hyperlipoproteinemia or dyslipoproteinemia - high lipoprotein concentrations from genetic abnormalities or an underlying condition such as diabetes, renal disease, hypothyroidism, biliary obstruction, or dysproteinemia
Management and Medications
Medical management in persons who have the common chronic conditions often involves one or more medications for each condition, such that people with cardiometabolic conditions are often on five to eight prescription medicines. Again, this discussion treats these independently, but readers should expect to see multiple medications in persons in this group.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Case Study: Diabetes and Obesity with Osteoarthrosis
I intend to live into my 90s but I can’t get there unless I’m dancing. A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk.
Type 2 Diabetes and Obesity With Osteoarthrosis
Presenter: Geoffrey E. Moore, MD, FACSM
S
"I intend to live into my 90s but I can't get there unless I'm dancing."
A 52-year-old woman with type 2 diabetes was referred for help on lifestyle. She had a family history of diabetes and tended toward a centripetal/abdominal fat distribution pattern associated with high CV risk. Her recent A1c values had been 6.5-6.6, and her a.m. fasting glucose was recently 102. She qualified as T2DM by A1c criteria but wasn't working on her diet or weight and had refused to start taking metformin, and her primary care physician was increasingly concerned.
She expressed a desire to be more active through dance, which she had loved since childhood and felt was a part of her culture (having immigrated to the United States as a child). She expressed little concern about her weight and was more worried that the pain in her L shoulder kept her from dancing. She had first experienced the shoulder problem 10 years earlier while swimming backstroke. She had been to physical therapy (PT) twice, which made it worse. She also had received subacromial cortisone injections, but the relief didn't last. Her shoulder is worse at night (rolls over on her left side); the pain was rated 8/10 and was daily and constant except for sharp pain that radiated to the side of the neck when she moved the shoulder too much. She tried not to take pain or anti-inflammatory medications because she said they "wreck her stomach." Acupuncture (cupping) helped.
She also noted a history of her L knee "giving out," causing falls, and of having 2 knee arthroscopic surgeries (4 and 10 years earlier). When she overdoes weight-bearing activity, her left knee swells "like a watermelon." She did PT after the surgeries and gets to her normal daily activities but can't dance.
O
- Height: 5 ft 4¾ in. (1.65 m)
- Weight: 234.4 lb (106.3 kg)
- BMI: 39 kg/m2
- HR: 65 contractions/min
- BP: 188/98 mmHg
Pertinent Exam
- General: normal development, good nutrition, obese body habitus, no deformities
- CV: regular rhythm with normal S1 and S2, without rubs, gallops, or murmurs; distal pulses/circulation normal; no edema
- Musculoskeletal:
- Normal gait and station, muscular build especially of lower extremities
- Valgus alignment of both knees, no tenderness but the L knee has a small effusion
- Normal ROM without pain, substantial crepitus in both knees
- Left shoulder-specific tests:
- + Painful arc
- + Glenohumeral laxity, with crepitus
- + Neer test, +/- Hawkins test, +/- Speed's test
- + Painful with resisted external rotation, - pain with resisted internal rotation
- + AC joint tenderness
X Rays
- Osteoarthrosis in the acromioclavicular joint; severe osteoarthrosis in the glenohumeral joint with advanced sclerosis, subchondral cysts, and spurring; subluxed position of the humeral head at rest
Medications
- Coreg 10 mg once daily
- Diovan HCT 320/12.5 once daily
- Multivitamin once daily
A
- Increased CV risk: HTN, hyperlipidemia, diabetes by A1c criteria, sleep apnea, obesity
- Advanced glenohumeral osteoarthrosis and reduced function due to pain, status post - bilateral partial meniscectomies
Her shoulder markedly diminishes quality of life, impairing her ability to sleep and to recreate. Dance is her preferred form of physical activity, which she wants to do as her approach to improve the blood glucose and reduce her CV risk profile.
P
- L shoulder OA: refer to PT shoulder specialist
- It was explained that her shoulder would take a long time to get better, but she was likely to have some gains in reduced pain and better function after 3-6 months of PT
- Ibuprofen 500 mg every 8-12 hours and prior to bedtime as needed for pain
- Dance for exercise, but any dances that cause pain should be avoided
- Review on the difference between pain and discomfort
- High cardiovascular risk: She was not interested in addressing her cardiometabolic risk at the time of the first visit.
Goals
- Pain-free near-normal physical functioning of L shoulder
- Dance, including tango, for recreation and physical activity
- Physical therapy focused on rotator cuff and scapular stabilizer strengthening, postural control, manual therapy, and education on pain avoidance
- Gentle dancing that avoids painful arm movements started, daily for 30 min
- Dancing and daily activities to be increased as tolerated (i.e., shoulder discomfort)
Exercise Program
- Physical therapy twice weekly
- Home exercises daily, as advised by therapist
- Dancing that does not cause pain allowed as tolerated
Follow-Up
- L shoulder OA
- Pain-avoidance techniques gave rapidly improved physical functioning of L upper extremity.
- Physical therapy made good progress over 3 months to near-normal physical functioning.
- Dance for aerobic exercise was very successful in getting her motivated.
- High cardiovascular risk
After 2 months of PT, she was motivated to work on weight management and diabetes prevention. She enrolled in a partial meal-replacement lifestyle intervention plan, lost 25 lb (11.3 kg) over the subsequent 3 months, and her fasting blood glucose/A1c returned to normal.
Senior Editor's Comment
This patient's story illustrates some of the art of exercise medicine, revealing the importance of working with patients to meet their emotional expectations and needs. Her primary care team was concerned about the diabetes and had been advising her about diet, weight loss, and taking metformin, but this was less important to the patient than the loss of her ability to dance. Dancing was the only type of physical exercise she enjoyed, so she needed to be able to dance as part of her pathway to improving insulin sensitivity. Close liaison with the physical therapist facilitated the process, because the therapist provided her with tips on how to avoid painful movements and begin to dance immediately. By accepting the need to dance as her top priority and then working to help overcome her barriers to dancing, the lifestyle intervention team gained her faith in them and she began to follow their advice on diet and weight. This approach seemed unusual to many who were involved in her care, as it appeared to put the diabetes problem on hold while focusing on a painful shoulder. But from another perspective, the painful shoulder was the most important problem to the patient and thus a significant barrier that needed to be overcome if exercise (in the form of dance) was to become her most important medicine.
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
A Closer Look at Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons: There are thousands of chronic conditions and causes of disability.
Basic CDD4 Recommendations for Physical Activity or Exercise in Chronic Conditions
After four editions of the CDD series, with many decades of clinical experience on the part of the contributors to CDD4, the main working group of authors concluded that it is confusing and unnecessary to sustain disease-specific recommendations, for these reasons:
- There are thousands of chronic conditions and causes of disability.
- The vast majority of recommendations seem similar for most chronic conditions.
- Ultimately, exercise is fairly simple and needs to be seen as elegantly powerful.
- The complexities and nuances are matters of clinical judgment for safety's sake.
- The main concern in the chronic conditions in CDD4 is loss of independent living, which is primarily a function of light-intensity physical activities.
For these reasons, the Basic CDD4 Recommendations are consistent with but differ very slightly from the Guidelines and from the various physical activity guidelines discussed in the preceding section, because the CDD4 editors also want to make certain that sufficient attention is paid to light-intensity physical activity, especially the ability to perform instrumental activities of daily living with the goal of having patients remain independent. With these considerations in mind, the Basic CDD4 Recommendations are as follows:
- Every person with a chronic condition should be physically active, accumulating a minimum weekly total of
- 150 min of preferably moderate-intensity physical activity or, if that is too difficult, then
- 150 min of light-intensity physical activity may be substituted.
- At least 2 days per week of flexibility and muscle strengthening activities that should minimally involve
- chair sit-and-reach stretches on left and right,
- at least eight consecutive sit-to-stand exercises,
- at least 10 step-ups (or a flight of steps), leading with each foot, and
- at least eight consecutive arm curls with a minimum of 2 kg held in the hand; 4 kg is recommended.
- Individuals at risk for falls should be evaluated for causes of falls. Not all falls are caused by a condition that can be treated with exercise training. If the diagnosis of the causes suggests that exercise training can reduce the likelihood of a fall, then activities to improve balance should be incorporated into individuals' exercise regimens, under the supervision of an exercise therapist trained in fall prevention.
The higher the aerobic intensity, muscle forces, and required range of motion, the greater the likelihood of an adverse event.
These Basic CDD4 Recommendations are summarized in table 2.4. Readers should always bear in mind the goals behind the Basic CDD4 Recommendations, because these goals are helpful in drafting an individualized program to meet the unique needs of each patient. Everyone should be physically active to an extent sufficient to maintain independent living:

- Let no barrier block someone from doing light-intensity physical activity.
- Independent living requires a minimum ability to perform activities involving (or demanding)
- light-intensity aerobic work (or exertion), combined with
- strength, flexibility, and balance and coordination.
Adverse events from exercise cannot be completely eliminated, but there are two main categories to consider:
- Activity-dependent risks (due to the nature of the activity)
- Disease-dependent risks (those that relate to the pathophysiology)
The best way to minimize activity-dependent risks is to encourage the patient to practice safety precautions. If there is concern that the individual cannot do this independently, then he needs a supervised exercise program, at least to get started.
One major concern is whether or not the advice to do physical activity exposes the patient to the possibility of a disease-dependent risk. Such risks are associated with the intensity of exercise. Accordingly, if the recommendation is to complete vigorous- or high-intensity physical activities, it is prudent to follow the Guidelines on exercise testing and prescription. Most people with a chronic condition can safely participate in moderate-intensity physical activity, and if there is any concern that a particular individual cannot do so, she should either undergo some disease-specific diagnostic exercise testing or be referred to a supervised exercise program (or both).
There are few data beyond anecdotal cases to support the concern that light-intensity physical activities are likely to precipitate a disease-dependent adverse event (especially sudden death or myocardial infarction). Discerning the epidemiological role of light activities in precipitating such events would be exquisitely difficult, because participation in light-intensity activities is so ubiquitous in daily life. If someone is medically unstable to the point that activities of daily living threaten injury or death, then the Basic CDD4 Recommendations do not apply because the individual is not able to maintain independence and belongs in either a hospital or a nursing home. Indeed, it is likely that many people end up in a nursing facility sooner than they need to because no one recommended that they do light-intensity physical activity.
These nuances of safety are a key reason why an exercise professional is a necessary member of the chronic care team, because these staff are trained and have the experience to make good judgments regarding when exercise is safe and when it is not safe. See chapter 3 for a more in-depth discussion on how these judgments are made, which often involves more art than science.
Learn how to prescribe physical activity or exercise in chronic care in ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.
Permanent Pacemakers and Implantable Cardioverter-Defibrillators
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both.
Permanent Pacemakers
A variety of factors contribute to optimal cardiac functioning, including atrioventricular (AV) synchronization and the chronotropic and inotropic responses to neurohormonal stimuli. Alterations in the normal sequence of atrial and ventricular filling and contraction can result in deterioration of hemodynamics and subsequent symptoms at rest, during exercise, or both. In persons who have light-headedness, syncopal spells, shortness of breath, and more rarely chest pain or other cardiovascular symptoms owing to these problems, a permanent pacemaker
- improves symptoms,
- enhances exercise performance, and
- improves quality of life.
According to guidelines developed jointly by the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Rhythm Society (HRS), class I indications for a permanent pacemaker include the following:
- Sinus node dysfunction
- Third-degree block and advanced second-degree AV block
- Hypersensitive carotid sinus syndrome
- Symptomatic bradycardia
- Sustained pause-dependent ventricular tachycardia
- Left ventricular systolic dysfunction and New York Heart Association (NYHA) functional class III or ambulatory class IV
A typical pacemaker system consists of two basic components: a pulse generator and either one or two pacing wires. In a traditional pacemaker the pacing wires are insulated and are implanted transvenously into the right atrium, right ventricle, or both. With a biventricular pacemaker, a lead is also placed in the left ventricle. The leads are connected to the pulse generator, which is typically implanted subcutaneously just below the clavicle. The two main functions of the leads are sensing and pacing. Sensing involves detecting electrical signals (i.e., P-waves and R-waves) from the heart. When these signals are not sensed at the proper timing, the pacemaker generator fires an impulse that causes the atria or ventricles (or both) to contract. Optimally, the pacing system uses an atrial and ventricular lead to maintain AV synchrony, which serves to optimize cardiac output at rest and during exercise.
Pacemakers are described by a standardized code. The first letter represents the chamber paced; the second is the chamber sensed; and the third denotes the response to a sensed event. The fourth position is used to indicate that the pacemaker has rate-response capabilities. For example, VVIR is the abbreviation used when the ventricle (V) is the chamber being paced and sensed. When the pacemaker senses a normal ventricular contraction, the pacemaker is inhibited (I). The "R" indicates that the pulse generator is rate-responsive during exercise. The response by the pacemaker is to either trigger or inhibit a pacing stimulus, depending on the absence or presence, respectively, of atrial or ventricular conduction, separately or in combination, relative to the range of heart rates that are programmed into the pacer.
A commonly used mode of pacing is the DDDR, which has dual-chamber (i.e., atrium and ventricle) pacing and inhibiting and has rate-response capability. The DDDR pacemaker is widely regarded as the optimal pacing mode in individuals who have normal sinoatrial (SA) node function, because it provides AV synchrony and uses the client's own sinus rhythm to guide ventricular stimulation. This results in a heart rate and cardiac output that, for the rest of the circulatory system, is very nearly normal.
Implantable Cardioverter-Defibrillators
An implantable cardioverter-defibrillator (ICD) is another electronic device that can be permanently implanted in individuals who either have a history of, or are at increased risk for, a life-threatening ventricular dysrhythmia. These devices impressively reduce mortality in persons with cardiomyopathy. Cardioverter-defibrillators can be just an ICD or can be a model that functions as both an ICD and a permanent pacemaker; like pacemakers, they are usually implanted subcutaneously just below the clavicle.
Implantable cardioverter-defibrillators electrically terminate life-threatening ventricular tachyarrhythmias. They consist of two basic parts: the lead system and the ICD itself. Implantable cardioverter-defibrillators have lead systems that are placed transvenously, typically by way of the subclavian vein. The ICD leads pick up the electrical rhythm of the heart and transmit this to the pulse generator, which senses the rhythm. Implantable cardioverter-defibrillators can detect atrial and ventricular arrhythmias, can provide antitachycardia pacing and defibrillation, and can be programmed with multiple protocols and the ability to record an electrocardiogram. Ventricular tachycardia (VT) and ventricular fibrillation (VF) are recognized by their rapid rates. If either VT or VF is sensed, the pulse generator delivers defibrillation or a synchronized cardioversion to terminate the rhythm. Other accelerated rhythms will initiate a pacing therapy intended to restore the rate within the preprogrammed limits.
According to guidelines developed jointly by the ACC, AHA, and HRS, class I indications for an ICD include the following:
- Survivor of cardiac arrest due to ventricular fibrillation (VF) or sustained ventricular tachycardia (VT)
- Structural heart disease with VT
- History of syncope of undetermined origin with clinically relevant VF or sustained VT induced during an electrophysiology study
- Left ventricular dysfunction due to myocardial infarction (post ≥40 days) with an ejection fraction (EF) ≤35% and NYHA class II or III or an EF ≤30% and NYHA class I
- Nonischemic dilated cardiomyopathy with an EF ≤35% and NYHA class II or III
- Nonsustained VT due to myocardial infarction with an EF ≤40% and VF or sustained VT induced during electrophysiology study
Combination Pacemaker - Defibrillator Devices
Some implantable devices are capable of providing both pacing and defibrillation. Recent evolution in terminology of pacemakers and defibrillators is toward calling them cardiac resynchronization therapy (CRT), with subclasses that provide pacing alone (CRT-P) and those that provide both pacing and defibrillation (CRT-D).
Learn more about ACSM's Exercise Management for Persons With Chronic Diseases and Disabilities, Fourth Edition.