- Home
- Track and Field (Athletics)
- Medicine in Exercise and Sport
- Health Care in Exercise and Sport
- Cardiopulmonary Rehabilitation
- Athletic Training and Therapy
- Acute and Emergency Care in Athletic Training
Authors Michelle Cleary and Katie Walsh Flanagan take an interdisciplinary approach, drawing from literature, position statements, and guidelines from numerous professional health care organizations to offer current evidence-based clinical best practices. The book’s comprehensive coverage adheres to and incorporates guidelines from the Commission on Accreditation of Athletic Training Education (CAATE) and the Board of Certification (BOC), and it is one of the first textbooks to align with the competencies outlined in the CAATE 2020 standards.
To prepare students to effectively provide appropriate care before getting an injured or ill athlete to the hospital, Acute and Emergency Care in Athletic Training includes the following learning aids:
- Case studies in the web study guide offer practical scenarios that will facilitate critical thinking and decision-making skills.
- Clinical Skills sidebars guide students through the process of completing specific tasks such as splinting, wound care, and airway maintenance.
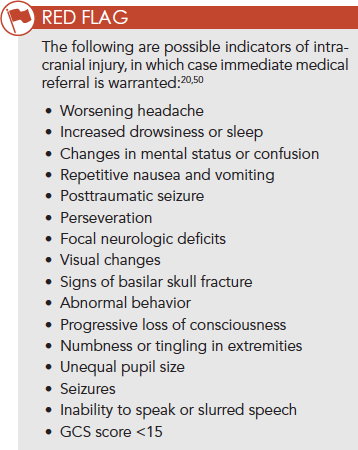
- Red Flag sidebars indicate areas where significant caution is warranted.
- Decision-making algorithms and decision trees lead students through selecting the most appropriate treatment option based on a patient’s signs and symptoms.
- Key terms are boldfaced in the text and are defined in the glossary section.
With a full-color presentation and more than 280 photos and illustrations, the text takes a systematic approach to acute and emergency care, with the content divided into two parts. Part I provides critical information on prevention and risk management strategies, including developing an emergency action plan, conducting an emergency examination, and administering emergency medications. Part II then provides the basics of emergency evaluations, describing how to examine, treat, and manage common acute injuries and illnesses to limit the severity of these potentially life-threatening conditions.
To aid instructors using Acute and Emergency Care in Athletic Training in the classroom, there is a full array of ancillaries, including a test package, an instructor guide with sample answers to the case study questions, and a presentation package plus image bank.
When an athlete is injured on the field of play, time is of the essence. Acute and Emergency Care in Athletic Training is an invaluable resource for training and preparing the initial responders to recognize critical situations and treat the acutely injured or ill patient.
Chapter 1. The Interprofessional Health Care Team
Characteristics of a Good Team
Sports Medicine Setting
Breakdowns in Teamwork
Effective Practices in Teamwork
Professional Attributes of Effective Health Care Providers
Therapeutic Behaviors
Summary
Chapter 2. Prevention and Risk Management Strategies
Risk Management
Infectious Diseases
Standard Precautions
Exposure Control Plans
Legal Responsibility
Summary
Chapter 3. Planning for Emergencies
Epidemiology of Medical Emergencies in Sports
Emergency Planning in Sports
Developing an Emergency Action Plan for Each Venue
Developing Acute Care and Emergency Protocols for Major Trauma and Medical Emergencies
Consulting With Institutional Authorities and Working With Local EMS Providers
Obtaining and Maintaining Emergency Equipment and Supplies
Review the EAP and Training Personnel
Communicating During an Emergency
Mass Care and Catastrophic Incidents
Post-Catastrophic Injury or Post-Critical Incident Plan
Evidence for Best Practices in Emergency Preparedness
Summary
Chapter 4. The Emergency Examination
Scene Size-Up
Initial Assessment
Identify the Chief Complaint or Concern
Focused Assessment
Monitoring the Critically Injured or Ill Patient
Reassessment
Patient Hand-Off
Evidence for Injury Scoring Systems
Summary
Chapter 5. Emergency Medications and Administration
Medical Direction and Oversight
Best Practices for Safe Administration of Medication
Medication Administration
Oral Medication Administration
Sublingual Medication Administration
Metered-Dose Inhaler Administration
Oxygen Administration
Nebulized Medication Administration
Emergency Medication Injection
Intravenous Access
Summary
Part II. Immediate Management of Acute Injuries and Illnesses
Chapter 6. Immediate Management of Bleeding, Shock, and Immunologic Emergencies
Overview of the Circulatory System
Hemorrhage
Shock
Anaphylactic Reactions and Immunologic Emergencies
Evidence
Summary
Chapter 7. Immediate Management of Musculoskeletal Injuries
Overview of the Structures
Classification of Injuries
Shoulder Dislocation
Elbow Dislocation
Finger Dislocation
Hip Dislocation
Knee Dislocation
Ankle Dislocation
Humeral Fractures
Colles’ Fracture
Pelvis Fracture
Femur Fracture
Tibia-Fibula Fractures
Ankle Fractures
Management of Lower-Leg Fractures
Compartment Syndrome
Ring Avulsion
Summary
Chapter 8. Traumatic Injuries to the Head and Face
Overview of the Head and Face
Overview of Head Injuries
Scalp Lacerations
Skull Fracture
Concussion
Chronic Traumatic Encephalopathy
Intracranial Pressure
Intracerebral Contusion
Epidural Hematoma
Subdural Hematoma
Headaches
Stroke
Seizures
Altered Mental Status
Overview of Facial Injuries
Corneal Abrasion and Foreign Objects in the Eye
Retinal Detachment
Hyphema
Tympanic Membrane Rupture
Facial Fractures
Temporomandibular Joint Dislocation
Dental Injuries
Laryngeal Injuries
Summary
Chapter 9. Traumatic Injuries to the Spine
Anatomy and Physiology of the Spine
Pathophysiology
Emergency Medical Care of Injuries to the Spine
Equipment Removal
Summary
Chapter 10. Injuries of the Thorax and Lungs
Overview of Anatomical Structures in the Thorax
Respiratory Assessment
Using Supplemental Oxygen
Airway Maintenance
Rib Fracture
Sternoclavicular Joint Injury
Pulmonary Embolism
Pneumothorax, Hemothorax, and Hemopneumothorax
Asthma
Summary
Chapter 11. Life-Threatening Cardiac Conditions
Overview of the Cardiovascular System
Epidemiology of Sudden Cardiac Death
Etiology and Pathophysiology of Acute Cardiac Conditions
Field Assessment Techniques for Emergent Cardiac Conditions
Immediate Management of Sudden Cardiac Arrest
Emergency Preparedness for Sudden Cardiac Arrest
Clinical Decision Making
Evidence: Cardiovascular Screening
Evidence: Factors Affecting Survival After Sudden Cardiac Arrest
Summary
Chapter 12. Injuries and Illnesses of the Abdominopelvic Region
Overview of Anatomical Structures in the Abdomen and Pelvis
Trauma to Abdominal Organs
Injuries to the Liver and Spleen
Injury to the Kidneys
Appendicitis
Acute Abdominopelvic Concerns for Female Athletes
Acute Trauma to Male Genitals
Summary
Chapter 13. Life-Threatening Metabolic Emergencies
Overview of the Anatomical Structures in Metabolic Emergencies
Diabetes
Hypoglycemia and Hyperglycemia
Summary
Chapter 14. Exertional Sickling and Rhabdomyolysis
Exertional Rhabdomyolysis
Sickle Cell Trait
Evidence: Factors That Increase Risk of Exertional Rhabdomyolysis
Summary
Chapter 15. Environmental Emergencies
Lightning Emergencies
Heat-Related Emergencies
Cold-Related Emergencies
Altitude-Related Emergencies
Summary
Appendix A. Model Exposure Control Plan
Appendix B. SCAT-5
Michelle A. Cleary, PhD, ATC, CSCS, is an associate professor in the athletic training program and an associate dean of graduate health science at Chapman University. Prior to joining Chapman in 2012, Cleary taught at Temple University, where she earned her doctorate, and at Florida International University and the University of Hawaii. She is certified as an athletic trainer by the Board of Certification (BOC) and is certified as a strength and conditioning specialist by the National Strength and Conditioning Association. She is the chair of the Research and Grants Committee of the Far West Athletic Trainers’ Association and is also a member of the American College of Sports Medicine. Cleary’s primary research interests focus on heat-related illness and injury and other sport safety issues. In addition to numerous journal articles and book chapters, Cleary has written two national position statements for the National Athletic Trainers’ Association (NATA). Her clinical experience includes time as an athletic trainer at the high school, NCAA Division I, and international/Olympic levels.
Katie Walsh Flanagan, EdD, ATC, is a professor and director of the sports medicine and athletic training program in the department of health education and promotion at East Carolina University, where she has worked for more than 20 years, and is an athletic trainer certified by the Board of Certification (BOC). Walsh Flanagan previously worked as a lecturer and assistant athletic trainer at California State University, Fresno, and as the head athletic trainer for the Chicago Power, a men’s professional soccer team. She has also assisted as an athletic trainer for various sports in international competitions, including the 1996 Summer Olympic Games and 1987 Pan American Games.
In 2012, Walsh Flanagan was elected to the North Carolina Athletic Trainers’ Association Hall of Fame. The organization named her the North Carolina College/University Athletic Trainer of the Year in 2000 and 2006. She received the National Athletic Trainers’ Association (NATA) Most Distinguished Athletic Trainer Award in 2010 and NATA’s Service Award in 2006. In 2017, she was named a NATA board member as the director of District Three. She coauthored Medical Conditions in the Athlete, Third Edition.
Sternoclavicular joint injury
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton.
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton. This joint is a loose connection between the medial clavicle and manubrium of the superior sternum. It has a joint capsule, disc, and several ligaments in addition to the SC ligament—the intraclavicular ligament (between the two medial aspects of the clavicle, superior to the sternum) and the costoclavicular ligament, which maintains the stability of the clavicle on the ribs below. The SC joint is inherently unstable, and only a portion of the clavicle actually articulates with the manubrium, relying on the SC ligament to provide more stability.
Injury to the SC joint is one of the true medical emergencies in orthopedics. Just posterior to the joint lie the trachea and carotid arteries, and not too lateral from there, the subclavian arteries are located (figure 10.12). A posterior subluxation or dislocation can be a life-threatening emergency with compression on any of these structures.
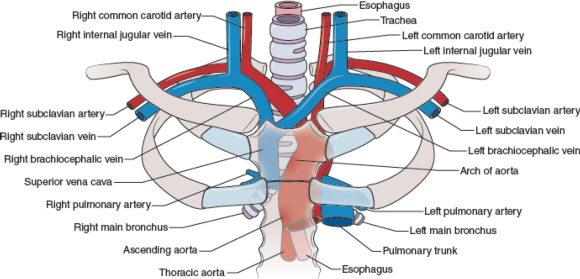
Figure 10.12 Internal structures behind the sternoclavicular (SC) joint.
Because of the SC's importance in connecting the arm to the body proper, the SC joint has many MOIs. One can fall on an outstretched hand or elbow, and the force can transmit along the bones of the arm, acromion of the scapula, and clavicle to the joint, injuring it. Another MOI is a fall on the lateral aspect of the shoulder (humerus or acromion of the scapula), or lying on one side with a pileup on the opposite lateral shoulder. In both of these situations, the force is transmitted along from the humerus/acromion to the clavicle and on to the biomechanically weakest aspect. The athlete could sprain the acromioclavicular joint or fracture the clavicle, or the force could continue medially and injure the SC joint at the sternum.
Incidence and Epidemiology
Injury to the sternoclavicular joint is rare, and posterior dislocations are more unusual. In a study of 251 SC dislocations, only 80 were posterior dislocations. Of the total number of dislocations (both anterior and posterior), the average age of the patient was 29 years old, and 67% of them were male.5 These data are consistent in other publications, in that younger males are more likely to sustain SC injuries than are other age groups or women.6
Risk Factors
Risk factors for injuring the SC joint include falling on an outstretched arm, elbow, or lateral shoulder. As noted, men under 30 years old tend to have higher incidences of SC injuries, so that population is at higher risk. Because high-velocity contact is a MOI, motor vehicle accidents are also a means of sustaining this injury.
Signs and Symptoms
When evaluating an injury to the upper extremity, it is important to be aware of the anatomical connection of the upper extremity and the SC joint. The athlete may initially feel more soreness at the point of impact (e.g., hand, elbow, shoulder) and not recognize the injury to the SC joint. Appreciating the MOI for a potential transmitted force to the medial clavicle and sternum is critical.
On inspection, a deformity may be present over the medial clavicle. It can range from mild swelling to gross deformity. A divot at the SC junction may indicate a posterior dislocation or subluxation, or a posterior fracture of the medial clavicular head (depending on the age of the athlete). Palpation results in a painful SC ligament or joint. Crepitus indicates a fracture, not dislocation or subluxation, but it is equally disconcerting.
Joint stress testing is not recommended, but sometimes the athlete presents with pain away from the SC joint, and that specific injury is not considered at the initial time of testing. The patient will present with an unwillingness to demonstrate full glenohumeral range of motion, because the stress on that joint affects the SC joint.
In a true posterior SC dislocation or subluxation, the patient may have dyspnea or hoarseness and relate difficulty swallowing, because the trachea is pushing posteriorly into the esophagus. If any of these complaints occur, consider it a medical emergency and transport via ambulance as soon as possible. On occasion, the patient will not identify the difficulty swallowing and hoarseness as related to the falling injury, and may not report these conditions. Anecdotal conversations with ATs indicate that athletes sometimes delay reporting issues of the voice or swallowing because they do not relate it to the SC sprain injury, only to have it be an emergency hours later when swelling increases and the airway begins to be compromised.
Field Assessment Techniques
Always assume a potential SC injury when presented with a mechanism consistent with the biomechanical weakness of the joint. Palpate all aspects of the clavicle, SC joint, and manubrium when evaluating falls resulting in landing on the outstretched hand, olecranon of the elbow, or acromion of scapula. If injury to the SC joint is suspected, assess airway and quality of voice. Ask the athlete to swallow, and query whether that action feels normal. Patients with swelling over the SC joint, who report that it is hard to swallow, or who have altered breath sounds, anxiety, or hoarseness should be removed from activity, have their shoulder pads removed (if wearing them), and be transported to the emergency department via ambulance. While waiting for transport, keep the athlete sitting up to facilitate breathing, and apply a sling to the affected arm. The sling will prevent unnecessary movement of the SC joint.
Reduction of the sternoclavicular joint is not recommended on the field. This procedure is performed under sedation or general anesthesia in an operating room. Open reduction and possible stabilization are necessary in situations of failed closed reduction or ongoing symptoms.7 Typically, surgical reduction of this injury is performed in conjunction with a cardiothoracic surgeon because of the potential for complications external to orthopedic surgery.
Diagnostic Accuracy
Standard radiographs of the SC joint are ineffective, because the X-rays are poor at viewing relevant anatomy of the joint.7 One technique that does provide better viewing is the serendipity view, which allows a 40° cephalic tilt.7 In this technique, an anterior dislocation presents as a superiorly displaced medial clavicle, and a posterior dislocation is represented as an inferiorly displaced medial clavicle.7 The preferred imaging is CT, which clearly defines the vascular and respiratory features that could be compromised.
Immediate Management Techniques
If the patient reports no difficulty with breathing or swallowing, but has swelling or tenderness over the SC joint, remove the patient from activity, place the affected arm in a sling, and reassess often. In this situation, ice may be held in place by the patient for 15- to 20-minute intervals if it relieves pain and swelling.
Indications
Dyspnea, hoarseness, or dysphagia following a collision or fall on an out stretched arm, elbow, or lateral shoulder are indications to transport the athlete via ambulance to the nearest ED.
Contraindications
Applying ice to the SC region after an acute injury may be contraindicated for a few reasons. The weight of the ice itself could put additional pressure on an unstable joint, further aggravating any dyspnea. Using a wrap to secure the ice to the area provides additional pressure to the area, which can actually worsen an unstable SC joint injury. The anatomical positioning of the trachea and major vessels from the heart immediately under the thin skin of the neck make ice an inappropriate treatment.
Criteria for Deciding to Transport for Further Medical Examination
Dyspnea, hoarseness, and difficulty swallowing following a collision or fall on an outstretched arm, elbow, or lateral shoulder are indications to transport the patient via ambulance to the nearest emergency department.
Transportation Techniques
Patients with a suspected posterior SC sprain should have supplemental oxygen available delivered via a nasal cannula. Transportation should occur in a recumbent position to facilitate easier respiration. A sling should be placed on the affected arm to relieve any traction of the SC joint from the weight of the upper extremity.
Heat-related emergencies in athletes
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS).
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS). EHS is the only true heat-related life-threatening emergency, and it is the only heat illness discussed here. As the name suggests, EHS is brought about by the combination of exertion (working out), temperature (including air and humidity), and other factors. A person can acclimate to the hot weather if given the time and cautiously increasing the activity duration slowly in the hot environment. Heatstroke is preventable in many aspects, including paying close attention to the weather (air temperature, ambient temperature, humidity, wind, sunshine), the heat and humidity trends in the local area, clothing and equipment worn, work-to-rest ratio, and hydration and food intake.13 Other salient factors include medical conditions, body mass, poor conditioning, medications, prior history of heat illness, and other predispositions that can exacerbate heat illness.14
Incidence and Epidemiology
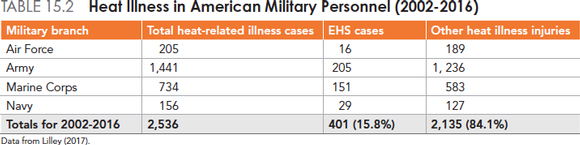
Although the overall risk of EHS is low, its consequences can be fatal. According to the National Center for Catastrophic Sport Injury Research, 148 deaths have occurred since 1955 (56 since 1996) due to EHS in football.17 Rates are highest across all levels of football (youth, high school, and collegiate) during the preseason and lower during youth practices and high school games.18 Athletics are not alone in EHS injury; the U.S. military forces also have significant data. Fort Benning, Georgia and Fort Bragg, North Carolina led a 14-year study period with over 1,400 heat-related illnesses each, and nearly 3,500 incidents were reported from military bases in North and South Carolina combined (table 15.2).19
Medical Consequences
of Heatstroke
The systemic physiological effects of untreated EHS are many. The rising internal temperature denatures proteins and cellular membranes, causing an inflammatory response.20 As a reaction, the body relocates an aspect of bacteria usually found in the gastrointestinal system, which can promulgate a sepsis reaction systemically, and therefore begins a coagulation reaction throughout organs.20 Aside from death, EHS can elicit multi-organ failure, acute respiratory distress syndrome, and coma. Organ failure can become irreversible and the long-term sequelae catastrophic.
Signs and Symptoms
If the weather is hot or humid, be suspicious of EHS for any athlete who presents with any of these signs of symptoms. The 2 cardinal signs of EHS are a rectal temperature over 105°F (40.5°C) and central nervous system dysfunction, namely, concussion-like behaviors.21 Strictly from an observational standpoint, the athlete may be disoriented, confused, or dizzy, and his performance may be deteriorating. EHS patients tend to have diaphoretic and hot skin. The presence or absence of sweat should not be a deterrent to consider EHS, given other feedback. Complaints of muscular cramping, headache, weakness, or dry mouth are worth continued exploration. Nausea, vomiting, or diarrhea can occur prior to
collapse.14,20-23
Sudden collapse, seizure, altered consciousness, or coma can occur and will likely transpire if not rapidly diagnosed and treated.21,22 Vital signs can diminish with time, especially if the patient is untreated.
Field Assessment Techniques
A person who has heatstroke presents with concussion-like symptoms, which include confusion, stupor, dizziness, personality changes, and acting combative or complacent. A rapid decision must be made to assess core temperature using a rectal thermometer to diagnose EHS (figure 15.1). Every minute delay to diagnose EHS via rectal thermometry is critical.
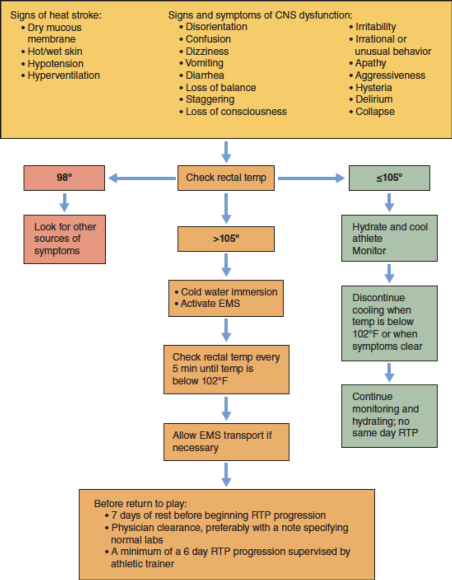
Figure 15.1 Decision tree for EHS.
Safe helmet removal after spinal injury
If the decision has been made to remove the athlete’s equipment, the helmet and shoulder pads should be considered a unit and both be removed.
If the decision has been made to remove the athlete's equipment, the helmet and shoulder pads should be considered a unit and both be removed. Once the face mask has been removed, the helmet can be removed from the injured patient. Less motion in the cervical spine is generated when the face mask is removed from the football helmet prior to removing the helmet.95 Removal of the face mask allows for easier access to stabilize the cervical spine. However, circumstances may arise where the face mask cannot be removed. The sports medicine team should be prepared to remove the helmet under both conditions. Figures 9.24 and 9.25 demonstrate helmet removal with the face mask off and on, respectively. When working with lacrosse, hockey, or other types of helmets, different considerations may need to be made.96-98If time is of the essence, consider leaving the face mask on and simply removing the helmet with the face mask attached.

Figure 9.24 Helmet removal with no face mask.
Courtesy of University of Georgia.

Figure 9.25 Helmet removal with face mask.
Courtesy of University of Georgia.
Here are some tips for helmet removal:
- The chin strap should be cut away, because unsnapping the helmet may create unnecessary movement.
- Cheek pads should be removed from the helmet using a tongue depressor (or something similar) to snap the pad away from the inside of the helmet. However, the ability to remove the cheek pads varies based on the model of the helmet.
- If possible, air bladders in the helmet should be deflated to loosen the fit on the helmet on the patient's head.
- Before the removing the helmet:
- Manual inline stabilization should be transferred from the rescuer at the patient's head (rescuer 1) to rescuer 2, who can provide inline stabilization from the front of the patient.
- Rescuer 2 places 1 hand on the chin and the other hand on the posterior side of the patient's neck (or as depicted in figure 9.26, on either side of the patient's head).
- Rescuer 1, located at the head, grasps the side of the helmet while slightly spreading the cheek pad area on the helmet.
- Rescuer 1 then rotates the helmet forward while sliding the helmet off the patient's head, being mindful to not place the head into flexion or extension.
- Once the helmet is removed, manual inline stabilization should be returned to rescuer 1 and padding (such as a folded towel) should be placed under the patient's head.8 This padding will offset the height of the shoulder pads and prevent hyperextension, which can decrease space available for the cord.
- ATs and other rescue personnel should practice helmet removal with all types of helmets used at their venue.

Figure 9.26 Helmet removal: baseball catcher.
Courtesy of University of Georgia.
Traumatic injuries to the head and face: Subdural hematoma
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.2 Bleeding collects under the inner layer of the dura mater but external to the brain and arachnoid membrane. Subdural hematomas can become life-threatening very quickly.
Incidence and Epidemiology
A subdural hematoma results most often from a severe head injury. Acceleration-deceleration forces cause injuries as the patient's momentum is stopped suddenly by a solid object and the brain makes contact with the inside of the skull.2 Subdural hematomas can present either acutely or chronically based on the time since symptoms first appeared. Acute subdural hematomas occur within 72 hours after injury, while chronic subdural hematomas may take as long 3 weeks to show signs.
Risk Factors
Risk factors associated with acute subdural hematoma include head trauma, postsurgical complications, anticoagulation drug therapy, and nontraumatic cerebral aneurysm. As with epidural hematomas, decreased risk is associated with appropriate use of protective headgear in athletic environments.
Signs and Symptoms
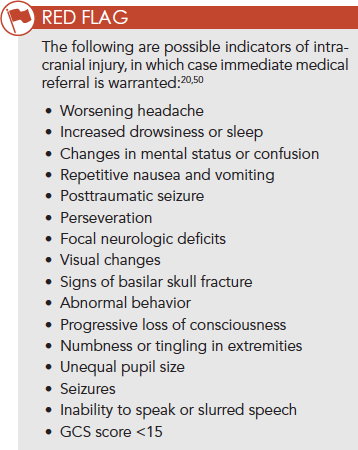
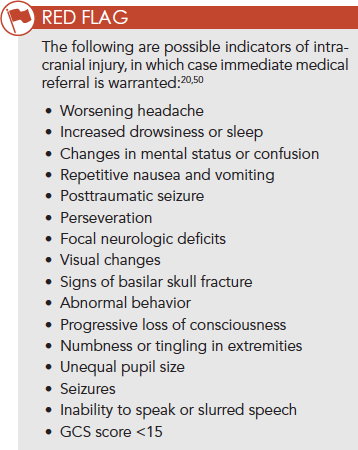
Immediate medical referral and emergency management are recommended for any of the signs presented in the Red Flag box. Subsequent impacts to the head during the development of a chronic subdural hematoma may put patients at a higher risk of experiencing a life-threatening situation; as such, continued monitoring and serial assessment is important.
Field Assessment Techniques
In the pre-competition season, athletes participating in at-risk sports (e.g., football, soccer, rugby) should undergo baseline neurocognitive testing, either as a component of a pre-participation physical exam or an adjunct to such an exam. The importance of an established emergency care plan (ECP) cannot be overemphasized; the ECP provides for a standard of care and ensures rapid and efficient treatment measures are in place.
The Canadian CT Head Rule is a clinical prediction rule that uses CT scans to identify head injuries that could require neurosurgical intervention.55 Inclusion criteria include patients with a GCS score of 13 to 15; injury within 24 hours; and blunt head trauma resulting in loss of consciousness, definite amnesia, or disorientation. Exclusion criteria include patients under 16 years of age, nontraumatic cases, patients using anticoagulants or with a bleeding disorder, obvious skull fracture, GCS score of less than 13, and pregnancy.
Immediate Management Techniques
Emergency management of any sports-related injury should first address a primary survey assessment of the patient's mental status, followed by ensuring proper ABC. Knowledge of the patient's neurocognitive baseline may be critical for both short-term and long-term management, and it is helpful when conducting a sideline assessment. Although uncommon, possible differential diagnoses should include intracranial hemorrhage, because the signs and symptoms of a concussion and an intracranial injury are differentiated.50,56 Incorporating potential clinical signs of intracranial injury into the assessment of a patient with a suspected concussion is important.50 Injuries to the head can escalate into medical emergencies quickly, therefore an efficient process of providing immediate care based on signs and symptoms is required (figure 8.6).

Figure 8.6 Head injury algorithm.
Sternoclavicular joint injury
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton.
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton. This joint is a loose connection between the medial clavicle and manubrium of the superior sternum. It has a joint capsule, disc, and several ligaments in addition to the SC ligament—the intraclavicular ligament (between the two medial aspects of the clavicle, superior to the sternum) and the costoclavicular ligament, which maintains the stability of the clavicle on the ribs below. The SC joint is inherently unstable, and only a portion of the clavicle actually articulates with the manubrium, relying on the SC ligament to provide more stability.
Injury to the SC joint is one of the true medical emergencies in orthopedics. Just posterior to the joint lie the trachea and carotid arteries, and not too lateral from there, the subclavian arteries are located (figure 10.12). A posterior subluxation or dislocation can be a life-threatening emergency with compression on any of these structures.
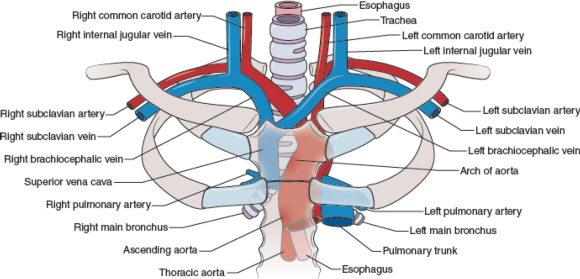
Figure 10.12 Internal structures behind the sternoclavicular (SC) joint.
Because of the SC's importance in connecting the arm to the body proper, the SC joint has many MOIs. One can fall on an outstretched hand or elbow, and the force can transmit along the bones of the arm, acromion of the scapula, and clavicle to the joint, injuring it. Another MOI is a fall on the lateral aspect of the shoulder (humerus or acromion of the scapula), or lying on one side with a pileup on the opposite lateral shoulder. In both of these situations, the force is transmitted along from the humerus/acromion to the clavicle and on to the biomechanically weakest aspect. The athlete could sprain the acromioclavicular joint or fracture the clavicle, or the force could continue medially and injure the SC joint at the sternum.
Incidence and Epidemiology
Injury to the sternoclavicular joint is rare, and posterior dislocations are more unusual. In a study of 251 SC dislocations, only 80 were posterior dislocations. Of the total number of dislocations (both anterior and posterior), the average age of the patient was 29 years old, and 67% of them were male.5 These data are consistent in other publications, in that younger males are more likely to sustain SC injuries than are other age groups or women.6
Risk Factors
Risk factors for injuring the SC joint include falling on an outstretched arm, elbow, or lateral shoulder. As noted, men under 30 years old tend to have higher incidences of SC injuries, so that population is at higher risk. Because high-velocity contact is a MOI, motor vehicle accidents are also a means of sustaining this injury.
Signs and Symptoms
When evaluating an injury to the upper extremity, it is important to be aware of the anatomical connection of the upper extremity and the SC joint. The athlete may initially feel more soreness at the point of impact (e.g., hand, elbow, shoulder) and not recognize the injury to the SC joint. Appreciating the MOI for a potential transmitted force to the medial clavicle and sternum is critical.
On inspection, a deformity may be present over the medial clavicle. It can range from mild swelling to gross deformity. A divot at the SC junction may indicate a posterior dislocation or subluxation, or a posterior fracture of the medial clavicular head (depending on the age of the athlete). Palpation results in a painful SC ligament or joint. Crepitus indicates a fracture, not dislocation or subluxation, but it is equally disconcerting.
Joint stress testing is not recommended, but sometimes the athlete presents with pain away from the SC joint, and that specific injury is not considered at the initial time of testing. The patient will present with an unwillingness to demonstrate full glenohumeral range of motion, because the stress on that joint affects the SC joint.
In a true posterior SC dislocation or subluxation, the patient may have dyspnea or hoarseness and relate difficulty swallowing, because the trachea is pushing posteriorly into the esophagus. If any of these complaints occur, consider it a medical emergency and transport via ambulance as soon as possible. On occasion, the patient will not identify the difficulty swallowing and hoarseness as related to the falling injury, and may not report these conditions. Anecdotal conversations with ATs indicate that athletes sometimes delay reporting issues of the voice or swallowing because they do not relate it to the SC sprain injury, only to have it be an emergency hours later when swelling increases and the airway begins to be compromised.
Field Assessment Techniques
Always assume a potential SC injury when presented with a mechanism consistent with the biomechanical weakness of the joint. Palpate all aspects of the clavicle, SC joint, and manubrium when evaluating falls resulting in landing on the outstretched hand, olecranon of the elbow, or acromion of scapula. If injury to the SC joint is suspected, assess airway and quality of voice. Ask the athlete to swallow, and query whether that action feels normal. Patients with swelling over the SC joint, who report that it is hard to swallow, or who have altered breath sounds, anxiety, or hoarseness should be removed from activity, have their shoulder pads removed (if wearing them), and be transported to the emergency department via ambulance. While waiting for transport, keep the athlete sitting up to facilitate breathing, and apply a sling to the affected arm. The sling will prevent unnecessary movement of the SC joint.
Reduction of the sternoclavicular joint is not recommended on the field. This procedure is performed under sedation or general anesthesia in an operating room. Open reduction and possible stabilization are necessary in situations of failed closed reduction or ongoing symptoms.7 Typically, surgical reduction of this injury is performed in conjunction with a cardiothoracic surgeon because of the potential for complications external to orthopedic surgery.
Diagnostic Accuracy
Standard radiographs of the SC joint are ineffective, because the X-rays are poor at viewing relevant anatomy of the joint.7 One technique that does provide better viewing is the serendipity view, which allows a 40° cephalic tilt.7 In this technique, an anterior dislocation presents as a superiorly displaced medial clavicle, and a posterior dislocation is represented as an inferiorly displaced medial clavicle.7 The preferred imaging is CT, which clearly defines the vascular and respiratory features that could be compromised.
Immediate Management Techniques
If the patient reports no difficulty with breathing or swallowing, but has swelling or tenderness over the SC joint, remove the patient from activity, place the affected arm in a sling, and reassess often. In this situation, ice may be held in place by the patient for 15- to 20-minute intervals if it relieves pain and swelling.
Indications
Dyspnea, hoarseness, or dysphagia following a collision or fall on an out stretched arm, elbow, or lateral shoulder are indications to transport the athlete via ambulance to the nearest ED.
Contraindications
Applying ice to the SC region after an acute injury may be contraindicated for a few reasons. The weight of the ice itself could put additional pressure on an unstable joint, further aggravating any dyspnea. Using a wrap to secure the ice to the area provides additional pressure to the area, which can actually worsen an unstable SC joint injury. The anatomical positioning of the trachea and major vessels from the heart immediately under the thin skin of the neck make ice an inappropriate treatment.
Criteria for Deciding to Transport for Further Medical Examination
Dyspnea, hoarseness, and difficulty swallowing following a collision or fall on an outstretched arm, elbow, or lateral shoulder are indications to transport the patient via ambulance to the nearest emergency department.
Transportation Techniques
Patients with a suspected posterior SC sprain should have supplemental oxygen available delivered via a nasal cannula. Transportation should occur in a recumbent position to facilitate easier respiration. A sling should be placed on the affected arm to relieve any traction of the SC joint from the weight of the upper extremity.
Heat-related emergencies in athletes
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS).
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS). EHS is the only true heat-related life-threatening emergency, and it is the only heat illness discussed here. As the name suggests, EHS is brought about by the combination of exertion (working out), temperature (including air and humidity), and other factors. A person can acclimate to the hot weather if given the time and cautiously increasing the activity duration slowly in the hot environment. Heatstroke is preventable in many aspects, including paying close attention to the weather (air temperature, ambient temperature, humidity, wind, sunshine), the heat and humidity trends in the local area, clothing and equipment worn, work-to-rest ratio, and hydration and food intake.13 Other salient factors include medical conditions, body mass, poor conditioning, medications, prior history of heat illness, and other predispositions that can exacerbate heat illness.14
Incidence and Epidemiology
Although the overall risk of EHS is low, its consequences can be fatal. According to the National Center for Catastrophic Sport Injury Research, 148 deaths have occurred since 1955 (56 since 1996) due to EHS in football.17 Rates are highest across all levels of football (youth, high school, and collegiate) during the preseason and lower during youth practices and high school games.18 Athletics are not alone in EHS injury; the U.S. military forces also have significant data. Fort Benning, Georgia and Fort Bragg, North Carolina led a 14-year study period with over 1,400 heat-related illnesses each, and nearly 3,500 incidents were reported from military bases in North and South Carolina combined (table 15.2).19
Medical Consequences
of Heatstroke
The systemic physiological effects of untreated EHS are many. The rising internal temperature denatures proteins and cellular membranes, causing an inflammatory response.20 As a reaction, the body relocates an aspect of bacteria usually found in the gastrointestinal system, which can promulgate a sepsis reaction systemically, and therefore begins a coagulation reaction throughout organs.20 Aside from death, EHS can elicit multi-organ failure, acute respiratory distress syndrome, and coma. Organ failure can become irreversible and the long-term sequelae catastrophic.
Signs and Symptoms
If the weather is hot or humid, be suspicious of EHS for any athlete who presents with any of these signs of symptoms. The 2 cardinal signs of EHS are a rectal temperature over 105°F (40.5°C) and central nervous system dysfunction, namely, concussion-like behaviors.21 Strictly from an observational standpoint, the athlete may be disoriented, confused, or dizzy, and his performance may be deteriorating. EHS patients tend to have diaphoretic and hot skin. The presence or absence of sweat should not be a deterrent to consider EHS, given other feedback. Complaints of muscular cramping, headache, weakness, or dry mouth are worth continued exploration. Nausea, vomiting, or diarrhea can occur prior to
collapse.14,20-23
Sudden collapse, seizure, altered consciousness, or coma can occur and will likely transpire if not rapidly diagnosed and treated.21,22 Vital signs can diminish with time, especially if the patient is untreated.
Field Assessment Techniques
A person who has heatstroke presents with concussion-like symptoms, which include confusion, stupor, dizziness, personality changes, and acting combative or complacent. A rapid decision must be made to assess core temperature using a rectal thermometer to diagnose EHS (figure 15.1). Every minute delay to diagnose EHS via rectal thermometry is critical.
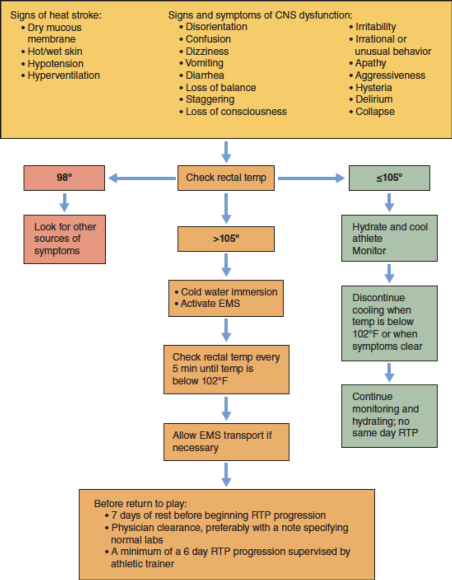
Figure 15.1 Decision tree for EHS.
Safe helmet removal after spinal injury
If the decision has been made to remove the athlete’s equipment, the helmet and shoulder pads should be considered a unit and both be removed.
If the decision has been made to remove the athlete's equipment, the helmet and shoulder pads should be considered a unit and both be removed. Once the face mask has been removed, the helmet can be removed from the injured patient. Less motion in the cervical spine is generated when the face mask is removed from the football helmet prior to removing the helmet.95 Removal of the face mask allows for easier access to stabilize the cervical spine. However, circumstances may arise where the face mask cannot be removed. The sports medicine team should be prepared to remove the helmet under both conditions. Figures 9.24 and 9.25 demonstrate helmet removal with the face mask off and on, respectively. When working with lacrosse, hockey, or other types of helmets, different considerations may need to be made.96-98If time is of the essence, consider leaving the face mask on and simply removing the helmet with the face mask attached.

Figure 9.24 Helmet removal with no face mask.
Courtesy of University of Georgia.

Figure 9.25 Helmet removal with face mask.
Courtesy of University of Georgia.
Here are some tips for helmet removal:
- The chin strap should be cut away, because unsnapping the helmet may create unnecessary movement.
- Cheek pads should be removed from the helmet using a tongue depressor (or something similar) to snap the pad away from the inside of the helmet. However, the ability to remove the cheek pads varies based on the model of the helmet.
- If possible, air bladders in the helmet should be deflated to loosen the fit on the helmet on the patient's head.
- Before the removing the helmet:
- Manual inline stabilization should be transferred from the rescuer at the patient's head (rescuer 1) to rescuer 2, who can provide inline stabilization from the front of the patient.
- Rescuer 2 places 1 hand on the chin and the other hand on the posterior side of the patient's neck (or as depicted in figure 9.26, on either side of the patient's head).
- Rescuer 1, located at the head, grasps the side of the helmet while slightly spreading the cheek pad area on the helmet.
- Rescuer 1 then rotates the helmet forward while sliding the helmet off the patient's head, being mindful to not place the head into flexion or extension.
- Once the helmet is removed, manual inline stabilization should be returned to rescuer 1 and padding (such as a folded towel) should be placed under the patient's head.8 This padding will offset the height of the shoulder pads and prevent hyperextension, which can decrease space available for the cord.
- ATs and other rescue personnel should practice helmet removal with all types of helmets used at their venue.

Figure 9.26 Helmet removal: baseball catcher.
Courtesy of University of Georgia.
Traumatic injuries to the head and face: Subdural hematoma
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.2 Bleeding collects under the inner layer of the dura mater but external to the brain and arachnoid membrane. Subdural hematomas can become life-threatening very quickly.
Incidence and Epidemiology
A subdural hematoma results most often from a severe head injury. Acceleration-deceleration forces cause injuries as the patient's momentum is stopped suddenly by a solid object and the brain makes contact with the inside of the skull.2 Subdural hematomas can present either acutely or chronically based on the time since symptoms first appeared. Acute subdural hematomas occur within 72 hours after injury, while chronic subdural hematomas may take as long 3 weeks to show signs.
Risk Factors
Risk factors associated with acute subdural hematoma include head trauma, postsurgical complications, anticoagulation drug therapy, and nontraumatic cerebral aneurysm. As with epidural hematomas, decreased risk is associated with appropriate use of protective headgear in athletic environments.
Signs and Symptoms
Immediate medical referral and emergency management are recommended for any of the signs presented in the Red Flag box. Subsequent impacts to the head during the development of a chronic subdural hematoma may put patients at a higher risk of experiencing a life-threatening situation; as such, continued monitoring and serial assessment is important.
Field Assessment Techniques
In the pre-competition season, athletes participating in at-risk sports (e.g., football, soccer, rugby) should undergo baseline neurocognitive testing, either as a component of a pre-participation physical exam or an adjunct to such an exam. The importance of an established emergency care plan (ECP) cannot be overemphasized; the ECP provides for a standard of care and ensures rapid and efficient treatment measures are in place.
The Canadian CT Head Rule is a clinical prediction rule that uses CT scans to identify head injuries that could require neurosurgical intervention.55 Inclusion criteria include patients with a GCS score of 13 to 15; injury within 24 hours; and blunt head trauma resulting in loss of consciousness, definite amnesia, or disorientation. Exclusion criteria include patients under 16 years of age, nontraumatic cases, patients using anticoagulants or with a bleeding disorder, obvious skull fracture, GCS score of less than 13, and pregnancy.
Immediate Management Techniques
Emergency management of any sports-related injury should first address a primary survey assessment of the patient's mental status, followed by ensuring proper ABC. Knowledge of the patient's neurocognitive baseline may be critical for both short-term and long-term management, and it is helpful when conducting a sideline assessment. Although uncommon, possible differential diagnoses should include intracranial hemorrhage, because the signs and symptoms of a concussion and an intracranial injury are differentiated.50,56 Incorporating potential clinical signs of intracranial injury into the assessment of a patient with a suspected concussion is important.50 Injuries to the head can escalate into medical emergencies quickly, therefore an efficient process of providing immediate care based on signs and symptoms is required (figure 8.6).

Figure 8.6 Head injury algorithm.
Sternoclavicular joint injury
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton.
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton. This joint is a loose connection between the medial clavicle and manubrium of the superior sternum. It has a joint capsule, disc, and several ligaments in addition to the SC ligament—the intraclavicular ligament (between the two medial aspects of the clavicle, superior to the sternum) and the costoclavicular ligament, which maintains the stability of the clavicle on the ribs below. The SC joint is inherently unstable, and only a portion of the clavicle actually articulates with the manubrium, relying on the SC ligament to provide more stability.
Injury to the SC joint is one of the true medical emergencies in orthopedics. Just posterior to the joint lie the trachea and carotid arteries, and not too lateral from there, the subclavian arteries are located (figure 10.12). A posterior subluxation or dislocation can be a life-threatening emergency with compression on any of these structures.
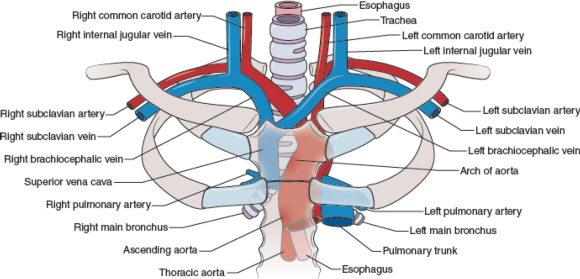
Figure 10.12 Internal structures behind the sternoclavicular (SC) joint.
Because of the SC's importance in connecting the arm to the body proper, the SC joint has many MOIs. One can fall on an outstretched hand or elbow, and the force can transmit along the bones of the arm, acromion of the scapula, and clavicle to the joint, injuring it. Another MOI is a fall on the lateral aspect of the shoulder (humerus or acromion of the scapula), or lying on one side with a pileup on the opposite lateral shoulder. In both of these situations, the force is transmitted along from the humerus/acromion to the clavicle and on to the biomechanically weakest aspect. The athlete could sprain the acromioclavicular joint or fracture the clavicle, or the force could continue medially and injure the SC joint at the sternum.
Incidence and Epidemiology
Injury to the sternoclavicular joint is rare, and posterior dislocations are more unusual. In a study of 251 SC dislocations, only 80 were posterior dislocations. Of the total number of dislocations (both anterior and posterior), the average age of the patient was 29 years old, and 67% of them were male.5 These data are consistent in other publications, in that younger males are more likely to sustain SC injuries than are other age groups or women.6
Risk Factors
Risk factors for injuring the SC joint include falling on an outstretched arm, elbow, or lateral shoulder. As noted, men under 30 years old tend to have higher incidences of SC injuries, so that population is at higher risk. Because high-velocity contact is a MOI, motor vehicle accidents are also a means of sustaining this injury.
Signs and Symptoms
When evaluating an injury to the upper extremity, it is important to be aware of the anatomical connection of the upper extremity and the SC joint. The athlete may initially feel more soreness at the point of impact (e.g., hand, elbow, shoulder) and not recognize the injury to the SC joint. Appreciating the MOI for a potential transmitted force to the medial clavicle and sternum is critical.
On inspection, a deformity may be present over the medial clavicle. It can range from mild swelling to gross deformity. A divot at the SC junction may indicate a posterior dislocation or subluxation, or a posterior fracture of the medial clavicular head (depending on the age of the athlete). Palpation results in a painful SC ligament or joint. Crepitus indicates a fracture, not dislocation or subluxation, but it is equally disconcerting.
Joint stress testing is not recommended, but sometimes the athlete presents with pain away from the SC joint, and that specific injury is not considered at the initial time of testing. The patient will present with an unwillingness to demonstrate full glenohumeral range of motion, because the stress on that joint affects the SC joint.
In a true posterior SC dislocation or subluxation, the patient may have dyspnea or hoarseness and relate difficulty swallowing, because the trachea is pushing posteriorly into the esophagus. If any of these complaints occur, consider it a medical emergency and transport via ambulance as soon as possible. On occasion, the patient will not identify the difficulty swallowing and hoarseness as related to the falling injury, and may not report these conditions. Anecdotal conversations with ATs indicate that athletes sometimes delay reporting issues of the voice or swallowing because they do not relate it to the SC sprain injury, only to have it be an emergency hours later when swelling increases and the airway begins to be compromised.
Field Assessment Techniques
Always assume a potential SC injury when presented with a mechanism consistent with the biomechanical weakness of the joint. Palpate all aspects of the clavicle, SC joint, and manubrium when evaluating falls resulting in landing on the outstretched hand, olecranon of the elbow, or acromion of scapula. If injury to the SC joint is suspected, assess airway and quality of voice. Ask the athlete to swallow, and query whether that action feels normal. Patients with swelling over the SC joint, who report that it is hard to swallow, or who have altered breath sounds, anxiety, or hoarseness should be removed from activity, have their shoulder pads removed (if wearing them), and be transported to the emergency department via ambulance. While waiting for transport, keep the athlete sitting up to facilitate breathing, and apply a sling to the affected arm. The sling will prevent unnecessary movement of the SC joint.
Reduction of the sternoclavicular joint is not recommended on the field. This procedure is performed under sedation or general anesthesia in an operating room. Open reduction and possible stabilization are necessary in situations of failed closed reduction or ongoing symptoms.7 Typically, surgical reduction of this injury is performed in conjunction with a cardiothoracic surgeon because of the potential for complications external to orthopedic surgery.
Diagnostic Accuracy
Standard radiographs of the SC joint are ineffective, because the X-rays are poor at viewing relevant anatomy of the joint.7 One technique that does provide better viewing is the serendipity view, which allows a 40° cephalic tilt.7 In this technique, an anterior dislocation presents as a superiorly displaced medial clavicle, and a posterior dislocation is represented as an inferiorly displaced medial clavicle.7 The preferred imaging is CT, which clearly defines the vascular and respiratory features that could be compromised.
Immediate Management Techniques
If the patient reports no difficulty with breathing or swallowing, but has swelling or tenderness over the SC joint, remove the patient from activity, place the affected arm in a sling, and reassess often. In this situation, ice may be held in place by the patient for 15- to 20-minute intervals if it relieves pain and swelling.
Indications
Dyspnea, hoarseness, or dysphagia following a collision or fall on an out stretched arm, elbow, or lateral shoulder are indications to transport the athlete via ambulance to the nearest ED.
Contraindications
Applying ice to the SC region after an acute injury may be contraindicated for a few reasons. The weight of the ice itself could put additional pressure on an unstable joint, further aggravating any dyspnea. Using a wrap to secure the ice to the area provides additional pressure to the area, which can actually worsen an unstable SC joint injury. The anatomical positioning of the trachea and major vessels from the heart immediately under the thin skin of the neck make ice an inappropriate treatment.
Criteria for Deciding to Transport for Further Medical Examination
Dyspnea, hoarseness, and difficulty swallowing following a collision or fall on an outstretched arm, elbow, or lateral shoulder are indications to transport the patient via ambulance to the nearest emergency department.
Transportation Techniques
Patients with a suspected posterior SC sprain should have supplemental oxygen available delivered via a nasal cannula. Transportation should occur in a recumbent position to facilitate easier respiration. A sling should be placed on the affected arm to relieve any traction of the SC joint from the weight of the upper extremity.
Heat-related emergencies in athletes
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS).
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS). EHS is the only true heat-related life-threatening emergency, and it is the only heat illness discussed here. As the name suggests, EHS is brought about by the combination of exertion (working out), temperature (including air and humidity), and other factors. A person can acclimate to the hot weather if given the time and cautiously increasing the activity duration slowly in the hot environment. Heatstroke is preventable in many aspects, including paying close attention to the weather (air temperature, ambient temperature, humidity, wind, sunshine), the heat and humidity trends in the local area, clothing and equipment worn, work-to-rest ratio, and hydration and food intake.13 Other salient factors include medical conditions, body mass, poor conditioning, medications, prior history of heat illness, and other predispositions that can exacerbate heat illness.14
Incidence and Epidemiology
Although the overall risk of EHS is low, its consequences can be fatal. According to the National Center for Catastrophic Sport Injury Research, 148 deaths have occurred since 1955 (56 since 1996) due to EHS in football.17 Rates are highest across all levels of football (youth, high school, and collegiate) during the preseason and lower during youth practices and high school games.18 Athletics are not alone in EHS injury; the U.S. military forces also have significant data. Fort Benning, Georgia and Fort Bragg, North Carolina led a 14-year study period with over 1,400 heat-related illnesses each, and nearly 3,500 incidents were reported from military bases in North and South Carolina combined (table 15.2).19
Medical Consequences
of Heatstroke
The systemic physiological effects of untreated EHS are many. The rising internal temperature denatures proteins and cellular membranes, causing an inflammatory response.20 As a reaction, the body relocates an aspect of bacteria usually found in the gastrointestinal system, which can promulgate a sepsis reaction systemically, and therefore begins a coagulation reaction throughout organs.20 Aside from death, EHS can elicit multi-organ failure, acute respiratory distress syndrome, and coma. Organ failure can become irreversible and the long-term sequelae catastrophic.
Signs and Symptoms
If the weather is hot or humid, be suspicious of EHS for any athlete who presents with any of these signs of symptoms. The 2 cardinal signs of EHS are a rectal temperature over 105°F (40.5°C) and central nervous system dysfunction, namely, concussion-like behaviors.21 Strictly from an observational standpoint, the athlete may be disoriented, confused, or dizzy, and his performance may be deteriorating. EHS patients tend to have diaphoretic and hot skin. The presence or absence of sweat should not be a deterrent to consider EHS, given other feedback. Complaints of muscular cramping, headache, weakness, or dry mouth are worth continued exploration. Nausea, vomiting, or diarrhea can occur prior to
collapse.14,20-23
Sudden collapse, seizure, altered consciousness, or coma can occur and will likely transpire if not rapidly diagnosed and treated.21,22 Vital signs can diminish with time, especially if the patient is untreated.
Field Assessment Techniques
A person who has heatstroke presents with concussion-like symptoms, which include confusion, stupor, dizziness, personality changes, and acting combative or complacent. A rapid decision must be made to assess core temperature using a rectal thermometer to diagnose EHS (figure 15.1). Every minute delay to diagnose EHS via rectal thermometry is critical.
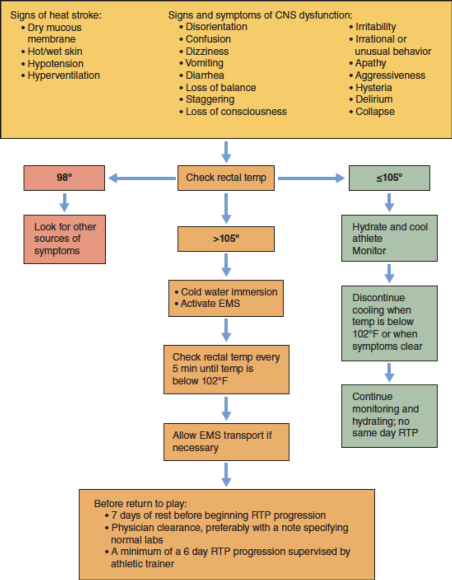
Figure 15.1 Decision tree for EHS.
Safe helmet removal after spinal injury
If the decision has been made to remove the athlete’s equipment, the helmet and shoulder pads should be considered a unit and both be removed.
If the decision has been made to remove the athlete's equipment, the helmet and shoulder pads should be considered a unit and both be removed. Once the face mask has been removed, the helmet can be removed from the injured patient. Less motion in the cervical spine is generated when the face mask is removed from the football helmet prior to removing the helmet.95 Removal of the face mask allows for easier access to stabilize the cervical spine. However, circumstances may arise where the face mask cannot be removed. The sports medicine team should be prepared to remove the helmet under both conditions. Figures 9.24 and 9.25 demonstrate helmet removal with the face mask off and on, respectively. When working with lacrosse, hockey, or other types of helmets, different considerations may need to be made.96-98If time is of the essence, consider leaving the face mask on and simply removing the helmet with the face mask attached.

Figure 9.24 Helmet removal with no face mask.
Courtesy of University of Georgia.

Figure 9.25 Helmet removal with face mask.
Courtesy of University of Georgia.
Here are some tips for helmet removal:
- The chin strap should be cut away, because unsnapping the helmet may create unnecessary movement.
- Cheek pads should be removed from the helmet using a tongue depressor (or something similar) to snap the pad away from the inside of the helmet. However, the ability to remove the cheek pads varies based on the model of the helmet.
- If possible, air bladders in the helmet should be deflated to loosen the fit on the helmet on the patient's head.
- Before the removing the helmet:
- Manual inline stabilization should be transferred from the rescuer at the patient's head (rescuer 1) to rescuer 2, who can provide inline stabilization from the front of the patient.
- Rescuer 2 places 1 hand on the chin and the other hand on the posterior side of the patient's neck (or as depicted in figure 9.26, on either side of the patient's head).
- Rescuer 1, located at the head, grasps the side of the helmet while slightly spreading the cheek pad area on the helmet.
- Rescuer 1 then rotates the helmet forward while sliding the helmet off the patient's head, being mindful to not place the head into flexion or extension.
- Once the helmet is removed, manual inline stabilization should be returned to rescuer 1 and padding (such as a folded towel) should be placed under the patient's head.8 This padding will offset the height of the shoulder pads and prevent hyperextension, which can decrease space available for the cord.
- ATs and other rescue personnel should practice helmet removal with all types of helmets used at their venue.

Figure 9.26 Helmet removal: baseball catcher.
Courtesy of University of Georgia.
Traumatic injuries to the head and face: Subdural hematoma
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.2 Bleeding collects under the inner layer of the dura mater but external to the brain and arachnoid membrane. Subdural hematomas can become life-threatening very quickly.
Incidence and Epidemiology
A subdural hematoma results most often from a severe head injury. Acceleration-deceleration forces cause injuries as the patient's momentum is stopped suddenly by a solid object and the brain makes contact with the inside of the skull.2 Subdural hematomas can present either acutely or chronically based on the time since symptoms first appeared. Acute subdural hematomas occur within 72 hours after injury, while chronic subdural hematomas may take as long 3 weeks to show signs.
Risk Factors
Risk factors associated with acute subdural hematoma include head trauma, postsurgical complications, anticoagulation drug therapy, and nontraumatic cerebral aneurysm. As with epidural hematomas, decreased risk is associated with appropriate use of protective headgear in athletic environments.
Signs and Symptoms
Immediate medical referral and emergency management are recommended for any of the signs presented in the Red Flag box. Subsequent impacts to the head during the development of a chronic subdural hematoma may put patients at a higher risk of experiencing a life-threatening situation; as such, continued monitoring and serial assessment is important.
Field Assessment Techniques
In the pre-competition season, athletes participating in at-risk sports (e.g., football, soccer, rugby) should undergo baseline neurocognitive testing, either as a component of a pre-participation physical exam or an adjunct to such an exam. The importance of an established emergency care plan (ECP) cannot be overemphasized; the ECP provides for a standard of care and ensures rapid and efficient treatment measures are in place.
The Canadian CT Head Rule is a clinical prediction rule that uses CT scans to identify head injuries that could require neurosurgical intervention.55 Inclusion criteria include patients with a GCS score of 13 to 15; injury within 24 hours; and blunt head trauma resulting in loss of consciousness, definite amnesia, or disorientation. Exclusion criteria include patients under 16 years of age, nontraumatic cases, patients using anticoagulants or with a bleeding disorder, obvious skull fracture, GCS score of less than 13, and pregnancy.
Immediate Management Techniques
Emergency management of any sports-related injury should first address a primary survey assessment of the patient's mental status, followed by ensuring proper ABC. Knowledge of the patient's neurocognitive baseline may be critical for both short-term and long-term management, and it is helpful when conducting a sideline assessment. Although uncommon, possible differential diagnoses should include intracranial hemorrhage, because the signs and symptoms of a concussion and an intracranial injury are differentiated.50,56 Incorporating potential clinical signs of intracranial injury into the assessment of a patient with a suspected concussion is important.50 Injuries to the head can escalate into medical emergencies quickly, therefore an efficient process of providing immediate care based on signs and symptoms is required (figure 8.6).

Figure 8.6 Head injury algorithm.
Sternoclavicular joint injury
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton.
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton. This joint is a loose connection between the medial clavicle and manubrium of the superior sternum. It has a joint capsule, disc, and several ligaments in addition to the SC ligament—the intraclavicular ligament (between the two medial aspects of the clavicle, superior to the sternum) and the costoclavicular ligament, which maintains the stability of the clavicle on the ribs below. The SC joint is inherently unstable, and only a portion of the clavicle actually articulates with the manubrium, relying on the SC ligament to provide more stability.
Injury to the SC joint is one of the true medical emergencies in orthopedics. Just posterior to the joint lie the trachea and carotid arteries, and not too lateral from there, the subclavian arteries are located (figure 10.12). A posterior subluxation or dislocation can be a life-threatening emergency with compression on any of these structures.
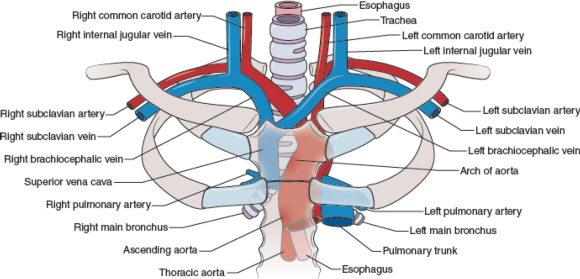
Figure 10.12 Internal structures behind the sternoclavicular (SC) joint.
Because of the SC's importance in connecting the arm to the body proper, the SC joint has many MOIs. One can fall on an outstretched hand or elbow, and the force can transmit along the bones of the arm, acromion of the scapula, and clavicle to the joint, injuring it. Another MOI is a fall on the lateral aspect of the shoulder (humerus or acromion of the scapula), or lying on one side with a pileup on the opposite lateral shoulder. In both of these situations, the force is transmitted along from the humerus/acromion to the clavicle and on to the biomechanically weakest aspect. The athlete could sprain the acromioclavicular joint or fracture the clavicle, or the force could continue medially and injure the SC joint at the sternum.
Incidence and Epidemiology
Injury to the sternoclavicular joint is rare, and posterior dislocations are more unusual. In a study of 251 SC dislocations, only 80 were posterior dislocations. Of the total number of dislocations (both anterior and posterior), the average age of the patient was 29 years old, and 67% of them were male.5 These data are consistent in other publications, in that younger males are more likely to sustain SC injuries than are other age groups or women.6
Risk Factors
Risk factors for injuring the SC joint include falling on an outstretched arm, elbow, or lateral shoulder. As noted, men under 30 years old tend to have higher incidences of SC injuries, so that population is at higher risk. Because high-velocity contact is a MOI, motor vehicle accidents are also a means of sustaining this injury.
Signs and Symptoms
When evaluating an injury to the upper extremity, it is important to be aware of the anatomical connection of the upper extremity and the SC joint. The athlete may initially feel more soreness at the point of impact (e.g., hand, elbow, shoulder) and not recognize the injury to the SC joint. Appreciating the MOI for a potential transmitted force to the medial clavicle and sternum is critical.
On inspection, a deformity may be present over the medial clavicle. It can range from mild swelling to gross deformity. A divot at the SC junction may indicate a posterior dislocation or subluxation, or a posterior fracture of the medial clavicular head (depending on the age of the athlete). Palpation results in a painful SC ligament or joint. Crepitus indicates a fracture, not dislocation or subluxation, but it is equally disconcerting.
Joint stress testing is not recommended, but sometimes the athlete presents with pain away from the SC joint, and that specific injury is not considered at the initial time of testing. The patient will present with an unwillingness to demonstrate full glenohumeral range of motion, because the stress on that joint affects the SC joint.
In a true posterior SC dislocation or subluxation, the patient may have dyspnea or hoarseness and relate difficulty swallowing, because the trachea is pushing posteriorly into the esophagus. If any of these complaints occur, consider it a medical emergency and transport via ambulance as soon as possible. On occasion, the patient will not identify the difficulty swallowing and hoarseness as related to the falling injury, and may not report these conditions. Anecdotal conversations with ATs indicate that athletes sometimes delay reporting issues of the voice or swallowing because they do not relate it to the SC sprain injury, only to have it be an emergency hours later when swelling increases and the airway begins to be compromised.
Field Assessment Techniques
Always assume a potential SC injury when presented with a mechanism consistent with the biomechanical weakness of the joint. Palpate all aspects of the clavicle, SC joint, and manubrium when evaluating falls resulting in landing on the outstretched hand, olecranon of the elbow, or acromion of scapula. If injury to the SC joint is suspected, assess airway and quality of voice. Ask the athlete to swallow, and query whether that action feels normal. Patients with swelling over the SC joint, who report that it is hard to swallow, or who have altered breath sounds, anxiety, or hoarseness should be removed from activity, have their shoulder pads removed (if wearing them), and be transported to the emergency department via ambulance. While waiting for transport, keep the athlete sitting up to facilitate breathing, and apply a sling to the affected arm. The sling will prevent unnecessary movement of the SC joint.
Reduction of the sternoclavicular joint is not recommended on the field. This procedure is performed under sedation or general anesthesia in an operating room. Open reduction and possible stabilization are necessary in situations of failed closed reduction or ongoing symptoms.7 Typically, surgical reduction of this injury is performed in conjunction with a cardiothoracic surgeon because of the potential for complications external to orthopedic surgery.
Diagnostic Accuracy
Standard radiographs of the SC joint are ineffective, because the X-rays are poor at viewing relevant anatomy of the joint.7 One technique that does provide better viewing is the serendipity view, which allows a 40° cephalic tilt.7 In this technique, an anterior dislocation presents as a superiorly displaced medial clavicle, and a posterior dislocation is represented as an inferiorly displaced medial clavicle.7 The preferred imaging is CT, which clearly defines the vascular and respiratory features that could be compromised.
Immediate Management Techniques
If the patient reports no difficulty with breathing or swallowing, but has swelling or tenderness over the SC joint, remove the patient from activity, place the affected arm in a sling, and reassess often. In this situation, ice may be held in place by the patient for 15- to 20-minute intervals if it relieves pain and swelling.
Indications
Dyspnea, hoarseness, or dysphagia following a collision or fall on an out stretched arm, elbow, or lateral shoulder are indications to transport the athlete via ambulance to the nearest ED.
Contraindications
Applying ice to the SC region after an acute injury may be contraindicated for a few reasons. The weight of the ice itself could put additional pressure on an unstable joint, further aggravating any dyspnea. Using a wrap to secure the ice to the area provides additional pressure to the area, which can actually worsen an unstable SC joint injury. The anatomical positioning of the trachea and major vessels from the heart immediately under the thin skin of the neck make ice an inappropriate treatment.
Criteria for Deciding to Transport for Further Medical Examination
Dyspnea, hoarseness, and difficulty swallowing following a collision or fall on an outstretched arm, elbow, or lateral shoulder are indications to transport the patient via ambulance to the nearest emergency department.
Transportation Techniques
Patients with a suspected posterior SC sprain should have supplemental oxygen available delivered via a nasal cannula. Transportation should occur in a recumbent position to facilitate easier respiration. A sling should be placed on the affected arm to relieve any traction of the SC joint from the weight of the upper extremity.
Heat-related emergencies in athletes
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS).
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS). EHS is the only true heat-related life-threatening emergency, and it is the only heat illness discussed here. As the name suggests, EHS is brought about by the combination of exertion (working out), temperature (including air and humidity), and other factors. A person can acclimate to the hot weather if given the time and cautiously increasing the activity duration slowly in the hot environment. Heatstroke is preventable in many aspects, including paying close attention to the weather (air temperature, ambient temperature, humidity, wind, sunshine), the heat and humidity trends in the local area, clothing and equipment worn, work-to-rest ratio, and hydration and food intake.13 Other salient factors include medical conditions, body mass, poor conditioning, medications, prior history of heat illness, and other predispositions that can exacerbate heat illness.14
Incidence and Epidemiology
Although the overall risk of EHS is low, its consequences can be fatal. According to the National Center for Catastrophic Sport Injury Research, 148 deaths have occurred since 1955 (56 since 1996) due to EHS in football.17 Rates are highest across all levels of football (youth, high school, and collegiate) during the preseason and lower during youth practices and high school games.18 Athletics are not alone in EHS injury; the U.S. military forces also have significant data. Fort Benning, Georgia and Fort Bragg, North Carolina led a 14-year study period with over 1,400 heat-related illnesses each, and nearly 3,500 incidents were reported from military bases in North and South Carolina combined (table 15.2).19
Medical Consequences
of Heatstroke
The systemic physiological effects of untreated EHS are many. The rising internal temperature denatures proteins and cellular membranes, causing an inflammatory response.20 As a reaction, the body relocates an aspect of bacteria usually found in the gastrointestinal system, which can promulgate a sepsis reaction systemically, and therefore begins a coagulation reaction throughout organs.20 Aside from death, EHS can elicit multi-organ failure, acute respiratory distress syndrome, and coma. Organ failure can become irreversible and the long-term sequelae catastrophic.
Signs and Symptoms
If the weather is hot or humid, be suspicious of EHS for any athlete who presents with any of these signs of symptoms. The 2 cardinal signs of EHS are a rectal temperature over 105°F (40.5°C) and central nervous system dysfunction, namely, concussion-like behaviors.21 Strictly from an observational standpoint, the athlete may be disoriented, confused, or dizzy, and his performance may be deteriorating. EHS patients tend to have diaphoretic and hot skin. The presence or absence of sweat should not be a deterrent to consider EHS, given other feedback. Complaints of muscular cramping, headache, weakness, or dry mouth are worth continued exploration. Nausea, vomiting, or diarrhea can occur prior to
collapse.14,20-23
Sudden collapse, seizure, altered consciousness, or coma can occur and will likely transpire if not rapidly diagnosed and treated.21,22 Vital signs can diminish with time, especially if the patient is untreated.
Field Assessment Techniques
A person who has heatstroke presents with concussion-like symptoms, which include confusion, stupor, dizziness, personality changes, and acting combative or complacent. A rapid decision must be made to assess core temperature using a rectal thermometer to diagnose EHS (figure 15.1). Every minute delay to diagnose EHS via rectal thermometry is critical.
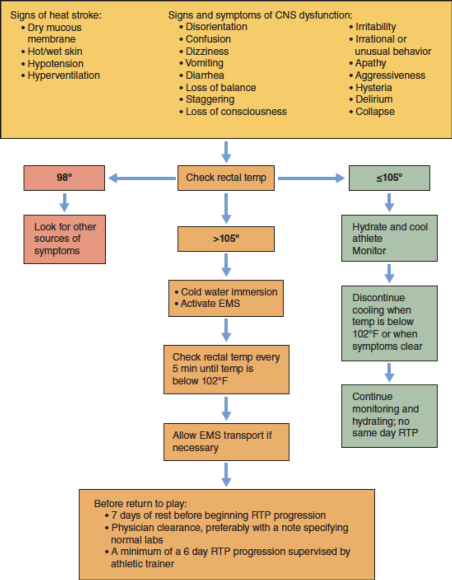
Figure 15.1 Decision tree for EHS.
Safe helmet removal after spinal injury
If the decision has been made to remove the athlete’s equipment, the helmet and shoulder pads should be considered a unit and both be removed.
If the decision has been made to remove the athlete's equipment, the helmet and shoulder pads should be considered a unit and both be removed. Once the face mask has been removed, the helmet can be removed from the injured patient. Less motion in the cervical spine is generated when the face mask is removed from the football helmet prior to removing the helmet.95 Removal of the face mask allows for easier access to stabilize the cervical spine. However, circumstances may arise where the face mask cannot be removed. The sports medicine team should be prepared to remove the helmet under both conditions. Figures 9.24 and 9.25 demonstrate helmet removal with the face mask off and on, respectively. When working with lacrosse, hockey, or other types of helmets, different considerations may need to be made.96-98If time is of the essence, consider leaving the face mask on and simply removing the helmet with the face mask attached.

Figure 9.24 Helmet removal with no face mask.
Courtesy of University of Georgia.

Figure 9.25 Helmet removal with face mask.
Courtesy of University of Georgia.
Here are some tips for helmet removal:
- The chin strap should be cut away, because unsnapping the helmet may create unnecessary movement.
- Cheek pads should be removed from the helmet using a tongue depressor (or something similar) to snap the pad away from the inside of the helmet. However, the ability to remove the cheek pads varies based on the model of the helmet.
- If possible, air bladders in the helmet should be deflated to loosen the fit on the helmet on the patient's head.
- Before the removing the helmet:
- Manual inline stabilization should be transferred from the rescuer at the patient's head (rescuer 1) to rescuer 2, who can provide inline stabilization from the front of the patient.
- Rescuer 2 places 1 hand on the chin and the other hand on the posterior side of the patient's neck (or as depicted in figure 9.26, on either side of the patient's head).
- Rescuer 1, located at the head, grasps the side of the helmet while slightly spreading the cheek pad area on the helmet.
- Rescuer 1 then rotates the helmet forward while sliding the helmet off the patient's head, being mindful to not place the head into flexion or extension.
- Once the helmet is removed, manual inline stabilization should be returned to rescuer 1 and padding (such as a folded towel) should be placed under the patient's head.8 This padding will offset the height of the shoulder pads and prevent hyperextension, which can decrease space available for the cord.
- ATs and other rescue personnel should practice helmet removal with all types of helmets used at their venue.

Figure 9.26 Helmet removal: baseball catcher.
Courtesy of University of Georgia.
Traumatic injuries to the head and face: Subdural hematoma
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.2 Bleeding collects under the inner layer of the dura mater but external to the brain and arachnoid membrane. Subdural hematomas can become life-threatening very quickly.
Incidence and Epidemiology
A subdural hematoma results most often from a severe head injury. Acceleration-deceleration forces cause injuries as the patient's momentum is stopped suddenly by a solid object and the brain makes contact with the inside of the skull.2 Subdural hematomas can present either acutely or chronically based on the time since symptoms first appeared. Acute subdural hematomas occur within 72 hours after injury, while chronic subdural hematomas may take as long 3 weeks to show signs.
Risk Factors
Risk factors associated with acute subdural hematoma include head trauma, postsurgical complications, anticoagulation drug therapy, and nontraumatic cerebral aneurysm. As with epidural hematomas, decreased risk is associated with appropriate use of protective headgear in athletic environments.
Signs and Symptoms
Immediate medical referral and emergency management are recommended for any of the signs presented in the Red Flag box. Subsequent impacts to the head during the development of a chronic subdural hematoma may put patients at a higher risk of experiencing a life-threatening situation; as such, continued monitoring and serial assessment is important.
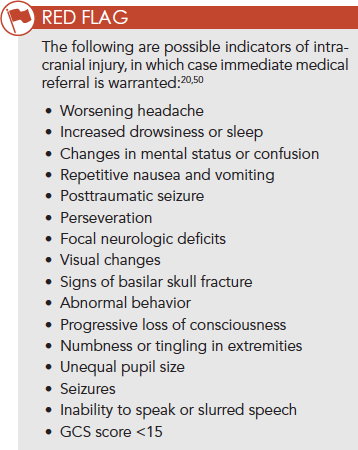
Field Assessment Techniques
In the pre-competition season, athletes participating in at-risk sports (e.g., football, soccer, rugby) should undergo baseline neurocognitive testing, either as a component of a pre-participation physical exam or an adjunct to such an exam. The importance of an established emergency care plan (ECP) cannot be overemphasized; the ECP provides for a standard of care and ensures rapid and efficient treatment measures are in place.
The Canadian CT Head Rule is a clinical prediction rule that uses CT scans to identify head injuries that could require neurosurgical intervention.55 Inclusion criteria include patients with a GCS score of 13 to 15; injury within 24 hours; and blunt head trauma resulting in loss of consciousness, definite amnesia, or disorientation. Exclusion criteria include patients under 16 years of age, nontraumatic cases, patients using anticoagulants or with a bleeding disorder, obvious skull fracture, GCS score of less than 13, and pregnancy.
Immediate Management Techniques
Emergency management of any sports-related injury should first address a primary survey assessment of the patient's mental status, followed by ensuring proper ABC. Knowledge of the patient's neurocognitive baseline may be critical for both short-term and long-term management, and it is helpful when conducting a sideline assessment. Although uncommon, possible differential diagnoses should include intracranial hemorrhage, because the signs and symptoms of a concussion and an intracranial injury are differentiated.50,56 Incorporating potential clinical signs of intracranial injury into the assessment of a patient with a suspected concussion is important.50 Injuries to the head can escalate into medical emergencies quickly, therefore an efficient process of providing immediate care based on signs and symptoms is required (figure 8.6).

Figure 8.6 Head injury algorithm.
Sternoclavicular joint injury
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton.
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton. This joint is a loose connection between the medial clavicle and manubrium of the superior sternum. It has a joint capsule, disc, and several ligaments in addition to the SC ligament—the intraclavicular ligament (between the two medial aspects of the clavicle, superior to the sternum) and the costoclavicular ligament, which maintains the stability of the clavicle on the ribs below. The SC joint is inherently unstable, and only a portion of the clavicle actually articulates with the manubrium, relying on the SC ligament to provide more stability.
Injury to the SC joint is one of the true medical emergencies in orthopedics. Just posterior to the joint lie the trachea and carotid arteries, and not too lateral from there, the subclavian arteries are located (figure 10.12). A posterior subluxation or dislocation can be a life-threatening emergency with compression on any of these structures.
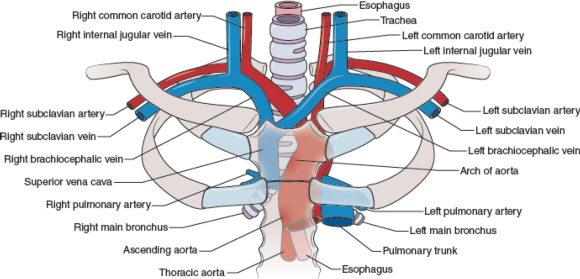
Figure 10.12 Internal structures behind the sternoclavicular (SC) joint.
Because of the SC's importance in connecting the arm to the body proper, the SC joint has many MOIs. One can fall on an outstretched hand or elbow, and the force can transmit along the bones of the arm, acromion of the scapula, and clavicle to the joint, injuring it. Another MOI is a fall on the lateral aspect of the shoulder (humerus or acromion of the scapula), or lying on one side with a pileup on the opposite lateral shoulder. In both of these situations, the force is transmitted along from the humerus/acromion to the clavicle and on to the biomechanically weakest aspect. The athlete could sprain the acromioclavicular joint or fracture the clavicle, or the force could continue medially and injure the SC joint at the sternum.
Incidence and Epidemiology
Injury to the sternoclavicular joint is rare, and posterior dislocations are more unusual. In a study of 251 SC dislocations, only 80 were posterior dislocations. Of the total number of dislocations (both anterior and posterior), the average age of the patient was 29 years old, and 67% of them were male.5 These data are consistent in other publications, in that younger males are more likely to sustain SC injuries than are other age groups or women.6
Risk Factors
Risk factors for injuring the SC joint include falling on an outstretched arm, elbow, or lateral shoulder. As noted, men under 30 years old tend to have higher incidences of SC injuries, so that population is at higher risk. Because high-velocity contact is a MOI, motor vehicle accidents are also a means of sustaining this injury.
Signs and Symptoms
When evaluating an injury to the upper extremity, it is important to be aware of the anatomical connection of the upper extremity and the SC joint. The athlete may initially feel more soreness at the point of impact (e.g., hand, elbow, shoulder) and not recognize the injury to the SC joint. Appreciating the MOI for a potential transmitted force to the medial clavicle and sternum is critical.
On inspection, a deformity may be present over the medial clavicle. It can range from mild swelling to gross deformity. A divot at the SC junction may indicate a posterior dislocation or subluxation, or a posterior fracture of the medial clavicular head (depending on the age of the athlete). Palpation results in a painful SC ligament or joint. Crepitus indicates a fracture, not dislocation or subluxation, but it is equally disconcerting.
Joint stress testing is not recommended, but sometimes the athlete presents with pain away from the SC joint, and that specific injury is not considered at the initial time of testing. The patient will present with an unwillingness to demonstrate full glenohumeral range of motion, because the stress on that joint affects the SC joint.
In a true posterior SC dislocation or subluxation, the patient may have dyspnea or hoarseness and relate difficulty swallowing, because the trachea is pushing posteriorly into the esophagus. If any of these complaints occur, consider it a medical emergency and transport via ambulance as soon as possible. On occasion, the patient will not identify the difficulty swallowing and hoarseness as related to the falling injury, and may not report these conditions. Anecdotal conversations with ATs indicate that athletes sometimes delay reporting issues of the voice or swallowing because they do not relate it to the SC sprain injury, only to have it be an emergency hours later when swelling increases and the airway begins to be compromised.
Field Assessment Techniques
Always assume a potential SC injury when presented with a mechanism consistent with the biomechanical weakness of the joint. Palpate all aspects of the clavicle, SC joint, and manubrium when evaluating falls resulting in landing on the outstretched hand, olecranon of the elbow, or acromion of scapula. If injury to the SC joint is suspected, assess airway and quality of voice. Ask the athlete to swallow, and query whether that action feels normal. Patients with swelling over the SC joint, who report that it is hard to swallow, or who have altered breath sounds, anxiety, or hoarseness should be removed from activity, have their shoulder pads removed (if wearing them), and be transported to the emergency department via ambulance. While waiting for transport, keep the athlete sitting up to facilitate breathing, and apply a sling to the affected arm. The sling will prevent unnecessary movement of the SC joint.
Reduction of the sternoclavicular joint is not recommended on the field. This procedure is performed under sedation or general anesthesia in an operating room. Open reduction and possible stabilization are necessary in situations of failed closed reduction or ongoing symptoms.7 Typically, surgical reduction of this injury is performed in conjunction with a cardiothoracic surgeon because of the potential for complications external to orthopedic surgery.
Diagnostic Accuracy
Standard radiographs of the SC joint are ineffective, because the X-rays are poor at viewing relevant anatomy of the joint.7 One technique that does provide better viewing is the serendipity view, which allows a 40° cephalic tilt.7 In this technique, an anterior dislocation presents as a superiorly displaced medial clavicle, and a posterior dislocation is represented as an inferiorly displaced medial clavicle.7 The preferred imaging is CT, which clearly defines the vascular and respiratory features that could be compromised.
Immediate Management Techniques
If the patient reports no difficulty with breathing or swallowing, but has swelling or tenderness over the SC joint, remove the patient from activity, place the affected arm in a sling, and reassess often. In this situation, ice may be held in place by the patient for 15- to 20-minute intervals if it relieves pain and swelling.
Indications
Dyspnea, hoarseness, or dysphagia following a collision or fall on an out stretched arm, elbow, or lateral shoulder are indications to transport the athlete via ambulance to the nearest ED.
Contraindications
Applying ice to the SC region after an acute injury may be contraindicated for a few reasons. The weight of the ice itself could put additional pressure on an unstable joint, further aggravating any dyspnea. Using a wrap to secure the ice to the area provides additional pressure to the area, which can actually worsen an unstable SC joint injury. The anatomical positioning of the trachea and major vessels from the heart immediately under the thin skin of the neck make ice an inappropriate treatment.
Criteria for Deciding to Transport for Further Medical Examination
Dyspnea, hoarseness, and difficulty swallowing following a collision or fall on an outstretched arm, elbow, or lateral shoulder are indications to transport the patient via ambulance to the nearest emergency department.
Transportation Techniques
Patients with a suspected posterior SC sprain should have supplemental oxygen available delivered via a nasal cannula. Transportation should occur in a recumbent position to facilitate easier respiration. A sling should be placed on the affected arm to relieve any traction of the SC joint from the weight of the upper extremity.
Heat-related emergencies in athletes
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS).
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS). EHS is the only true heat-related life-threatening emergency, and it is the only heat illness discussed here. As the name suggests, EHS is brought about by the combination of exertion (working out), temperature (including air and humidity), and other factors. A person can acclimate to the hot weather if given the time and cautiously increasing the activity duration slowly in the hot environment. Heatstroke is preventable in many aspects, including paying close attention to the weather (air temperature, ambient temperature, humidity, wind, sunshine), the heat and humidity trends in the local area, clothing and equipment worn, work-to-rest ratio, and hydration and food intake.13 Other salient factors include medical conditions, body mass, poor conditioning, medications, prior history of heat illness, and other predispositions that can exacerbate heat illness.14
Incidence and Epidemiology
Although the overall risk of EHS is low, its consequences can be fatal. According to the National Center for Catastrophic Sport Injury Research, 148 deaths have occurred since 1955 (56 since 1996) due to EHS in football.17 Rates are highest across all levels of football (youth, high school, and collegiate) during the preseason and lower during youth practices and high school games.18 Athletics are not alone in EHS injury; the U.S. military forces also have significant data. Fort Benning, Georgia and Fort Bragg, North Carolina led a 14-year study period with over 1,400 heat-related illnesses each, and nearly 3,500 incidents were reported from military bases in North and South Carolina combined (table 15.2).19
Medical Consequences
of Heatstroke
The systemic physiological effects of untreated EHS are many. The rising internal temperature denatures proteins and cellular membranes, causing an inflammatory response.20 As a reaction, the body relocates an aspect of bacteria usually found in the gastrointestinal system, which can promulgate a sepsis reaction systemically, and therefore begins a coagulation reaction throughout organs.20 Aside from death, EHS can elicit multi-organ failure, acute respiratory distress syndrome, and coma. Organ failure can become irreversible and the long-term sequelae catastrophic.
Signs and Symptoms
If the weather is hot or humid, be suspicious of EHS for any athlete who presents with any of these signs of symptoms. The 2 cardinal signs of EHS are a rectal temperature over 105°F (40.5°C) and central nervous system dysfunction, namely, concussion-like behaviors.21 Strictly from an observational standpoint, the athlete may be disoriented, confused, or dizzy, and his performance may be deteriorating. EHS patients tend to have diaphoretic and hot skin. The presence or absence of sweat should not be a deterrent to consider EHS, given other feedback. Complaints of muscular cramping, headache, weakness, or dry mouth are worth continued exploration. Nausea, vomiting, or diarrhea can occur prior to
collapse.14,20-23
Sudden collapse, seizure, altered consciousness, or coma can occur and will likely transpire if not rapidly diagnosed and treated.21,22 Vital signs can diminish with time, especially if the patient is untreated.
Field Assessment Techniques
A person who has heatstroke presents with concussion-like symptoms, which include confusion, stupor, dizziness, personality changes, and acting combative or complacent. A rapid decision must be made to assess core temperature using a rectal thermometer to diagnose EHS (figure 15.1). Every minute delay to diagnose EHS via rectal thermometry is critical.
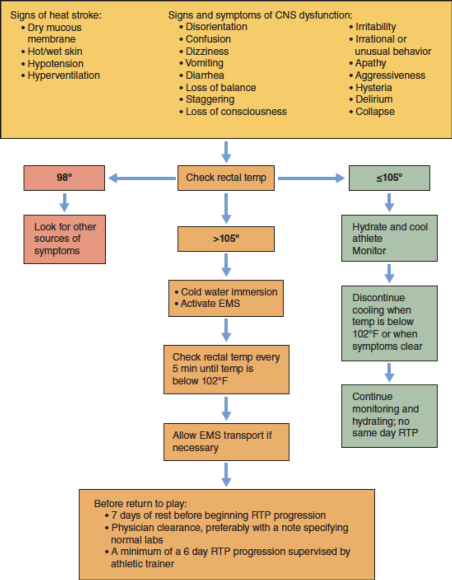
Figure 15.1 Decision tree for EHS.
Safe helmet removal after spinal injury
If the decision has been made to remove the athlete’s equipment, the helmet and shoulder pads should be considered a unit and both be removed.
If the decision has been made to remove the athlete's equipment, the helmet and shoulder pads should be considered a unit and both be removed. Once the face mask has been removed, the helmet can be removed from the injured patient. Less motion in the cervical spine is generated when the face mask is removed from the football helmet prior to removing the helmet.95 Removal of the face mask allows for easier access to stabilize the cervical spine. However, circumstances may arise where the face mask cannot be removed. The sports medicine team should be prepared to remove the helmet under both conditions. Figures 9.24 and 9.25 demonstrate helmet removal with the face mask off and on, respectively. When working with lacrosse, hockey, or other types of helmets, different considerations may need to be made.96-98If time is of the essence, consider leaving the face mask on and simply removing the helmet with the face mask attached.

Figure 9.24 Helmet removal with no face mask.
Courtesy of University of Georgia.

Figure 9.25 Helmet removal with face mask.
Courtesy of University of Georgia.
Here are some tips for helmet removal:
- The chin strap should be cut away, because unsnapping the helmet may create unnecessary movement.
- Cheek pads should be removed from the helmet using a tongue depressor (or something similar) to snap the pad away from the inside of the helmet. However, the ability to remove the cheek pads varies based on the model of the helmet.
- If possible, air bladders in the helmet should be deflated to loosen the fit on the helmet on the patient's head.
- Before the removing the helmet:
- Manual inline stabilization should be transferred from the rescuer at the patient's head (rescuer 1) to rescuer 2, who can provide inline stabilization from the front of the patient.
- Rescuer 2 places 1 hand on the chin and the other hand on the posterior side of the patient's neck (or as depicted in figure 9.26, on either side of the patient's head).
- Rescuer 1, located at the head, grasps the side of the helmet while slightly spreading the cheek pad area on the helmet.
- Rescuer 1 then rotates the helmet forward while sliding the helmet off the patient's head, being mindful to not place the head into flexion or extension.
- Once the helmet is removed, manual inline stabilization should be returned to rescuer 1 and padding (such as a folded towel) should be placed under the patient's head.8 This padding will offset the height of the shoulder pads and prevent hyperextension, which can decrease space available for the cord.
- ATs and other rescue personnel should practice helmet removal with all types of helmets used at their venue.

Figure 9.26 Helmet removal: baseball catcher.
Courtesy of University of Georgia.
Traumatic injuries to the head and face: Subdural hematoma
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.2 Bleeding collects under the inner layer of the dura mater but external to the brain and arachnoid membrane. Subdural hematomas can become life-threatening very quickly.
Incidence and Epidemiology
A subdural hematoma results most often from a severe head injury. Acceleration-deceleration forces cause injuries as the patient's momentum is stopped suddenly by a solid object and the brain makes contact with the inside of the skull.2 Subdural hematomas can present either acutely or chronically based on the time since symptoms first appeared. Acute subdural hematomas occur within 72 hours after injury, while chronic subdural hematomas may take as long 3 weeks to show signs.
Risk Factors
Risk factors associated with acute subdural hematoma include head trauma, postsurgical complications, anticoagulation drug therapy, and nontraumatic cerebral aneurysm. As with epidural hematomas, decreased risk is associated with appropriate use of protective headgear in athletic environments.
Signs and Symptoms
Immediate medical referral and emergency management are recommended for any of the signs presented in the Red Flag box. Subsequent impacts to the head during the development of a chronic subdural hematoma may put patients at a higher risk of experiencing a life-threatening situation; as such, continued monitoring and serial assessment is important.
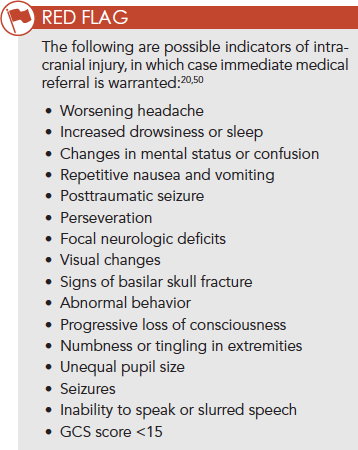
Field Assessment Techniques
In the pre-competition season, athletes participating in at-risk sports (e.g., football, soccer, rugby) should undergo baseline neurocognitive testing, either as a component of a pre-participation physical exam or an adjunct to such an exam. The importance of an established emergency care plan (ECP) cannot be overemphasized; the ECP provides for a standard of care and ensures rapid and efficient treatment measures are in place.
The Canadian CT Head Rule is a clinical prediction rule that uses CT scans to identify head injuries that could require neurosurgical intervention.55 Inclusion criteria include patients with a GCS score of 13 to 15; injury within 24 hours; and blunt head trauma resulting in loss of consciousness, definite amnesia, or disorientation. Exclusion criteria include patients under 16 years of age, nontraumatic cases, patients using anticoagulants or with a bleeding disorder, obvious skull fracture, GCS score of less than 13, and pregnancy.
Immediate Management Techniques
Emergency management of any sports-related injury should first address a primary survey assessment of the patient's mental status, followed by ensuring proper ABC. Knowledge of the patient's neurocognitive baseline may be critical for both short-term and long-term management, and it is helpful when conducting a sideline assessment. Although uncommon, possible differential diagnoses should include intracranial hemorrhage, because the signs and symptoms of a concussion and an intracranial injury are differentiated.50,56 Incorporating potential clinical signs of intracranial injury into the assessment of a patient with a suspected concussion is important.50 Injuries to the head can escalate into medical emergencies quickly, therefore an efficient process of providing immediate care based on signs and symptoms is required (figure 8.6).

Figure 8.6 Head injury algorithm.
Sternoclavicular joint injury
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton.
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton. This joint is a loose connection between the medial clavicle and manubrium of the superior sternum. It has a joint capsule, disc, and several ligaments in addition to the SC ligament—the intraclavicular ligament (between the two medial aspects of the clavicle, superior to the sternum) and the costoclavicular ligament, which maintains the stability of the clavicle on the ribs below. The SC joint is inherently unstable, and only a portion of the clavicle actually articulates with the manubrium, relying on the SC ligament to provide more stability.
Injury to the SC joint is one of the true medical emergencies in orthopedics. Just posterior to the joint lie the trachea and carotid arteries, and not too lateral from there, the subclavian arteries are located (figure 10.12). A posterior subluxation or dislocation can be a life-threatening emergency with compression on any of these structures.
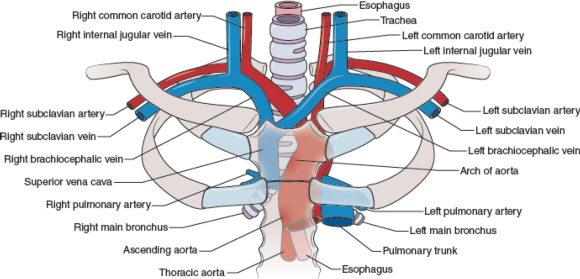
Figure 10.12 Internal structures behind the sternoclavicular (SC) joint.
Because of the SC's importance in connecting the arm to the body proper, the SC joint has many MOIs. One can fall on an outstretched hand or elbow, and the force can transmit along the bones of the arm, acromion of the scapula, and clavicle to the joint, injuring it. Another MOI is a fall on the lateral aspect of the shoulder (humerus or acromion of the scapula), or lying on one side with a pileup on the opposite lateral shoulder. In both of these situations, the force is transmitted along from the humerus/acromion to the clavicle and on to the biomechanically weakest aspect. The athlete could sprain the acromioclavicular joint or fracture the clavicle, or the force could continue medially and injure the SC joint at the sternum.
Incidence and Epidemiology
Injury to the sternoclavicular joint is rare, and posterior dislocations are more unusual. In a study of 251 SC dislocations, only 80 were posterior dislocations. Of the total number of dislocations (both anterior and posterior), the average age of the patient was 29 years old, and 67% of them were male.5 These data are consistent in other publications, in that younger males are more likely to sustain SC injuries than are other age groups or women.6
Risk Factors
Risk factors for injuring the SC joint include falling on an outstretched arm, elbow, or lateral shoulder. As noted, men under 30 years old tend to have higher incidences of SC injuries, so that population is at higher risk. Because high-velocity contact is a MOI, motor vehicle accidents are also a means of sustaining this injury.
Signs and Symptoms
When evaluating an injury to the upper extremity, it is important to be aware of the anatomical connection of the upper extremity and the SC joint. The athlete may initially feel more soreness at the point of impact (e.g., hand, elbow, shoulder) and not recognize the injury to the SC joint. Appreciating the MOI for a potential transmitted force to the medial clavicle and sternum is critical.
On inspection, a deformity may be present over the medial clavicle. It can range from mild swelling to gross deformity. A divot at the SC junction may indicate a posterior dislocation or subluxation, or a posterior fracture of the medial clavicular head (depending on the age of the athlete). Palpation results in a painful SC ligament or joint. Crepitus indicates a fracture, not dislocation or subluxation, but it is equally disconcerting.
Joint stress testing is not recommended, but sometimes the athlete presents with pain away from the SC joint, and that specific injury is not considered at the initial time of testing. The patient will present with an unwillingness to demonstrate full glenohumeral range of motion, because the stress on that joint affects the SC joint.
In a true posterior SC dislocation or subluxation, the patient may have dyspnea or hoarseness and relate difficulty swallowing, because the trachea is pushing posteriorly into the esophagus. If any of these complaints occur, consider it a medical emergency and transport via ambulance as soon as possible. On occasion, the patient will not identify the difficulty swallowing and hoarseness as related to the falling injury, and may not report these conditions. Anecdotal conversations with ATs indicate that athletes sometimes delay reporting issues of the voice or swallowing because they do not relate it to the SC sprain injury, only to have it be an emergency hours later when swelling increases and the airway begins to be compromised.
Field Assessment Techniques
Always assume a potential SC injury when presented with a mechanism consistent with the biomechanical weakness of the joint. Palpate all aspects of the clavicle, SC joint, and manubrium when evaluating falls resulting in landing on the outstretched hand, olecranon of the elbow, or acromion of scapula. If injury to the SC joint is suspected, assess airway and quality of voice. Ask the athlete to swallow, and query whether that action feels normal. Patients with swelling over the SC joint, who report that it is hard to swallow, or who have altered breath sounds, anxiety, or hoarseness should be removed from activity, have their shoulder pads removed (if wearing them), and be transported to the emergency department via ambulance. While waiting for transport, keep the athlete sitting up to facilitate breathing, and apply a sling to the affected arm. The sling will prevent unnecessary movement of the SC joint.
Reduction of the sternoclavicular joint is not recommended on the field. This procedure is performed under sedation or general anesthesia in an operating room. Open reduction and possible stabilization are necessary in situations of failed closed reduction or ongoing symptoms.7 Typically, surgical reduction of this injury is performed in conjunction with a cardiothoracic surgeon because of the potential for complications external to orthopedic surgery.
Diagnostic Accuracy
Standard radiographs of the SC joint are ineffective, because the X-rays are poor at viewing relevant anatomy of the joint.7 One technique that does provide better viewing is the serendipity view, which allows a 40° cephalic tilt.7 In this technique, an anterior dislocation presents as a superiorly displaced medial clavicle, and a posterior dislocation is represented as an inferiorly displaced medial clavicle.7 The preferred imaging is CT, which clearly defines the vascular and respiratory features that could be compromised.
Immediate Management Techniques
If the patient reports no difficulty with breathing or swallowing, but has swelling or tenderness over the SC joint, remove the patient from activity, place the affected arm in a sling, and reassess often. In this situation, ice may be held in place by the patient for 15- to 20-minute intervals if it relieves pain and swelling.
Indications
Dyspnea, hoarseness, or dysphagia following a collision or fall on an out stretched arm, elbow, or lateral shoulder are indications to transport the athlete via ambulance to the nearest ED.
Contraindications
Applying ice to the SC region after an acute injury may be contraindicated for a few reasons. The weight of the ice itself could put additional pressure on an unstable joint, further aggravating any dyspnea. Using a wrap to secure the ice to the area provides additional pressure to the area, which can actually worsen an unstable SC joint injury. The anatomical positioning of the trachea and major vessels from the heart immediately under the thin skin of the neck make ice an inappropriate treatment.
Criteria for Deciding to Transport for Further Medical Examination
Dyspnea, hoarseness, and difficulty swallowing following a collision or fall on an outstretched arm, elbow, or lateral shoulder are indications to transport the patient via ambulance to the nearest emergency department.
Transportation Techniques
Patients with a suspected posterior SC sprain should have supplemental oxygen available delivered via a nasal cannula. Transportation should occur in a recumbent position to facilitate easier respiration. A sling should be placed on the affected arm to relieve any traction of the SC joint from the weight of the upper extremity.
Heat-related emergencies in athletes
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS).
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS). EHS is the only true heat-related life-threatening emergency, and it is the only heat illness discussed here. As the name suggests, EHS is brought about by the combination of exertion (working out), temperature (including air and humidity), and other factors. A person can acclimate to the hot weather if given the time and cautiously increasing the activity duration slowly in the hot environment. Heatstroke is preventable in many aspects, including paying close attention to the weather (air temperature, ambient temperature, humidity, wind, sunshine), the heat and humidity trends in the local area, clothing and equipment worn, work-to-rest ratio, and hydration and food intake.13 Other salient factors include medical conditions, body mass, poor conditioning, medications, prior history of heat illness, and other predispositions that can exacerbate heat illness.14
Incidence and Epidemiology
Although the overall risk of EHS is low, its consequences can be fatal. According to the National Center for Catastrophic Sport Injury Research, 148 deaths have occurred since 1955 (56 since 1996) due to EHS in football.17 Rates are highest across all levels of football (youth, high school, and collegiate) during the preseason and lower during youth practices and high school games.18 Athletics are not alone in EHS injury; the U.S. military forces also have significant data. Fort Benning, Georgia and Fort Bragg, North Carolina led a 14-year study period with over 1,400 heat-related illnesses each, and nearly 3,500 incidents were reported from military bases in North and South Carolina combined (table 15.2).19
Medical Consequences
of Heatstroke
The systemic physiological effects of untreated EHS are many. The rising internal temperature denatures proteins and cellular membranes, causing an inflammatory response.20 As a reaction, the body relocates an aspect of bacteria usually found in the gastrointestinal system, which can promulgate a sepsis reaction systemically, and therefore begins a coagulation reaction throughout organs.20 Aside from death, EHS can elicit multi-organ failure, acute respiratory distress syndrome, and coma. Organ failure can become irreversible and the long-term sequelae catastrophic.
Signs and Symptoms
If the weather is hot or humid, be suspicious of EHS for any athlete who presents with any of these signs of symptoms. The 2 cardinal signs of EHS are a rectal temperature over 105°F (40.5°C) and central nervous system dysfunction, namely, concussion-like behaviors.21 Strictly from an observational standpoint, the athlete may be disoriented, confused, or dizzy, and his performance may be deteriorating. EHS patients tend to have diaphoretic and hot skin. The presence or absence of sweat should not be a deterrent to consider EHS, given other feedback. Complaints of muscular cramping, headache, weakness, or dry mouth are worth continued exploration. Nausea, vomiting, or diarrhea can occur prior to
collapse.14,20-23
Sudden collapse, seizure, altered consciousness, or coma can occur and will likely transpire if not rapidly diagnosed and treated.21,22 Vital signs can diminish with time, especially if the patient is untreated.
Field Assessment Techniques
A person who has heatstroke presents with concussion-like symptoms, which include confusion, stupor, dizziness, personality changes, and acting combative or complacent. A rapid decision must be made to assess core temperature using a rectal thermometer to diagnose EHS (figure 15.1). Every minute delay to diagnose EHS via rectal thermometry is critical.
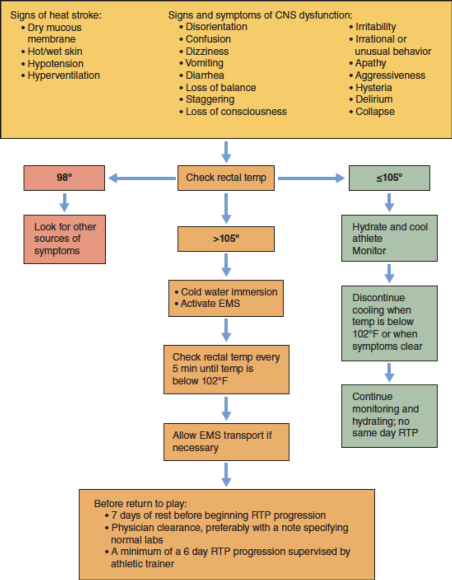
Figure 15.1 Decision tree for EHS.
Safe helmet removal after spinal injury
If the decision has been made to remove the athlete’s equipment, the helmet and shoulder pads should be considered a unit and both be removed.
If the decision has been made to remove the athlete's equipment, the helmet and shoulder pads should be considered a unit and both be removed. Once the face mask has been removed, the helmet can be removed from the injured patient. Less motion in the cervical spine is generated when the face mask is removed from the football helmet prior to removing the helmet.95 Removal of the face mask allows for easier access to stabilize the cervical spine. However, circumstances may arise where the face mask cannot be removed. The sports medicine team should be prepared to remove the helmet under both conditions. Figures 9.24 and 9.25 demonstrate helmet removal with the face mask off and on, respectively. When working with lacrosse, hockey, or other types of helmets, different considerations may need to be made.96-98If time is of the essence, consider leaving the face mask on and simply removing the helmet with the face mask attached.

Figure 9.24 Helmet removal with no face mask.
Courtesy of University of Georgia.

Figure 9.25 Helmet removal with face mask.
Courtesy of University of Georgia.
Here are some tips for helmet removal:
- The chin strap should be cut away, because unsnapping the helmet may create unnecessary movement.
- Cheek pads should be removed from the helmet using a tongue depressor (or something similar) to snap the pad away from the inside of the helmet. However, the ability to remove the cheek pads varies based on the model of the helmet.
- If possible, air bladders in the helmet should be deflated to loosen the fit on the helmet on the patient's head.
- Before the removing the helmet:
- Manual inline stabilization should be transferred from the rescuer at the patient's head (rescuer 1) to rescuer 2, who can provide inline stabilization from the front of the patient.
- Rescuer 2 places 1 hand on the chin and the other hand on the posterior side of the patient's neck (or as depicted in figure 9.26, on either side of the patient's head).
- Rescuer 1, located at the head, grasps the side of the helmet while slightly spreading the cheek pad area on the helmet.
- Rescuer 1 then rotates the helmet forward while sliding the helmet off the patient's head, being mindful to not place the head into flexion or extension.
- Once the helmet is removed, manual inline stabilization should be returned to rescuer 1 and padding (such as a folded towel) should be placed under the patient's head.8 This padding will offset the height of the shoulder pads and prevent hyperextension, which can decrease space available for the cord.
- ATs and other rescue personnel should practice helmet removal with all types of helmets used at their venue.

Figure 9.26 Helmet removal: baseball catcher.
Courtesy of University of Georgia.
Traumatic injuries to the head and face: Subdural hematoma
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.2 Bleeding collects under the inner layer of the dura mater but external to the brain and arachnoid membrane. Subdural hematomas can become life-threatening very quickly.
Incidence and Epidemiology
A subdural hematoma results most often from a severe head injury. Acceleration-deceleration forces cause injuries as the patient's momentum is stopped suddenly by a solid object and the brain makes contact with the inside of the skull.2 Subdural hematomas can present either acutely or chronically based on the time since symptoms first appeared. Acute subdural hematomas occur within 72 hours after injury, while chronic subdural hematomas may take as long 3 weeks to show signs.
Risk Factors
Risk factors associated with acute subdural hematoma include head trauma, postsurgical complications, anticoagulation drug therapy, and nontraumatic cerebral aneurysm. As with epidural hematomas, decreased risk is associated with appropriate use of protective headgear in athletic environments.
Signs and Symptoms
Immediate medical referral and emergency management are recommended for any of the signs presented in the Red Flag box. Subsequent impacts to the head during the development of a chronic subdural hematoma may put patients at a higher risk of experiencing a life-threatening situation; as such, continued monitoring and serial assessment is important.
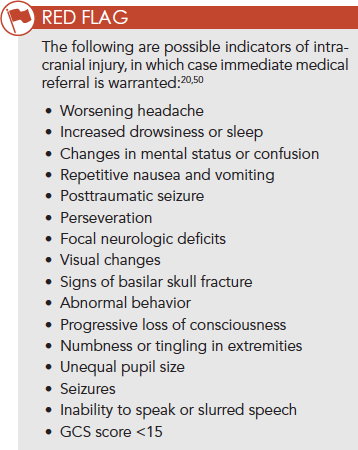
Field Assessment Techniques
In the pre-competition season, athletes participating in at-risk sports (e.g., football, soccer, rugby) should undergo baseline neurocognitive testing, either as a component of a pre-participation physical exam or an adjunct to such an exam. The importance of an established emergency care plan (ECP) cannot be overemphasized; the ECP provides for a standard of care and ensures rapid and efficient treatment measures are in place.
The Canadian CT Head Rule is a clinical prediction rule that uses CT scans to identify head injuries that could require neurosurgical intervention.55 Inclusion criteria include patients with a GCS score of 13 to 15; injury within 24 hours; and blunt head trauma resulting in loss of consciousness, definite amnesia, or disorientation. Exclusion criteria include patients under 16 years of age, nontraumatic cases, patients using anticoagulants or with a bleeding disorder, obvious skull fracture, GCS score of less than 13, and pregnancy.
Immediate Management Techniques
Emergency management of any sports-related injury should first address a primary survey assessment of the patient's mental status, followed by ensuring proper ABC. Knowledge of the patient's neurocognitive baseline may be critical for both short-term and long-term management, and it is helpful when conducting a sideline assessment. Although uncommon, possible differential diagnoses should include intracranial hemorrhage, because the signs and symptoms of a concussion and an intracranial injury are differentiated.50,56 Incorporating potential clinical signs of intracranial injury into the assessment of a patient with a suspected concussion is important.50 Injuries to the head can escalate into medical emergencies quickly, therefore an efficient process of providing immediate care based on signs and symptoms is required (figure 8.6).

Figure 8.6 Head injury algorithm.
Sternoclavicular joint injury
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton.
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton. This joint is a loose connection between the medial clavicle and manubrium of the superior sternum. It has a joint capsule, disc, and several ligaments in addition to the SC ligament—the intraclavicular ligament (between the two medial aspects of the clavicle, superior to the sternum) and the costoclavicular ligament, which maintains the stability of the clavicle on the ribs below. The SC joint is inherently unstable, and only a portion of the clavicle actually articulates with the manubrium, relying on the SC ligament to provide more stability.
Injury to the SC joint is one of the true medical emergencies in orthopedics. Just posterior to the joint lie the trachea and carotid arteries, and not too lateral from there, the subclavian arteries are located (figure 10.12). A posterior subluxation or dislocation can be a life-threatening emergency with compression on any of these structures.
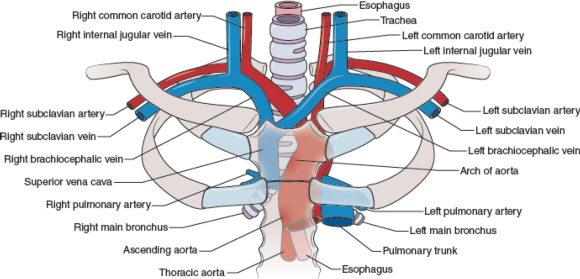
Figure 10.12 Internal structures behind the sternoclavicular (SC) joint.
Because of the SC's importance in connecting the arm to the body proper, the SC joint has many MOIs. One can fall on an outstretched hand or elbow, and the force can transmit along the bones of the arm, acromion of the scapula, and clavicle to the joint, injuring it. Another MOI is a fall on the lateral aspect of the shoulder (humerus or acromion of the scapula), or lying on one side with a pileup on the opposite lateral shoulder. In both of these situations, the force is transmitted along from the humerus/acromion to the clavicle and on to the biomechanically weakest aspect. The athlete could sprain the acromioclavicular joint or fracture the clavicle, or the force could continue medially and injure the SC joint at the sternum.
Incidence and Epidemiology
Injury to the sternoclavicular joint is rare, and posterior dislocations are more unusual. In a study of 251 SC dislocations, only 80 were posterior dislocations. Of the total number of dislocations (both anterior and posterior), the average age of the patient was 29 years old, and 67% of them were male.5 These data are consistent in other publications, in that younger males are more likely to sustain SC injuries than are other age groups or women.6
Risk Factors
Risk factors for injuring the SC joint include falling on an outstretched arm, elbow, or lateral shoulder. As noted, men under 30 years old tend to have higher incidences of SC injuries, so that population is at higher risk. Because high-velocity contact is a MOI, motor vehicle accidents are also a means of sustaining this injury.
Signs and Symptoms
When evaluating an injury to the upper extremity, it is important to be aware of the anatomical connection of the upper extremity and the SC joint. The athlete may initially feel more soreness at the point of impact (e.g., hand, elbow, shoulder) and not recognize the injury to the SC joint. Appreciating the MOI for a potential transmitted force to the medial clavicle and sternum is critical.
On inspection, a deformity may be present over the medial clavicle. It can range from mild swelling to gross deformity. A divot at the SC junction may indicate a posterior dislocation or subluxation, or a posterior fracture of the medial clavicular head (depending on the age of the athlete). Palpation results in a painful SC ligament or joint. Crepitus indicates a fracture, not dislocation or subluxation, but it is equally disconcerting.
Joint stress testing is not recommended, but sometimes the athlete presents with pain away from the SC joint, and that specific injury is not considered at the initial time of testing. The patient will present with an unwillingness to demonstrate full glenohumeral range of motion, because the stress on that joint affects the SC joint.
In a true posterior SC dislocation or subluxation, the patient may have dyspnea or hoarseness and relate difficulty swallowing, because the trachea is pushing posteriorly into the esophagus. If any of these complaints occur, consider it a medical emergency and transport via ambulance as soon as possible. On occasion, the patient will not identify the difficulty swallowing and hoarseness as related to the falling injury, and may not report these conditions. Anecdotal conversations with ATs indicate that athletes sometimes delay reporting issues of the voice or swallowing because they do not relate it to the SC sprain injury, only to have it be an emergency hours later when swelling increases and the airway begins to be compromised.
Field Assessment Techniques
Always assume a potential SC injury when presented with a mechanism consistent with the biomechanical weakness of the joint. Palpate all aspects of the clavicle, SC joint, and manubrium when evaluating falls resulting in landing on the outstretched hand, olecranon of the elbow, or acromion of scapula. If injury to the SC joint is suspected, assess airway and quality of voice. Ask the athlete to swallow, and query whether that action feels normal. Patients with swelling over the SC joint, who report that it is hard to swallow, or who have altered breath sounds, anxiety, or hoarseness should be removed from activity, have their shoulder pads removed (if wearing them), and be transported to the emergency department via ambulance. While waiting for transport, keep the athlete sitting up to facilitate breathing, and apply a sling to the affected arm. The sling will prevent unnecessary movement of the SC joint.
Reduction of the sternoclavicular joint is not recommended on the field. This procedure is performed under sedation or general anesthesia in an operating room. Open reduction and possible stabilization are necessary in situations of failed closed reduction or ongoing symptoms.7 Typically, surgical reduction of this injury is performed in conjunction with a cardiothoracic surgeon because of the potential for complications external to orthopedic surgery.
Diagnostic Accuracy
Standard radiographs of the SC joint are ineffective, because the X-rays are poor at viewing relevant anatomy of the joint.7 One technique that does provide better viewing is the serendipity view, which allows a 40° cephalic tilt.7 In this technique, an anterior dislocation presents as a superiorly displaced medial clavicle, and a posterior dislocation is represented as an inferiorly displaced medial clavicle.7 The preferred imaging is CT, which clearly defines the vascular and respiratory features that could be compromised.
Immediate Management Techniques
If the patient reports no difficulty with breathing or swallowing, but has swelling or tenderness over the SC joint, remove the patient from activity, place the affected arm in a sling, and reassess often. In this situation, ice may be held in place by the patient for 15- to 20-minute intervals if it relieves pain and swelling.
Indications
Dyspnea, hoarseness, or dysphagia following a collision or fall on an out stretched arm, elbow, or lateral shoulder are indications to transport the athlete via ambulance to the nearest ED.
Contraindications
Applying ice to the SC region after an acute injury may be contraindicated for a few reasons. The weight of the ice itself could put additional pressure on an unstable joint, further aggravating any dyspnea. Using a wrap to secure the ice to the area provides additional pressure to the area, which can actually worsen an unstable SC joint injury. The anatomical positioning of the trachea and major vessels from the heart immediately under the thin skin of the neck make ice an inappropriate treatment.
Criteria for Deciding to Transport for Further Medical Examination
Dyspnea, hoarseness, and difficulty swallowing following a collision or fall on an outstretched arm, elbow, or lateral shoulder are indications to transport the patient via ambulance to the nearest emergency department.
Transportation Techniques
Patients with a suspected posterior SC sprain should have supplemental oxygen available delivered via a nasal cannula. Transportation should occur in a recumbent position to facilitate easier respiration. A sling should be placed on the affected arm to relieve any traction of the SC joint from the weight of the upper extremity.
Heat-related emergencies in athletes
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS).
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS). EHS is the only true heat-related life-threatening emergency, and it is the only heat illness discussed here. As the name suggests, EHS is brought about by the combination of exertion (working out), temperature (including air and humidity), and other factors. A person can acclimate to the hot weather if given the time and cautiously increasing the activity duration slowly in the hot environment. Heatstroke is preventable in many aspects, including paying close attention to the weather (air temperature, ambient temperature, humidity, wind, sunshine), the heat and humidity trends in the local area, clothing and equipment worn, work-to-rest ratio, and hydration and food intake.13 Other salient factors include medical conditions, body mass, poor conditioning, medications, prior history of heat illness, and other predispositions that can exacerbate heat illness.14
Incidence and Epidemiology
Although the overall risk of EHS is low, its consequences can be fatal. According to the National Center for Catastrophic Sport Injury Research, 148 deaths have occurred since 1955 (56 since 1996) due to EHS in football.17 Rates are highest across all levels of football (youth, high school, and collegiate) during the preseason and lower during youth practices and high school games.18 Athletics are not alone in EHS injury; the U.S. military forces also have significant data. Fort Benning, Georgia and Fort Bragg, North Carolina led a 14-year study period with over 1,400 heat-related illnesses each, and nearly 3,500 incidents were reported from military bases in North and South Carolina combined (table 15.2).19
Medical Consequences
of Heatstroke
The systemic physiological effects of untreated EHS are many. The rising internal temperature denatures proteins and cellular membranes, causing an inflammatory response.20 As a reaction, the body relocates an aspect of bacteria usually found in the gastrointestinal system, which can promulgate a sepsis reaction systemically, and therefore begins a coagulation reaction throughout organs.20 Aside from death, EHS can elicit multi-organ failure, acute respiratory distress syndrome, and coma. Organ failure can become irreversible and the long-term sequelae catastrophic.
Signs and Symptoms
If the weather is hot or humid, be suspicious of EHS for any athlete who presents with any of these signs of symptoms. The 2 cardinal signs of EHS are a rectal temperature over 105°F (40.5°C) and central nervous system dysfunction, namely, concussion-like behaviors.21 Strictly from an observational standpoint, the athlete may be disoriented, confused, or dizzy, and his performance may be deteriorating. EHS patients tend to have diaphoretic and hot skin. The presence or absence of sweat should not be a deterrent to consider EHS, given other feedback. Complaints of muscular cramping, headache, weakness, or dry mouth are worth continued exploration. Nausea, vomiting, or diarrhea can occur prior to
collapse.14,20-23
Sudden collapse, seizure, altered consciousness, or coma can occur and will likely transpire if not rapidly diagnosed and treated.21,22 Vital signs can diminish with time, especially if the patient is untreated.
Field Assessment Techniques
A person who has heatstroke presents with concussion-like symptoms, which include confusion, stupor, dizziness, personality changes, and acting combative or complacent. A rapid decision must be made to assess core temperature using a rectal thermometer to diagnose EHS (figure 15.1). Every minute delay to diagnose EHS via rectal thermometry is critical.
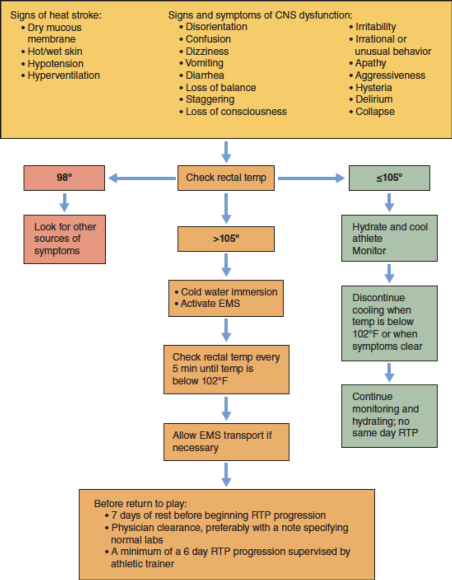
Figure 15.1 Decision tree for EHS.
Safe helmet removal after spinal injury
If the decision has been made to remove the athlete’s equipment, the helmet and shoulder pads should be considered a unit and both be removed.
If the decision has been made to remove the athlete's equipment, the helmet and shoulder pads should be considered a unit and both be removed. Once the face mask has been removed, the helmet can be removed from the injured patient. Less motion in the cervical spine is generated when the face mask is removed from the football helmet prior to removing the helmet.95 Removal of the face mask allows for easier access to stabilize the cervical spine. However, circumstances may arise where the face mask cannot be removed. The sports medicine team should be prepared to remove the helmet under both conditions. Figures 9.24 and 9.25 demonstrate helmet removal with the face mask off and on, respectively. When working with lacrosse, hockey, or other types of helmets, different considerations may need to be made.96-98If time is of the essence, consider leaving the face mask on and simply removing the helmet with the face mask attached.

Figure 9.24 Helmet removal with no face mask.
Courtesy of University of Georgia.

Figure 9.25 Helmet removal with face mask.
Courtesy of University of Georgia.
Here are some tips for helmet removal:
- The chin strap should be cut away, because unsnapping the helmet may create unnecessary movement.
- Cheek pads should be removed from the helmet using a tongue depressor (or something similar) to snap the pad away from the inside of the helmet. However, the ability to remove the cheek pads varies based on the model of the helmet.
- If possible, air bladders in the helmet should be deflated to loosen the fit on the helmet on the patient's head.
- Before the removing the helmet:
- Manual inline stabilization should be transferred from the rescuer at the patient's head (rescuer 1) to rescuer 2, who can provide inline stabilization from the front of the patient.
- Rescuer 2 places 1 hand on the chin and the other hand on the posterior side of the patient's neck (or as depicted in figure 9.26, on either side of the patient's head).
- Rescuer 1, located at the head, grasps the side of the helmet while slightly spreading the cheek pad area on the helmet.
- Rescuer 1 then rotates the helmet forward while sliding the helmet off the patient's head, being mindful to not place the head into flexion or extension.
- Once the helmet is removed, manual inline stabilization should be returned to rescuer 1 and padding (such as a folded towel) should be placed under the patient's head.8 This padding will offset the height of the shoulder pads and prevent hyperextension, which can decrease space available for the cord.
- ATs and other rescue personnel should practice helmet removal with all types of helmets used at their venue.

Figure 9.26 Helmet removal: baseball catcher.
Courtesy of University of Georgia.
Traumatic injuries to the head and face: Subdural hematoma
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.2 Bleeding collects under the inner layer of the dura mater but external to the brain and arachnoid membrane. Subdural hematomas can become life-threatening very quickly.
Incidence and Epidemiology
A subdural hematoma results most often from a severe head injury. Acceleration-deceleration forces cause injuries as the patient's momentum is stopped suddenly by a solid object and the brain makes contact with the inside of the skull.2 Subdural hematomas can present either acutely or chronically based on the time since symptoms first appeared. Acute subdural hematomas occur within 72 hours after injury, while chronic subdural hematomas may take as long 3 weeks to show signs.
Risk Factors
Risk factors associated with acute subdural hematoma include head trauma, postsurgical complications, anticoagulation drug therapy, and nontraumatic cerebral aneurysm. As with epidural hematomas, decreased risk is associated with appropriate use of protective headgear in athletic environments.
Signs and Symptoms
Immediate medical referral and emergency management are recommended for any of the signs presented in the Red Flag box. Subsequent impacts to the head during the development of a chronic subdural hematoma may put patients at a higher risk of experiencing a life-threatening situation; as such, continued monitoring and serial assessment is important.
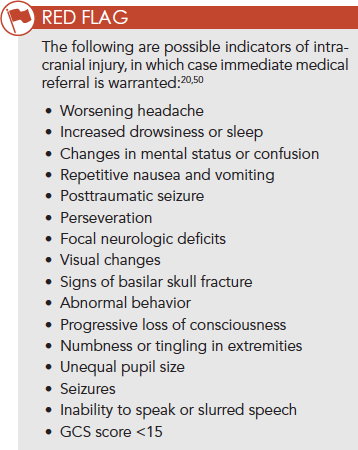
Field Assessment Techniques
In the pre-competition season, athletes participating in at-risk sports (e.g., football, soccer, rugby) should undergo baseline neurocognitive testing, either as a component of a pre-participation physical exam or an adjunct to such an exam. The importance of an established emergency care plan (ECP) cannot be overemphasized; the ECP provides for a standard of care and ensures rapid and efficient treatment measures are in place.
The Canadian CT Head Rule is a clinical prediction rule that uses CT scans to identify head injuries that could require neurosurgical intervention.55 Inclusion criteria include patients with a GCS score of 13 to 15; injury within 24 hours; and blunt head trauma resulting in loss of consciousness, definite amnesia, or disorientation. Exclusion criteria include patients under 16 years of age, nontraumatic cases, patients using anticoagulants or with a bleeding disorder, obvious skull fracture, GCS score of less than 13, and pregnancy.
Immediate Management Techniques
Emergency management of any sports-related injury should first address a primary survey assessment of the patient's mental status, followed by ensuring proper ABC. Knowledge of the patient's neurocognitive baseline may be critical for both short-term and long-term management, and it is helpful when conducting a sideline assessment. Although uncommon, possible differential diagnoses should include intracranial hemorrhage, because the signs and symptoms of a concussion and an intracranial injury are differentiated.50,56 Incorporating potential clinical signs of intracranial injury into the assessment of a patient with a suspected concussion is important.50 Injuries to the head can escalate into medical emergencies quickly, therefore an efficient process of providing immediate care based on signs and symptoms is required (figure 8.6).

Figure 8.6 Head injury algorithm.
Sternoclavicular joint injury
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton.
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton. This joint is a loose connection between the medial clavicle and manubrium of the superior sternum. It has a joint capsule, disc, and several ligaments in addition to the SC ligament—the intraclavicular ligament (between the two medial aspects of the clavicle, superior to the sternum) and the costoclavicular ligament, which maintains the stability of the clavicle on the ribs below. The SC joint is inherently unstable, and only a portion of the clavicle actually articulates with the manubrium, relying on the SC ligament to provide more stability.
Injury to the SC joint is one of the true medical emergencies in orthopedics. Just posterior to the joint lie the trachea and carotid arteries, and not too lateral from there, the subclavian arteries are located (figure 10.12). A posterior subluxation or dislocation can be a life-threatening emergency with compression on any of these structures.
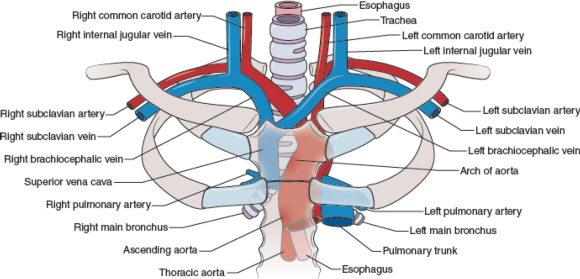
Figure 10.12 Internal structures behind the sternoclavicular (SC) joint.
Because of the SC's importance in connecting the arm to the body proper, the SC joint has many MOIs. One can fall on an outstretched hand or elbow, and the force can transmit along the bones of the arm, acromion of the scapula, and clavicle to the joint, injuring it. Another MOI is a fall on the lateral aspect of the shoulder (humerus or acromion of the scapula), or lying on one side with a pileup on the opposite lateral shoulder. In both of these situations, the force is transmitted along from the humerus/acromion to the clavicle and on to the biomechanically weakest aspect. The athlete could sprain the acromioclavicular joint or fracture the clavicle, or the force could continue medially and injure the SC joint at the sternum.
Incidence and Epidemiology
Injury to the sternoclavicular joint is rare, and posterior dislocations are more unusual. In a study of 251 SC dislocations, only 80 were posterior dislocations. Of the total number of dislocations (both anterior and posterior), the average age of the patient was 29 years old, and 67% of them were male.5 These data are consistent in other publications, in that younger males are more likely to sustain SC injuries than are other age groups or women.6
Risk Factors
Risk factors for injuring the SC joint include falling on an outstretched arm, elbow, or lateral shoulder. As noted, men under 30 years old tend to have higher incidences of SC injuries, so that population is at higher risk. Because high-velocity contact is a MOI, motor vehicle accidents are also a means of sustaining this injury.
Signs and Symptoms
When evaluating an injury to the upper extremity, it is important to be aware of the anatomical connection of the upper extremity and the SC joint. The athlete may initially feel more soreness at the point of impact (e.g., hand, elbow, shoulder) and not recognize the injury to the SC joint. Appreciating the MOI for a potential transmitted force to the medial clavicle and sternum is critical.
On inspection, a deformity may be present over the medial clavicle. It can range from mild swelling to gross deformity. A divot at the SC junction may indicate a posterior dislocation or subluxation, or a posterior fracture of the medial clavicular head (depending on the age of the athlete). Palpation results in a painful SC ligament or joint. Crepitus indicates a fracture, not dislocation or subluxation, but it is equally disconcerting.
Joint stress testing is not recommended, but sometimes the athlete presents with pain away from the SC joint, and that specific injury is not considered at the initial time of testing. The patient will present with an unwillingness to demonstrate full glenohumeral range of motion, because the stress on that joint affects the SC joint.
In a true posterior SC dislocation or subluxation, the patient may have dyspnea or hoarseness and relate difficulty swallowing, because the trachea is pushing posteriorly into the esophagus. If any of these complaints occur, consider it a medical emergency and transport via ambulance as soon as possible. On occasion, the patient will not identify the difficulty swallowing and hoarseness as related to the falling injury, and may not report these conditions. Anecdotal conversations with ATs indicate that athletes sometimes delay reporting issues of the voice or swallowing because they do not relate it to the SC sprain injury, only to have it be an emergency hours later when swelling increases and the airway begins to be compromised.
Field Assessment Techniques
Always assume a potential SC injury when presented with a mechanism consistent with the biomechanical weakness of the joint. Palpate all aspects of the clavicle, SC joint, and manubrium when evaluating falls resulting in landing on the outstretched hand, olecranon of the elbow, or acromion of scapula. If injury to the SC joint is suspected, assess airway and quality of voice. Ask the athlete to swallow, and query whether that action feels normal. Patients with swelling over the SC joint, who report that it is hard to swallow, or who have altered breath sounds, anxiety, or hoarseness should be removed from activity, have their shoulder pads removed (if wearing them), and be transported to the emergency department via ambulance. While waiting for transport, keep the athlete sitting up to facilitate breathing, and apply a sling to the affected arm. The sling will prevent unnecessary movement of the SC joint.
Reduction of the sternoclavicular joint is not recommended on the field. This procedure is performed under sedation or general anesthesia in an operating room. Open reduction and possible stabilization are necessary in situations of failed closed reduction or ongoing symptoms.7 Typically, surgical reduction of this injury is performed in conjunction with a cardiothoracic surgeon because of the potential for complications external to orthopedic surgery.
Diagnostic Accuracy
Standard radiographs of the SC joint are ineffective, because the X-rays are poor at viewing relevant anatomy of the joint.7 One technique that does provide better viewing is the serendipity view, which allows a 40° cephalic tilt.7 In this technique, an anterior dislocation presents as a superiorly displaced medial clavicle, and a posterior dislocation is represented as an inferiorly displaced medial clavicle.7 The preferred imaging is CT, which clearly defines the vascular and respiratory features that could be compromised.
Immediate Management Techniques
If the patient reports no difficulty with breathing or swallowing, but has swelling or tenderness over the SC joint, remove the patient from activity, place the affected arm in a sling, and reassess often. In this situation, ice may be held in place by the patient for 15- to 20-minute intervals if it relieves pain and swelling.
Indications
Dyspnea, hoarseness, or dysphagia following a collision or fall on an out stretched arm, elbow, or lateral shoulder are indications to transport the athlete via ambulance to the nearest ED.
Contraindications
Applying ice to the SC region after an acute injury may be contraindicated for a few reasons. The weight of the ice itself could put additional pressure on an unstable joint, further aggravating any dyspnea. Using a wrap to secure the ice to the area provides additional pressure to the area, which can actually worsen an unstable SC joint injury. The anatomical positioning of the trachea and major vessels from the heart immediately under the thin skin of the neck make ice an inappropriate treatment.
Criteria for Deciding to Transport for Further Medical Examination
Dyspnea, hoarseness, and difficulty swallowing following a collision or fall on an outstretched arm, elbow, or lateral shoulder are indications to transport the patient via ambulance to the nearest emergency department.
Transportation Techniques
Patients with a suspected posterior SC sprain should have supplemental oxygen available delivered via a nasal cannula. Transportation should occur in a recumbent position to facilitate easier respiration. A sling should be placed on the affected arm to relieve any traction of the SC joint from the weight of the upper extremity.
Heat-related emergencies in athletes
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS).
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS). EHS is the only true heat-related life-threatening emergency, and it is the only heat illness discussed here. As the name suggests, EHS is brought about by the combination of exertion (working out), temperature (including air and humidity), and other factors. A person can acclimate to the hot weather if given the time and cautiously increasing the activity duration slowly in the hot environment. Heatstroke is preventable in many aspects, including paying close attention to the weather (air temperature, ambient temperature, humidity, wind, sunshine), the heat and humidity trends in the local area, clothing and equipment worn, work-to-rest ratio, and hydration and food intake.13 Other salient factors include medical conditions, body mass, poor conditioning, medications, prior history of heat illness, and other predispositions that can exacerbate heat illness.14
Incidence and Epidemiology
Although the overall risk of EHS is low, its consequences can be fatal. According to the National Center for Catastrophic Sport Injury Research, 148 deaths have occurred since 1955 (56 since 1996) due to EHS in football.17 Rates are highest across all levels of football (youth, high school, and collegiate) during the preseason and lower during youth practices and high school games.18 Athletics are not alone in EHS injury; the U.S. military forces also have significant data. Fort Benning, Georgia and Fort Bragg, North Carolina led a 14-year study period with over 1,400 heat-related illnesses each, and nearly 3,500 incidents were reported from military bases in North and South Carolina combined (table 15.2).19
Medical Consequences
of Heatstroke
The systemic physiological effects of untreated EHS are many. The rising internal temperature denatures proteins and cellular membranes, causing an inflammatory response.20 As a reaction, the body relocates an aspect of bacteria usually found in the gastrointestinal system, which can promulgate a sepsis reaction systemically, and therefore begins a coagulation reaction throughout organs.20 Aside from death, EHS can elicit multi-organ failure, acute respiratory distress syndrome, and coma. Organ failure can become irreversible and the long-term sequelae catastrophic.
Signs and Symptoms
If the weather is hot or humid, be suspicious of EHS for any athlete who presents with any of these signs of symptoms. The 2 cardinal signs of EHS are a rectal temperature over 105°F (40.5°C) and central nervous system dysfunction, namely, concussion-like behaviors.21 Strictly from an observational standpoint, the athlete may be disoriented, confused, or dizzy, and his performance may be deteriorating. EHS patients tend to have diaphoretic and hot skin. The presence or absence of sweat should not be a deterrent to consider EHS, given other feedback. Complaints of muscular cramping, headache, weakness, or dry mouth are worth continued exploration. Nausea, vomiting, or diarrhea can occur prior to
collapse.14,20-23
Sudden collapse, seizure, altered consciousness, or coma can occur and will likely transpire if not rapidly diagnosed and treated.21,22 Vital signs can diminish with time, especially if the patient is untreated.
Field Assessment Techniques
A person who has heatstroke presents with concussion-like symptoms, which include confusion, stupor, dizziness, personality changes, and acting combative or complacent. A rapid decision must be made to assess core temperature using a rectal thermometer to diagnose EHS (figure 15.1). Every minute delay to diagnose EHS via rectal thermometry is critical.
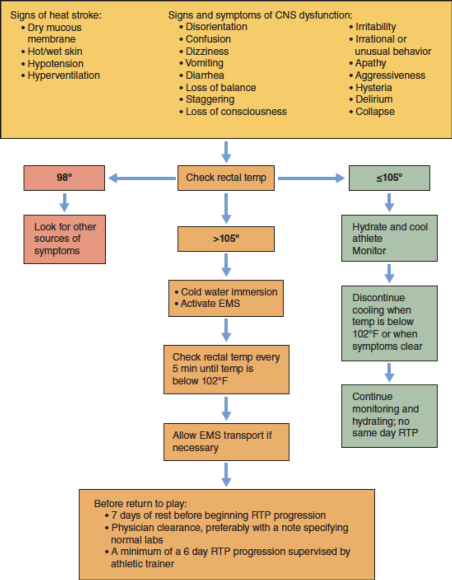
Figure 15.1 Decision tree for EHS.
Safe helmet removal after spinal injury
If the decision has been made to remove the athlete’s equipment, the helmet and shoulder pads should be considered a unit and both be removed.
If the decision has been made to remove the athlete's equipment, the helmet and shoulder pads should be considered a unit and both be removed. Once the face mask has been removed, the helmet can be removed from the injured patient. Less motion in the cervical spine is generated when the face mask is removed from the football helmet prior to removing the helmet.95 Removal of the face mask allows for easier access to stabilize the cervical spine. However, circumstances may arise where the face mask cannot be removed. The sports medicine team should be prepared to remove the helmet under both conditions. Figures 9.24 and 9.25 demonstrate helmet removal with the face mask off and on, respectively. When working with lacrosse, hockey, or other types of helmets, different considerations may need to be made.96-98If time is of the essence, consider leaving the face mask on and simply removing the helmet with the face mask attached.

Figure 9.24 Helmet removal with no face mask.
Courtesy of University of Georgia.

Figure 9.25 Helmet removal with face mask.
Courtesy of University of Georgia.
Here are some tips for helmet removal:
- The chin strap should be cut away, because unsnapping the helmet may create unnecessary movement.
- Cheek pads should be removed from the helmet using a tongue depressor (or something similar) to snap the pad away from the inside of the helmet. However, the ability to remove the cheek pads varies based on the model of the helmet.
- If possible, air bladders in the helmet should be deflated to loosen the fit on the helmet on the patient's head.
- Before the removing the helmet:
- Manual inline stabilization should be transferred from the rescuer at the patient's head (rescuer 1) to rescuer 2, who can provide inline stabilization from the front of the patient.
- Rescuer 2 places 1 hand on the chin and the other hand on the posterior side of the patient's neck (or as depicted in figure 9.26, on either side of the patient's head).
- Rescuer 1, located at the head, grasps the side of the helmet while slightly spreading the cheek pad area on the helmet.
- Rescuer 1 then rotates the helmet forward while sliding the helmet off the patient's head, being mindful to not place the head into flexion or extension.
- Once the helmet is removed, manual inline stabilization should be returned to rescuer 1 and padding (such as a folded towel) should be placed under the patient's head.8 This padding will offset the height of the shoulder pads and prevent hyperextension, which can decrease space available for the cord.
- ATs and other rescue personnel should practice helmet removal with all types of helmets used at their venue.

Figure 9.26 Helmet removal: baseball catcher.
Courtesy of University of Georgia.
Traumatic injuries to the head and face: Subdural hematoma
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.2 Bleeding collects under the inner layer of the dura mater but external to the brain and arachnoid membrane. Subdural hematomas can become life-threatening very quickly.
Incidence and Epidemiology
A subdural hematoma results most often from a severe head injury. Acceleration-deceleration forces cause injuries as the patient's momentum is stopped suddenly by a solid object and the brain makes contact with the inside of the skull.2 Subdural hematomas can present either acutely or chronically based on the time since symptoms first appeared. Acute subdural hematomas occur within 72 hours after injury, while chronic subdural hematomas may take as long 3 weeks to show signs.
Risk Factors
Risk factors associated with acute subdural hematoma include head trauma, postsurgical complications, anticoagulation drug therapy, and nontraumatic cerebral aneurysm. As with epidural hematomas, decreased risk is associated with appropriate use of protective headgear in athletic environments.
Signs and Symptoms
Immediate medical referral and emergency management are recommended for any of the signs presented in the Red Flag box. Subsequent impacts to the head during the development of a chronic subdural hematoma may put patients at a higher risk of experiencing a life-threatening situation; as such, continued monitoring and serial assessment is important.
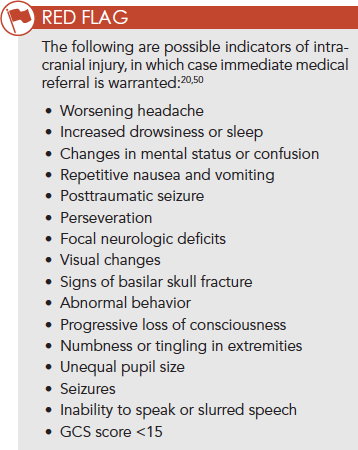
Field Assessment Techniques
In the pre-competition season, athletes participating in at-risk sports (e.g., football, soccer, rugby) should undergo baseline neurocognitive testing, either as a component of a pre-participation physical exam or an adjunct to such an exam. The importance of an established emergency care plan (ECP) cannot be overemphasized; the ECP provides for a standard of care and ensures rapid and efficient treatment measures are in place.
The Canadian CT Head Rule is a clinical prediction rule that uses CT scans to identify head injuries that could require neurosurgical intervention.55 Inclusion criteria include patients with a GCS score of 13 to 15; injury within 24 hours; and blunt head trauma resulting in loss of consciousness, definite amnesia, or disorientation. Exclusion criteria include patients under 16 years of age, nontraumatic cases, patients using anticoagulants or with a bleeding disorder, obvious skull fracture, GCS score of less than 13, and pregnancy.
Immediate Management Techniques
Emergency management of any sports-related injury should first address a primary survey assessment of the patient's mental status, followed by ensuring proper ABC. Knowledge of the patient's neurocognitive baseline may be critical for both short-term and long-term management, and it is helpful when conducting a sideline assessment. Although uncommon, possible differential diagnoses should include intracranial hemorrhage, because the signs and symptoms of a concussion and an intracranial injury are differentiated.50,56 Incorporating potential clinical signs of intracranial injury into the assessment of a patient with a suspected concussion is important.50 Injuries to the head can escalate into medical emergencies quickly, therefore an efficient process of providing immediate care based on signs and symptoms is required (figure 8.6).

Figure 8.6 Head injury algorithm.
Sternoclavicular joint injury
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton.
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton. This joint is a loose connection between the medial clavicle and manubrium of the superior sternum. It has a joint capsule, disc, and several ligaments in addition to the SC ligament—the intraclavicular ligament (between the two medial aspects of the clavicle, superior to the sternum) and the costoclavicular ligament, which maintains the stability of the clavicle on the ribs below. The SC joint is inherently unstable, and only a portion of the clavicle actually articulates with the manubrium, relying on the SC ligament to provide more stability.
Injury to the SC joint is one of the true medical emergencies in orthopedics. Just posterior to the joint lie the trachea and carotid arteries, and not too lateral from there, the subclavian arteries are located (figure 10.12). A posterior subluxation or dislocation can be a life-threatening emergency with compression on any of these structures.
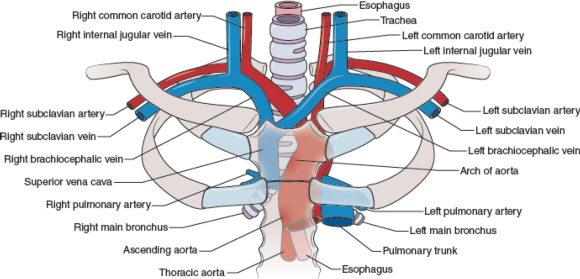
Figure 10.12 Internal structures behind the sternoclavicular (SC) joint.
Because of the SC's importance in connecting the arm to the body proper, the SC joint has many MOIs. One can fall on an outstretched hand or elbow, and the force can transmit along the bones of the arm, acromion of the scapula, and clavicle to the joint, injuring it. Another MOI is a fall on the lateral aspect of the shoulder (humerus or acromion of the scapula), or lying on one side with a pileup on the opposite lateral shoulder. In both of these situations, the force is transmitted along from the humerus/acromion to the clavicle and on to the biomechanically weakest aspect. The athlete could sprain the acromioclavicular joint or fracture the clavicle, or the force could continue medially and injure the SC joint at the sternum.
Incidence and Epidemiology
Injury to the sternoclavicular joint is rare, and posterior dislocations are more unusual. In a study of 251 SC dislocations, only 80 were posterior dislocations. Of the total number of dislocations (both anterior and posterior), the average age of the patient was 29 years old, and 67% of them were male.5 These data are consistent in other publications, in that younger males are more likely to sustain SC injuries than are other age groups or women.6
Risk Factors
Risk factors for injuring the SC joint include falling on an outstretched arm, elbow, or lateral shoulder. As noted, men under 30 years old tend to have higher incidences of SC injuries, so that population is at higher risk. Because high-velocity contact is a MOI, motor vehicle accidents are also a means of sustaining this injury.
Signs and Symptoms
When evaluating an injury to the upper extremity, it is important to be aware of the anatomical connection of the upper extremity and the SC joint. The athlete may initially feel more soreness at the point of impact (e.g., hand, elbow, shoulder) and not recognize the injury to the SC joint. Appreciating the MOI for a potential transmitted force to the medial clavicle and sternum is critical.
On inspection, a deformity may be present over the medial clavicle. It can range from mild swelling to gross deformity. A divot at the SC junction may indicate a posterior dislocation or subluxation, or a posterior fracture of the medial clavicular head (depending on the age of the athlete). Palpation results in a painful SC ligament or joint. Crepitus indicates a fracture, not dislocation or subluxation, but it is equally disconcerting.
Joint stress testing is not recommended, but sometimes the athlete presents with pain away from the SC joint, and that specific injury is not considered at the initial time of testing. The patient will present with an unwillingness to demonstrate full glenohumeral range of motion, because the stress on that joint affects the SC joint.
In a true posterior SC dislocation or subluxation, the patient may have dyspnea or hoarseness and relate difficulty swallowing, because the trachea is pushing posteriorly into the esophagus. If any of these complaints occur, consider it a medical emergency and transport via ambulance as soon as possible. On occasion, the patient will not identify the difficulty swallowing and hoarseness as related to the falling injury, and may not report these conditions. Anecdotal conversations with ATs indicate that athletes sometimes delay reporting issues of the voice or swallowing because they do not relate it to the SC sprain injury, only to have it be an emergency hours later when swelling increases and the airway begins to be compromised.
Field Assessment Techniques
Always assume a potential SC injury when presented with a mechanism consistent with the biomechanical weakness of the joint. Palpate all aspects of the clavicle, SC joint, and manubrium when evaluating falls resulting in landing on the outstretched hand, olecranon of the elbow, or acromion of scapula. If injury to the SC joint is suspected, assess airway and quality of voice. Ask the athlete to swallow, and query whether that action feels normal. Patients with swelling over the SC joint, who report that it is hard to swallow, or who have altered breath sounds, anxiety, or hoarseness should be removed from activity, have their shoulder pads removed (if wearing them), and be transported to the emergency department via ambulance. While waiting for transport, keep the athlete sitting up to facilitate breathing, and apply a sling to the affected arm. The sling will prevent unnecessary movement of the SC joint.
Reduction of the sternoclavicular joint is not recommended on the field. This procedure is performed under sedation or general anesthesia in an operating room. Open reduction and possible stabilization are necessary in situations of failed closed reduction or ongoing symptoms.7 Typically, surgical reduction of this injury is performed in conjunction with a cardiothoracic surgeon because of the potential for complications external to orthopedic surgery.
Diagnostic Accuracy
Standard radiographs of the SC joint are ineffective, because the X-rays are poor at viewing relevant anatomy of the joint.7 One technique that does provide better viewing is the serendipity view, which allows a 40° cephalic tilt.7 In this technique, an anterior dislocation presents as a superiorly displaced medial clavicle, and a posterior dislocation is represented as an inferiorly displaced medial clavicle.7 The preferred imaging is CT, which clearly defines the vascular and respiratory features that could be compromised.
Immediate Management Techniques
If the patient reports no difficulty with breathing or swallowing, but has swelling or tenderness over the SC joint, remove the patient from activity, place the affected arm in a sling, and reassess often. In this situation, ice may be held in place by the patient for 15- to 20-minute intervals if it relieves pain and swelling.
Indications
Dyspnea, hoarseness, or dysphagia following a collision or fall on an out stretched arm, elbow, or lateral shoulder are indications to transport the athlete via ambulance to the nearest ED.
Contraindications
Applying ice to the SC region after an acute injury may be contraindicated for a few reasons. The weight of the ice itself could put additional pressure on an unstable joint, further aggravating any dyspnea. Using a wrap to secure the ice to the area provides additional pressure to the area, which can actually worsen an unstable SC joint injury. The anatomical positioning of the trachea and major vessels from the heart immediately under the thin skin of the neck make ice an inappropriate treatment.
Criteria for Deciding to Transport for Further Medical Examination
Dyspnea, hoarseness, and difficulty swallowing following a collision or fall on an outstretched arm, elbow, or lateral shoulder are indications to transport the patient via ambulance to the nearest emergency department.
Transportation Techniques
Patients with a suspected posterior SC sprain should have supplemental oxygen available delivered via a nasal cannula. Transportation should occur in a recumbent position to facilitate easier respiration. A sling should be placed on the affected arm to relieve any traction of the SC joint from the weight of the upper extremity.
Heat-related emergencies in athletes
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS).
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS). EHS is the only true heat-related life-threatening emergency, and it is the only heat illness discussed here. As the name suggests, EHS is brought about by the combination of exertion (working out), temperature (including air and humidity), and other factors. A person can acclimate to the hot weather if given the time and cautiously increasing the activity duration slowly in the hot environment. Heatstroke is preventable in many aspects, including paying close attention to the weather (air temperature, ambient temperature, humidity, wind, sunshine), the heat and humidity trends in the local area, clothing and equipment worn, work-to-rest ratio, and hydration and food intake.13 Other salient factors include medical conditions, body mass, poor conditioning, medications, prior history of heat illness, and other predispositions that can exacerbate heat illness.14
Incidence and Epidemiology
Although the overall risk of EHS is low, its consequences can be fatal. According to the National Center for Catastrophic Sport Injury Research, 148 deaths have occurred since 1955 (56 since 1996) due to EHS in football.17 Rates are highest across all levels of football (youth, high school, and collegiate) during the preseason and lower during youth practices and high school games.18 Athletics are not alone in EHS injury; the U.S. military forces also have significant data. Fort Benning, Georgia and Fort Bragg, North Carolina led a 14-year study period with over 1,400 heat-related illnesses each, and nearly 3,500 incidents were reported from military bases in North and South Carolina combined (table 15.2).19
Medical Consequences
of Heatstroke
The systemic physiological effects of untreated EHS are many. The rising internal temperature denatures proteins and cellular membranes, causing an inflammatory response.20 As a reaction, the body relocates an aspect of bacteria usually found in the gastrointestinal system, which can promulgate a sepsis reaction systemically, and therefore begins a coagulation reaction throughout organs.20 Aside from death, EHS can elicit multi-organ failure, acute respiratory distress syndrome, and coma. Organ failure can become irreversible and the long-term sequelae catastrophic.
Signs and Symptoms
If the weather is hot or humid, be suspicious of EHS for any athlete who presents with any of these signs of symptoms. The 2 cardinal signs of EHS are a rectal temperature over 105°F (40.5°C) and central nervous system dysfunction, namely, concussion-like behaviors.21 Strictly from an observational standpoint, the athlete may be disoriented, confused, or dizzy, and his performance may be deteriorating. EHS patients tend to have diaphoretic and hot skin. The presence or absence of sweat should not be a deterrent to consider EHS, given other feedback. Complaints of muscular cramping, headache, weakness, or dry mouth are worth continued exploration. Nausea, vomiting, or diarrhea can occur prior to
collapse.14,20-23
Sudden collapse, seizure, altered consciousness, or coma can occur and will likely transpire if not rapidly diagnosed and treated.21,22 Vital signs can diminish with time, especially if the patient is untreated.
Field Assessment Techniques
A person who has heatstroke presents with concussion-like symptoms, which include confusion, stupor, dizziness, personality changes, and acting combative or complacent. A rapid decision must be made to assess core temperature using a rectal thermometer to diagnose EHS (figure 15.1). Every minute delay to diagnose EHS via rectal thermometry is critical.
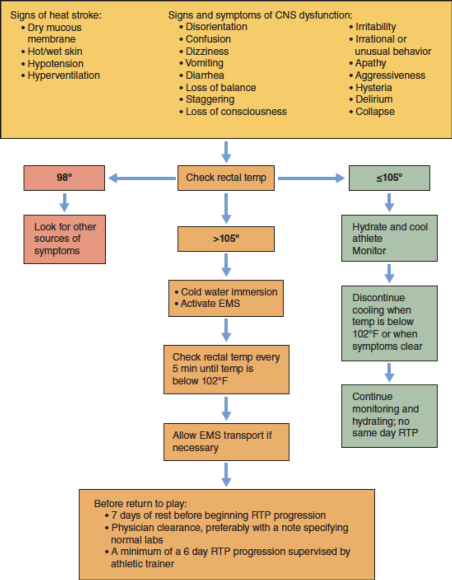
Figure 15.1 Decision tree for EHS.
Safe helmet removal after spinal injury
If the decision has been made to remove the athlete’s equipment, the helmet and shoulder pads should be considered a unit and both be removed.
If the decision has been made to remove the athlete's equipment, the helmet and shoulder pads should be considered a unit and both be removed. Once the face mask has been removed, the helmet can be removed from the injured patient. Less motion in the cervical spine is generated when the face mask is removed from the football helmet prior to removing the helmet.95 Removal of the face mask allows for easier access to stabilize the cervical spine. However, circumstances may arise where the face mask cannot be removed. The sports medicine team should be prepared to remove the helmet under both conditions. Figures 9.24 and 9.25 demonstrate helmet removal with the face mask off and on, respectively. When working with lacrosse, hockey, or other types of helmets, different considerations may need to be made.96-98If time is of the essence, consider leaving the face mask on and simply removing the helmet with the face mask attached.

Figure 9.24 Helmet removal with no face mask.
Courtesy of University of Georgia.

Figure 9.25 Helmet removal with face mask.
Courtesy of University of Georgia.
Here are some tips for helmet removal:
- The chin strap should be cut away, because unsnapping the helmet may create unnecessary movement.
- Cheek pads should be removed from the helmet using a tongue depressor (or something similar) to snap the pad away from the inside of the helmet. However, the ability to remove the cheek pads varies based on the model of the helmet.
- If possible, air bladders in the helmet should be deflated to loosen the fit on the helmet on the patient's head.
- Before the removing the helmet:
- Manual inline stabilization should be transferred from the rescuer at the patient's head (rescuer 1) to rescuer 2, who can provide inline stabilization from the front of the patient.
- Rescuer 2 places 1 hand on the chin and the other hand on the posterior side of the patient's neck (or as depicted in figure 9.26, on either side of the patient's head).
- Rescuer 1, located at the head, grasps the side of the helmet while slightly spreading the cheek pad area on the helmet.
- Rescuer 1 then rotates the helmet forward while sliding the helmet off the patient's head, being mindful to not place the head into flexion or extension.
- Once the helmet is removed, manual inline stabilization should be returned to rescuer 1 and padding (such as a folded towel) should be placed under the patient's head.8 This padding will offset the height of the shoulder pads and prevent hyperextension, which can decrease space available for the cord.
- ATs and other rescue personnel should practice helmet removal with all types of helmets used at their venue.

Figure 9.26 Helmet removal: baseball catcher.
Courtesy of University of Georgia.
Traumatic injuries to the head and face: Subdural hematoma
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.2 Bleeding collects under the inner layer of the dura mater but external to the brain and arachnoid membrane. Subdural hematomas can become life-threatening very quickly.
Incidence and Epidemiology
A subdural hematoma results most often from a severe head injury. Acceleration-deceleration forces cause injuries as the patient's momentum is stopped suddenly by a solid object and the brain makes contact with the inside of the skull.2 Subdural hematomas can present either acutely or chronically based on the time since symptoms first appeared. Acute subdural hematomas occur within 72 hours after injury, while chronic subdural hematomas may take as long 3 weeks to show signs.
Risk Factors
Risk factors associated with acute subdural hematoma include head trauma, postsurgical complications, anticoagulation drug therapy, and nontraumatic cerebral aneurysm. As with epidural hematomas, decreased risk is associated with appropriate use of protective headgear in athletic environments.
Signs and Symptoms
Immediate medical referral and emergency management are recommended for any of the signs presented in the Red Flag box. Subsequent impacts to the head during the development of a chronic subdural hematoma may put patients at a higher risk of experiencing a life-threatening situation; as such, continued monitoring and serial assessment is important.
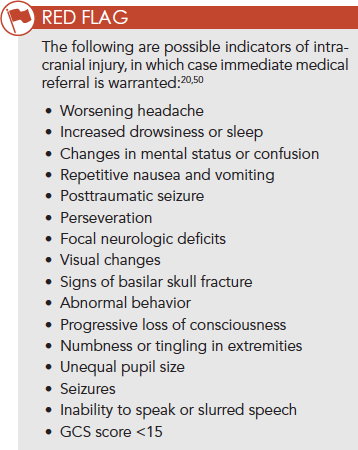
Field Assessment Techniques
In the pre-competition season, athletes participating in at-risk sports (e.g., football, soccer, rugby) should undergo baseline neurocognitive testing, either as a component of a pre-participation physical exam or an adjunct to such an exam. The importance of an established emergency care plan (ECP) cannot be overemphasized; the ECP provides for a standard of care and ensures rapid and efficient treatment measures are in place.
The Canadian CT Head Rule is a clinical prediction rule that uses CT scans to identify head injuries that could require neurosurgical intervention.55 Inclusion criteria include patients with a GCS score of 13 to 15; injury within 24 hours; and blunt head trauma resulting in loss of consciousness, definite amnesia, or disorientation. Exclusion criteria include patients under 16 years of age, nontraumatic cases, patients using anticoagulants or with a bleeding disorder, obvious skull fracture, GCS score of less than 13, and pregnancy.
Immediate Management Techniques
Emergency management of any sports-related injury should first address a primary survey assessment of the patient's mental status, followed by ensuring proper ABC. Knowledge of the patient's neurocognitive baseline may be critical for both short-term and long-term management, and it is helpful when conducting a sideline assessment. Although uncommon, possible differential diagnoses should include intracranial hemorrhage, because the signs and symptoms of a concussion and an intracranial injury are differentiated.50,56 Incorporating potential clinical signs of intracranial injury into the assessment of a patient with a suspected concussion is important.50 Injuries to the head can escalate into medical emergencies quickly, therefore an efficient process of providing immediate care based on signs and symptoms is required (figure 8.6).

Figure 8.6 Head injury algorithm.
Sternoclavicular joint injury
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton.
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton. This joint is a loose connection between the medial clavicle and manubrium of the superior sternum. It has a joint capsule, disc, and several ligaments in addition to the SC ligament—the intraclavicular ligament (between the two medial aspects of the clavicle, superior to the sternum) and the costoclavicular ligament, which maintains the stability of the clavicle on the ribs below. The SC joint is inherently unstable, and only a portion of the clavicle actually articulates with the manubrium, relying on the SC ligament to provide more stability.
Injury to the SC joint is one of the true medical emergencies in orthopedics. Just posterior to the joint lie the trachea and carotid arteries, and not too lateral from there, the subclavian arteries are located (figure 10.12). A posterior subluxation or dislocation can be a life-threatening emergency with compression on any of these structures.
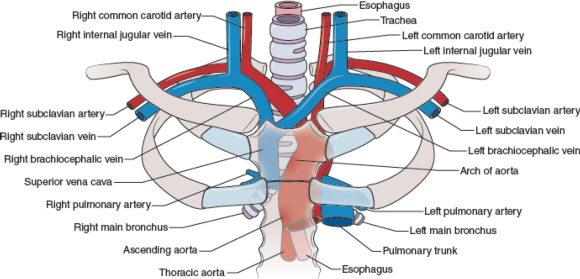
Figure 10.12 Internal structures behind the sternoclavicular (SC) joint.
Because of the SC's importance in connecting the arm to the body proper, the SC joint has many MOIs. One can fall on an outstretched hand or elbow, and the force can transmit along the bones of the arm, acromion of the scapula, and clavicle to the joint, injuring it. Another MOI is a fall on the lateral aspect of the shoulder (humerus or acromion of the scapula), or lying on one side with a pileup on the opposite lateral shoulder. In both of these situations, the force is transmitted along from the humerus/acromion to the clavicle and on to the biomechanically weakest aspect. The athlete could sprain the acromioclavicular joint or fracture the clavicle, or the force could continue medially and injure the SC joint at the sternum.
Incidence and Epidemiology
Injury to the sternoclavicular joint is rare, and posterior dislocations are more unusual. In a study of 251 SC dislocations, only 80 were posterior dislocations. Of the total number of dislocations (both anterior and posterior), the average age of the patient was 29 years old, and 67% of them were male.5 These data are consistent in other publications, in that younger males are more likely to sustain SC injuries than are other age groups or women.6
Risk Factors
Risk factors for injuring the SC joint include falling on an outstretched arm, elbow, or lateral shoulder. As noted, men under 30 years old tend to have higher incidences of SC injuries, so that population is at higher risk. Because high-velocity contact is a MOI, motor vehicle accidents are also a means of sustaining this injury.
Signs and Symptoms
When evaluating an injury to the upper extremity, it is important to be aware of the anatomical connection of the upper extremity and the SC joint. The athlete may initially feel more soreness at the point of impact (e.g., hand, elbow, shoulder) and not recognize the injury to the SC joint. Appreciating the MOI for a potential transmitted force to the medial clavicle and sternum is critical.
On inspection, a deformity may be present over the medial clavicle. It can range from mild swelling to gross deformity. A divot at the SC junction may indicate a posterior dislocation or subluxation, or a posterior fracture of the medial clavicular head (depending on the age of the athlete). Palpation results in a painful SC ligament or joint. Crepitus indicates a fracture, not dislocation or subluxation, but it is equally disconcerting.
Joint stress testing is not recommended, but sometimes the athlete presents with pain away from the SC joint, and that specific injury is not considered at the initial time of testing. The patient will present with an unwillingness to demonstrate full glenohumeral range of motion, because the stress on that joint affects the SC joint.
In a true posterior SC dislocation or subluxation, the patient may have dyspnea or hoarseness and relate difficulty swallowing, because the trachea is pushing posteriorly into the esophagus. If any of these complaints occur, consider it a medical emergency and transport via ambulance as soon as possible. On occasion, the patient will not identify the difficulty swallowing and hoarseness as related to the falling injury, and may not report these conditions. Anecdotal conversations with ATs indicate that athletes sometimes delay reporting issues of the voice or swallowing because they do not relate it to the SC sprain injury, only to have it be an emergency hours later when swelling increases and the airway begins to be compromised.
Field Assessment Techniques
Always assume a potential SC injury when presented with a mechanism consistent with the biomechanical weakness of the joint. Palpate all aspects of the clavicle, SC joint, and manubrium when evaluating falls resulting in landing on the outstretched hand, olecranon of the elbow, or acromion of scapula. If injury to the SC joint is suspected, assess airway and quality of voice. Ask the athlete to swallow, and query whether that action feels normal. Patients with swelling over the SC joint, who report that it is hard to swallow, or who have altered breath sounds, anxiety, or hoarseness should be removed from activity, have their shoulder pads removed (if wearing them), and be transported to the emergency department via ambulance. While waiting for transport, keep the athlete sitting up to facilitate breathing, and apply a sling to the affected arm. The sling will prevent unnecessary movement of the SC joint.
Reduction of the sternoclavicular joint is not recommended on the field. This procedure is performed under sedation or general anesthesia in an operating room. Open reduction and possible stabilization are necessary in situations of failed closed reduction or ongoing symptoms.7 Typically, surgical reduction of this injury is performed in conjunction with a cardiothoracic surgeon because of the potential for complications external to orthopedic surgery.
Diagnostic Accuracy
Standard radiographs of the SC joint are ineffective, because the X-rays are poor at viewing relevant anatomy of the joint.7 One technique that does provide better viewing is the serendipity view, which allows a 40° cephalic tilt.7 In this technique, an anterior dislocation presents as a superiorly displaced medial clavicle, and a posterior dislocation is represented as an inferiorly displaced medial clavicle.7 The preferred imaging is CT, which clearly defines the vascular and respiratory features that could be compromised.
Immediate Management Techniques
If the patient reports no difficulty with breathing or swallowing, but has swelling or tenderness over the SC joint, remove the patient from activity, place the affected arm in a sling, and reassess often. In this situation, ice may be held in place by the patient for 15- to 20-minute intervals if it relieves pain and swelling.
Indications
Dyspnea, hoarseness, or dysphagia following a collision or fall on an out stretched arm, elbow, or lateral shoulder are indications to transport the athlete via ambulance to the nearest ED.
Contraindications
Applying ice to the SC region after an acute injury may be contraindicated for a few reasons. The weight of the ice itself could put additional pressure on an unstable joint, further aggravating any dyspnea. Using a wrap to secure the ice to the area provides additional pressure to the area, which can actually worsen an unstable SC joint injury. The anatomical positioning of the trachea and major vessels from the heart immediately under the thin skin of the neck make ice an inappropriate treatment.
Criteria for Deciding to Transport for Further Medical Examination
Dyspnea, hoarseness, and difficulty swallowing following a collision or fall on an outstretched arm, elbow, or lateral shoulder are indications to transport the patient via ambulance to the nearest emergency department.
Transportation Techniques
Patients with a suspected posterior SC sprain should have supplemental oxygen available delivered via a nasal cannula. Transportation should occur in a recumbent position to facilitate easier respiration. A sling should be placed on the affected arm to relieve any traction of the SC joint from the weight of the upper extremity.
Heat-related emergencies in athletes
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS).
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS). EHS is the only true heat-related life-threatening emergency, and it is the only heat illness discussed here. As the name suggests, EHS is brought about by the combination of exertion (working out), temperature (including air and humidity), and other factors. A person can acclimate to the hot weather if given the time and cautiously increasing the activity duration slowly in the hot environment. Heatstroke is preventable in many aspects, including paying close attention to the weather (air temperature, ambient temperature, humidity, wind, sunshine), the heat and humidity trends in the local area, clothing and equipment worn, work-to-rest ratio, and hydration and food intake.13 Other salient factors include medical conditions, body mass, poor conditioning, medications, prior history of heat illness, and other predispositions that can exacerbate heat illness.14
Incidence and Epidemiology
Although the overall risk of EHS is low, its consequences can be fatal. According to the National Center for Catastrophic Sport Injury Research, 148 deaths have occurred since 1955 (56 since 1996) due to EHS in football.17 Rates are highest across all levels of football (youth, high school, and collegiate) during the preseason and lower during youth practices and high school games.18 Athletics are not alone in EHS injury; the U.S. military forces also have significant data. Fort Benning, Georgia and Fort Bragg, North Carolina led a 14-year study period with over 1,400 heat-related illnesses each, and nearly 3,500 incidents were reported from military bases in North and South Carolina combined (table 15.2).19
Medical Consequences
of Heatstroke
The systemic physiological effects of untreated EHS are many. The rising internal temperature denatures proteins and cellular membranes, causing an inflammatory response.20 As a reaction, the body relocates an aspect of bacteria usually found in the gastrointestinal system, which can promulgate a sepsis reaction systemically, and therefore begins a coagulation reaction throughout organs.20 Aside from death, EHS can elicit multi-organ failure, acute respiratory distress syndrome, and coma. Organ failure can become irreversible and the long-term sequelae catastrophic.
Signs and Symptoms
If the weather is hot or humid, be suspicious of EHS for any athlete who presents with any of these signs of symptoms. The 2 cardinal signs of EHS are a rectal temperature over 105°F (40.5°C) and central nervous system dysfunction, namely, concussion-like behaviors.21 Strictly from an observational standpoint, the athlete may be disoriented, confused, or dizzy, and his performance may be deteriorating. EHS patients tend to have diaphoretic and hot skin. The presence or absence of sweat should not be a deterrent to consider EHS, given other feedback. Complaints of muscular cramping, headache, weakness, or dry mouth are worth continued exploration. Nausea, vomiting, or diarrhea can occur prior to
collapse.14,20-23
Sudden collapse, seizure, altered consciousness, or coma can occur and will likely transpire if not rapidly diagnosed and treated.21,22 Vital signs can diminish with time, especially if the patient is untreated.
Field Assessment Techniques
A person who has heatstroke presents with concussion-like symptoms, which include confusion, stupor, dizziness, personality changes, and acting combative or complacent. A rapid decision must be made to assess core temperature using a rectal thermometer to diagnose EHS (figure 15.1). Every minute delay to diagnose EHS via rectal thermometry is critical.
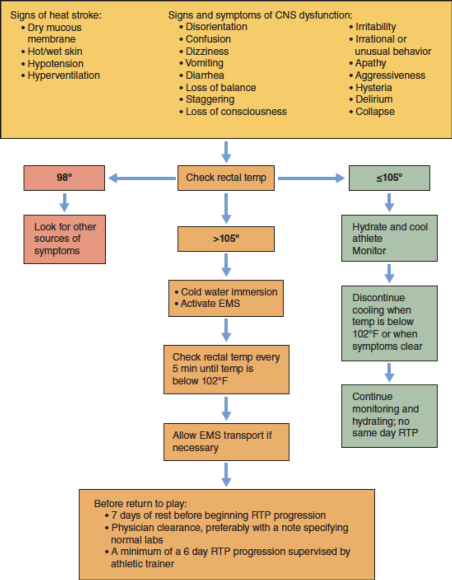
Figure 15.1 Decision tree for EHS.
Safe helmet removal after spinal injury
If the decision has been made to remove the athlete’s equipment, the helmet and shoulder pads should be considered a unit and both be removed.
If the decision has been made to remove the athlete's equipment, the helmet and shoulder pads should be considered a unit and both be removed. Once the face mask has been removed, the helmet can be removed from the injured patient. Less motion in the cervical spine is generated when the face mask is removed from the football helmet prior to removing the helmet.95 Removal of the face mask allows for easier access to stabilize the cervical spine. However, circumstances may arise where the face mask cannot be removed. The sports medicine team should be prepared to remove the helmet under both conditions. Figures 9.24 and 9.25 demonstrate helmet removal with the face mask off and on, respectively. When working with lacrosse, hockey, or other types of helmets, different considerations may need to be made.96-98If time is of the essence, consider leaving the face mask on and simply removing the helmet with the face mask attached.

Figure 9.24 Helmet removal with no face mask.
Courtesy of University of Georgia.

Figure 9.25 Helmet removal with face mask.
Courtesy of University of Georgia.
Here are some tips for helmet removal:
- The chin strap should be cut away, because unsnapping the helmet may create unnecessary movement.
- Cheek pads should be removed from the helmet using a tongue depressor (or something similar) to snap the pad away from the inside of the helmet. However, the ability to remove the cheek pads varies based on the model of the helmet.
- If possible, air bladders in the helmet should be deflated to loosen the fit on the helmet on the patient's head.
- Before the removing the helmet:
- Manual inline stabilization should be transferred from the rescuer at the patient's head (rescuer 1) to rescuer 2, who can provide inline stabilization from the front of the patient.
- Rescuer 2 places 1 hand on the chin and the other hand on the posterior side of the patient's neck (or as depicted in figure 9.26, on either side of the patient's head).
- Rescuer 1, located at the head, grasps the side of the helmet while slightly spreading the cheek pad area on the helmet.
- Rescuer 1 then rotates the helmet forward while sliding the helmet off the patient's head, being mindful to not place the head into flexion or extension.
- Once the helmet is removed, manual inline stabilization should be returned to rescuer 1 and padding (such as a folded towel) should be placed under the patient's head.8 This padding will offset the height of the shoulder pads and prevent hyperextension, which can decrease space available for the cord.
- ATs and other rescue personnel should practice helmet removal with all types of helmets used at their venue.

Figure 9.26 Helmet removal: baseball catcher.
Courtesy of University of Georgia.
Traumatic injuries to the head and face: Subdural hematoma
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.2 Bleeding collects under the inner layer of the dura mater but external to the brain and arachnoid membrane. Subdural hematomas can become life-threatening very quickly.
Incidence and Epidemiology
A subdural hematoma results most often from a severe head injury. Acceleration-deceleration forces cause injuries as the patient's momentum is stopped suddenly by a solid object and the brain makes contact with the inside of the skull.2 Subdural hematomas can present either acutely or chronically based on the time since symptoms first appeared. Acute subdural hematomas occur within 72 hours after injury, while chronic subdural hematomas may take as long 3 weeks to show signs.
Risk Factors
Risk factors associated with acute subdural hematoma include head trauma, postsurgical complications, anticoagulation drug therapy, and nontraumatic cerebral aneurysm. As with epidural hematomas, decreased risk is associated with appropriate use of protective headgear in athletic environments.
Signs and Symptoms
Immediate medical referral and emergency management are recommended for any of the signs presented in the Red Flag box. Subsequent impacts to the head during the development of a chronic subdural hematoma may put patients at a higher risk of experiencing a life-threatening situation; as such, continued monitoring and serial assessment is important.
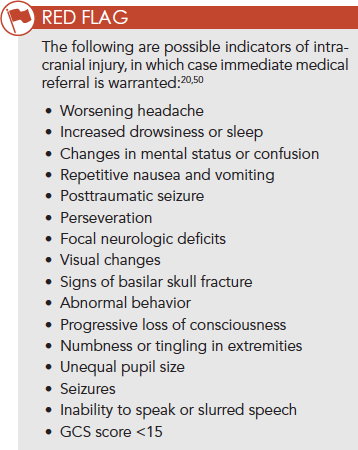
Field Assessment Techniques
In the pre-competition season, athletes participating in at-risk sports (e.g., football, soccer, rugby) should undergo baseline neurocognitive testing, either as a component of a pre-participation physical exam or an adjunct to such an exam. The importance of an established emergency care plan (ECP) cannot be overemphasized; the ECP provides for a standard of care and ensures rapid and efficient treatment measures are in place.
The Canadian CT Head Rule is a clinical prediction rule that uses CT scans to identify head injuries that could require neurosurgical intervention.55 Inclusion criteria include patients with a GCS score of 13 to 15; injury within 24 hours; and blunt head trauma resulting in loss of consciousness, definite amnesia, or disorientation. Exclusion criteria include patients under 16 years of age, nontraumatic cases, patients using anticoagulants or with a bleeding disorder, obvious skull fracture, GCS score of less than 13, and pregnancy.
Immediate Management Techniques
Emergency management of any sports-related injury should first address a primary survey assessment of the patient's mental status, followed by ensuring proper ABC. Knowledge of the patient's neurocognitive baseline may be critical for both short-term and long-term management, and it is helpful when conducting a sideline assessment. Although uncommon, possible differential diagnoses should include intracranial hemorrhage, because the signs and symptoms of a concussion and an intracranial injury are differentiated.50,56 Incorporating potential clinical signs of intracranial injury into the assessment of a patient with a suspected concussion is important.50 Injuries to the head can escalate into medical emergencies quickly, therefore an efficient process of providing immediate care based on signs and symptoms is required (figure 8.6).

Figure 8.6 Head injury algorithm.
Sternoclavicular joint injury
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton.
The sternoclavicular (SC) joint is the only place on the body where the upper arm attaches via bony articulation to the axial skeleton. This joint is a loose connection between the medial clavicle and manubrium of the superior sternum. It has a joint capsule, disc, and several ligaments in addition to the SC ligament—the intraclavicular ligament (between the two medial aspects of the clavicle, superior to the sternum) and the costoclavicular ligament, which maintains the stability of the clavicle on the ribs below. The SC joint is inherently unstable, and only a portion of the clavicle actually articulates with the manubrium, relying on the SC ligament to provide more stability.
Injury to the SC joint is one of the true medical emergencies in orthopedics. Just posterior to the joint lie the trachea and carotid arteries, and not too lateral from there, the subclavian arteries are located (figure 10.12). A posterior subluxation or dislocation can be a life-threatening emergency with compression on any of these structures.
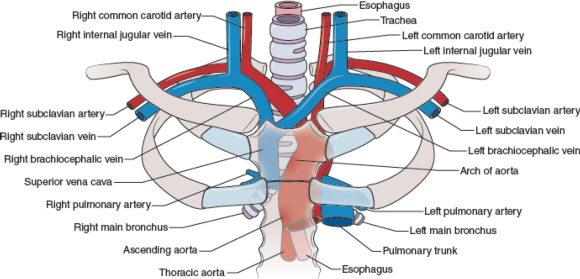
Figure 10.12 Internal structures behind the sternoclavicular (SC) joint.
Because of the SC's importance in connecting the arm to the body proper, the SC joint has many MOIs. One can fall on an outstretched hand or elbow, and the force can transmit along the bones of the arm, acromion of the scapula, and clavicle to the joint, injuring it. Another MOI is a fall on the lateral aspect of the shoulder (humerus or acromion of the scapula), or lying on one side with a pileup on the opposite lateral shoulder. In both of these situations, the force is transmitted along from the humerus/acromion to the clavicle and on to the biomechanically weakest aspect. The athlete could sprain the acromioclavicular joint or fracture the clavicle, or the force could continue medially and injure the SC joint at the sternum.
Incidence and Epidemiology
Injury to the sternoclavicular joint is rare, and posterior dislocations are more unusual. In a study of 251 SC dislocations, only 80 were posterior dislocations. Of the total number of dislocations (both anterior and posterior), the average age of the patient was 29 years old, and 67% of them were male.5 These data are consistent in other publications, in that younger males are more likely to sustain SC injuries than are other age groups or women.6
Risk Factors
Risk factors for injuring the SC joint include falling on an outstretched arm, elbow, or lateral shoulder. As noted, men under 30 years old tend to have higher incidences of SC injuries, so that population is at higher risk. Because high-velocity contact is a MOI, motor vehicle accidents are also a means of sustaining this injury.
Signs and Symptoms
When evaluating an injury to the upper extremity, it is important to be aware of the anatomical connection of the upper extremity and the SC joint. The athlete may initially feel more soreness at the point of impact (e.g., hand, elbow, shoulder) and not recognize the injury to the SC joint. Appreciating the MOI for a potential transmitted force to the medial clavicle and sternum is critical.
On inspection, a deformity may be present over the medial clavicle. It can range from mild swelling to gross deformity. A divot at the SC junction may indicate a posterior dislocation or subluxation, or a posterior fracture of the medial clavicular head (depending on the age of the athlete). Palpation results in a painful SC ligament or joint. Crepitus indicates a fracture, not dislocation or subluxation, but it is equally disconcerting.
Joint stress testing is not recommended, but sometimes the athlete presents with pain away from the SC joint, and that specific injury is not considered at the initial time of testing. The patient will present with an unwillingness to demonstrate full glenohumeral range of motion, because the stress on that joint affects the SC joint.
In a true posterior SC dislocation or subluxation, the patient may have dyspnea or hoarseness and relate difficulty swallowing, because the trachea is pushing posteriorly into the esophagus. If any of these complaints occur, consider it a medical emergency and transport via ambulance as soon as possible. On occasion, the patient will not identify the difficulty swallowing and hoarseness as related to the falling injury, and may not report these conditions. Anecdotal conversations with ATs indicate that athletes sometimes delay reporting issues of the voice or swallowing because they do not relate it to the SC sprain injury, only to have it be an emergency hours later when swelling increases and the airway begins to be compromised.
Field Assessment Techniques
Always assume a potential SC injury when presented with a mechanism consistent with the biomechanical weakness of the joint. Palpate all aspects of the clavicle, SC joint, and manubrium when evaluating falls resulting in landing on the outstretched hand, olecranon of the elbow, or acromion of scapula. If injury to the SC joint is suspected, assess airway and quality of voice. Ask the athlete to swallow, and query whether that action feels normal. Patients with swelling over the SC joint, who report that it is hard to swallow, or who have altered breath sounds, anxiety, or hoarseness should be removed from activity, have their shoulder pads removed (if wearing them), and be transported to the emergency department via ambulance. While waiting for transport, keep the athlete sitting up to facilitate breathing, and apply a sling to the affected arm. The sling will prevent unnecessary movement of the SC joint.
Reduction of the sternoclavicular joint is not recommended on the field. This procedure is performed under sedation or general anesthesia in an operating room. Open reduction and possible stabilization are necessary in situations of failed closed reduction or ongoing symptoms.7 Typically, surgical reduction of this injury is performed in conjunction with a cardiothoracic surgeon because of the potential for complications external to orthopedic surgery.
Diagnostic Accuracy
Standard radiographs of the SC joint are ineffective, because the X-rays are poor at viewing relevant anatomy of the joint.7 One technique that does provide better viewing is the serendipity view, which allows a 40° cephalic tilt.7 In this technique, an anterior dislocation presents as a superiorly displaced medial clavicle, and a posterior dislocation is represented as an inferiorly displaced medial clavicle.7 The preferred imaging is CT, which clearly defines the vascular and respiratory features that could be compromised.
Immediate Management Techniques
If the patient reports no difficulty with breathing or swallowing, but has swelling or tenderness over the SC joint, remove the patient from activity, place the affected arm in a sling, and reassess often. In this situation, ice may be held in place by the patient for 15- to 20-minute intervals if it relieves pain and swelling.
Indications
Dyspnea, hoarseness, or dysphagia following a collision or fall on an out stretched arm, elbow, or lateral shoulder are indications to transport the athlete via ambulance to the nearest ED.
Contraindications
Applying ice to the SC region after an acute injury may be contraindicated for a few reasons. The weight of the ice itself could put additional pressure on an unstable joint, further aggravating any dyspnea. Using a wrap to secure the ice to the area provides additional pressure to the area, which can actually worsen an unstable SC joint injury. The anatomical positioning of the trachea and major vessels from the heart immediately under the thin skin of the neck make ice an inappropriate treatment.
Criteria for Deciding to Transport for Further Medical Examination
Dyspnea, hoarseness, and difficulty swallowing following a collision or fall on an outstretched arm, elbow, or lateral shoulder are indications to transport the patient via ambulance to the nearest emergency department.
Transportation Techniques
Patients with a suspected posterior SC sprain should have supplemental oxygen available delivered via a nasal cannula. Transportation should occur in a recumbent position to facilitate easier respiration. A sling should be placed on the affected arm to relieve any traction of the SC joint from the weight of the upper extremity.
Heat-related emergencies in athletes
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS).
Many heat-related illnesses are possible, ranging from muscular twitches to fainting to exertional heatstroke (EHS). EHS is the only true heat-related life-threatening emergency, and it is the only heat illness discussed here. As the name suggests, EHS is brought about by the combination of exertion (working out), temperature (including air and humidity), and other factors. A person can acclimate to the hot weather if given the time and cautiously increasing the activity duration slowly in the hot environment. Heatstroke is preventable in many aspects, including paying close attention to the weather (air temperature, ambient temperature, humidity, wind, sunshine), the heat and humidity trends in the local area, clothing and equipment worn, work-to-rest ratio, and hydration and food intake.13 Other salient factors include medical conditions, body mass, poor conditioning, medications, prior history of heat illness, and other predispositions that can exacerbate heat illness.14
Incidence and Epidemiology
Although the overall risk of EHS is low, its consequences can be fatal. According to the National Center for Catastrophic Sport Injury Research, 148 deaths have occurred since 1955 (56 since 1996) due to EHS in football.17 Rates are highest across all levels of football (youth, high school, and collegiate) during the preseason and lower during youth practices and high school games.18 Athletics are not alone in EHS injury; the U.S. military forces also have significant data. Fort Benning, Georgia and Fort Bragg, North Carolina led a 14-year study period with over 1,400 heat-related illnesses each, and nearly 3,500 incidents were reported from military bases in North and South Carolina combined (table 15.2).19
Medical Consequences
of Heatstroke
The systemic physiological effects of untreated EHS are many. The rising internal temperature denatures proteins and cellular membranes, causing an inflammatory response.20 As a reaction, the body relocates an aspect of bacteria usually found in the gastrointestinal system, which can promulgate a sepsis reaction systemically, and therefore begins a coagulation reaction throughout organs.20 Aside from death, EHS can elicit multi-organ failure, acute respiratory distress syndrome, and coma. Organ failure can become irreversible and the long-term sequelae catastrophic.
Signs and Symptoms
If the weather is hot or humid, be suspicious of EHS for any athlete who presents with any of these signs of symptoms. The 2 cardinal signs of EHS are a rectal temperature over 105°F (40.5°C) and central nervous system dysfunction, namely, concussion-like behaviors.21 Strictly from an observational standpoint, the athlete may be disoriented, confused, or dizzy, and his performance may be deteriorating. EHS patients tend to have diaphoretic and hot skin. The presence or absence of sweat should not be a deterrent to consider EHS, given other feedback. Complaints of muscular cramping, headache, weakness, or dry mouth are worth continued exploration. Nausea, vomiting, or diarrhea can occur prior to
collapse.14,20-23
Sudden collapse, seizure, altered consciousness, or coma can occur and will likely transpire if not rapidly diagnosed and treated.21,22 Vital signs can diminish with time, especially if the patient is untreated.
Field Assessment Techniques
A person who has heatstroke presents with concussion-like symptoms, which include confusion, stupor, dizziness, personality changes, and acting combative or complacent. A rapid decision must be made to assess core temperature using a rectal thermometer to diagnose EHS (figure 15.1). Every minute delay to diagnose EHS via rectal thermometry is critical.
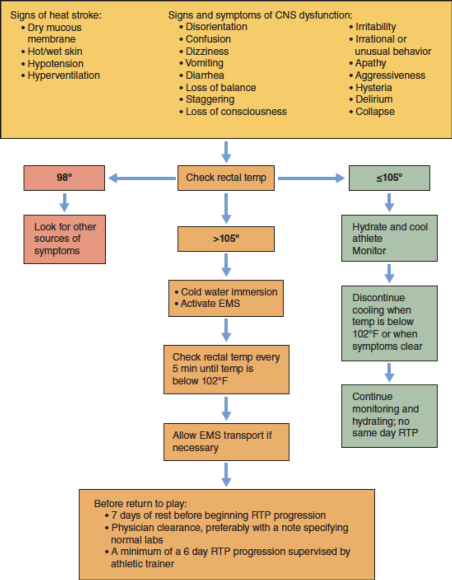
Figure 15.1 Decision tree for EHS.
Safe helmet removal after spinal injury
If the decision has been made to remove the athlete’s equipment, the helmet and shoulder pads should be considered a unit and both be removed.
If the decision has been made to remove the athlete's equipment, the helmet and shoulder pads should be considered a unit and both be removed. Once the face mask has been removed, the helmet can be removed from the injured patient. Less motion in the cervical spine is generated when the face mask is removed from the football helmet prior to removing the helmet.95 Removal of the face mask allows for easier access to stabilize the cervical spine. However, circumstances may arise where the face mask cannot be removed. The sports medicine team should be prepared to remove the helmet under both conditions. Figures 9.24 and 9.25 demonstrate helmet removal with the face mask off and on, respectively. When working with lacrosse, hockey, or other types of helmets, different considerations may need to be made.96-98If time is of the essence, consider leaving the face mask on and simply removing the helmet with the face mask attached.

Figure 9.24 Helmet removal with no face mask.
Courtesy of University of Georgia.

Figure 9.25 Helmet removal with face mask.
Courtesy of University of Georgia.
Here are some tips for helmet removal:
- The chin strap should be cut away, because unsnapping the helmet may create unnecessary movement.
- Cheek pads should be removed from the helmet using a tongue depressor (or something similar) to snap the pad away from the inside of the helmet. However, the ability to remove the cheek pads varies based on the model of the helmet.
- If possible, air bladders in the helmet should be deflated to loosen the fit on the helmet on the patient's head.
- Before the removing the helmet:
- Manual inline stabilization should be transferred from the rescuer at the patient's head (rescuer 1) to rescuer 2, who can provide inline stabilization from the front of the patient.
- Rescuer 2 places 1 hand on the chin and the other hand on the posterior side of the patient's neck (or as depicted in figure 9.26, on either side of the patient's head).
- Rescuer 1, located at the head, grasps the side of the helmet while slightly spreading the cheek pad area on the helmet.
- Rescuer 1 then rotates the helmet forward while sliding the helmet off the patient's head, being mindful to not place the head into flexion or extension.
- Once the helmet is removed, manual inline stabilization should be returned to rescuer 1 and padding (such as a folded towel) should be placed under the patient's head.8 This padding will offset the height of the shoulder pads and prevent hyperextension, which can decrease space available for the cord.
- ATs and other rescue personnel should practice helmet removal with all types of helmets used at their venue.

Figure 9.26 Helmet removal: baseball catcher.
Courtesy of University of Georgia.
Traumatic injuries to the head and face: Subdural hematoma
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.
Subdural hematomas are the leading cause of sports-related fatalities and are frequently reported in football.2 Bleeding collects under the inner layer of the dura mater but external to the brain and arachnoid membrane. Subdural hematomas can become life-threatening very quickly.
Incidence and Epidemiology
A subdural hematoma results most often from a severe head injury. Acceleration-deceleration forces cause injuries as the patient's momentum is stopped suddenly by a solid object and the brain makes contact with the inside of the skull.2 Subdural hematomas can present either acutely or chronically based on the time since symptoms first appeared. Acute subdural hematomas occur within 72 hours after injury, while chronic subdural hematomas may take as long 3 weeks to show signs.
Risk Factors
Risk factors associated with acute subdural hematoma include head trauma, postsurgical complications, anticoagulation drug therapy, and nontraumatic cerebral aneurysm. As with epidural hematomas, decreased risk is associated with appropriate use of protective headgear in athletic environments.
Signs and Symptoms
Immediate medical referral and emergency management are recommended for any of the signs presented in the Red Flag box. Subsequent impacts to the head during the development of a chronic subdural hematoma may put patients at a higher risk of experiencing a life-threatening situation; as such, continued monitoring and serial assessment is important.
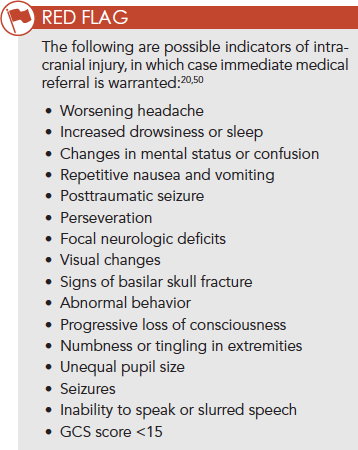
Field Assessment Techniques
In the pre-competition season, athletes participating in at-risk sports (e.g., football, soccer, rugby) should undergo baseline neurocognitive testing, either as a component of a pre-participation physical exam or an adjunct to such an exam. The importance of an established emergency care plan (ECP) cannot be overemphasized; the ECP provides for a standard of care and ensures rapid and efficient treatment measures are in place.
The Canadian CT Head Rule is a clinical prediction rule that uses CT scans to identify head injuries that could require neurosurgical intervention.55 Inclusion criteria include patients with a GCS score of 13 to 15; injury within 24 hours; and blunt head trauma resulting in loss of consciousness, definite amnesia, or disorientation. Exclusion criteria include patients under 16 years of age, nontraumatic cases, patients using anticoagulants or with a bleeding disorder, obvious skull fracture, GCS score of less than 13, and pregnancy.
Immediate Management Techniques
Emergency management of any sports-related injury should first address a primary survey assessment of the patient's mental status, followed by ensuring proper ABC. Knowledge of the patient's neurocognitive baseline may be critical for both short-term and long-term management, and it is helpful when conducting a sideline assessment. Although uncommon, possible differential diagnoses should include intracranial hemorrhage, because the signs and symptoms of a concussion and an intracranial injury are differentiated.50,56 Incorporating potential clinical signs of intracranial injury into the assessment of a patient with a suspected concussion is important.50 Injuries to the head can escalate into medical emergencies quickly, therefore an efficient process of providing immediate care based on signs and symptoms is required (figure 8.6).

Figure 8.6 Head injury algorithm.